Spontaneous abortion (Miscarriage)
Definition:
Spontaneous abortion, commonly known as a miscarriage, is the unintentional loss of a pregnancy before the 20th week.
Abortion is the expulsion or extraction from its mother of an embryo or fetus weighing 500 g or less when it is not capable of independent survival (WHO). This 500 g of foetal development is attained approximately at 22 weeks (154 days) of gestation. The expelled embryo or fetus is called abortus. The word miscarriage is the recommended terminology for spontaneous abortion.
Some synonyms for spontaneous abortion include:
- Miscarriage: This is the most common term used to describe the spontaneous loss of a pregnancy.
- Early pregnancy loss: This term is often used to describe a miscarriage that occurs in the first trimester.
- Spontaneous pregnancy loss: This is a more medical term for miscarriage.
- Fetal demise: This term is used to describe the death of a fetus before birth.
It is important to note that miscarriage is a common occurrence, and most women who experience a miscarriage go on to have healthy pregnancies in the future.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Spontaneous abortion (Miscarriage)
INCIDENCE: The incidence of abortion is difficult to work out but probably 10–20% of all clinical pregnancies end in miscarriage and another optimistic figure of 10% are induced or deliberate.
About 75% miscarriages occur before the 16th week and of these about 80% occur before the 12th week of pregnancy.[1]
Epidemiology
Epidemiology:
Prevalence: The overall prevalence of spontaneous abortion is estimated to be between 10% and 15% of all pregnancies.
Risk Factors: Several factors increase the risk of spontaneous abortion, including advanced maternal age, previous miscarriages, certain medical conditions (such as diabetes and thyroid disorders), and exposure to environmental toxins.
Regional Variations: Studies have shown that the prevalence of spontaneous abortion can vary significantly across different regions of India, possibly due to differences in socioeconomic factors, access to healthcare, and environmental exposures.
Kaur A, Gupta P, Kaur R. Epidemiology of spontaneous abortion. Indian J Community Med.[5]
Causes
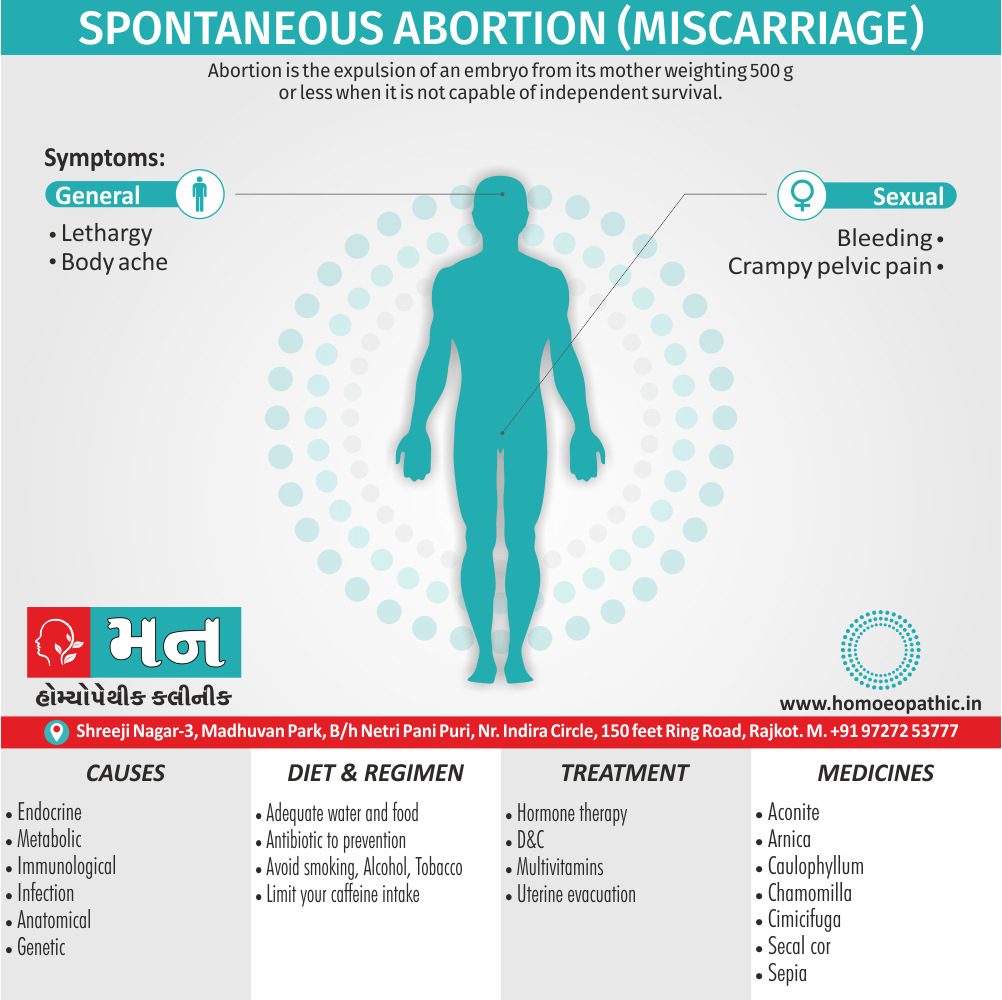
Causes of Spontaneous abortion (Miscarriage)
The etiology of miscarriage is often complex and obscure. The following factors (embryonic or parental) are important:
- Genetic
- Endocrine and metabolic
- Anatomic
- Infection
- Immunological
- Thrombophilia
- Environmental
- Others
- Unexplained
Genetic factors:
- Majority (50%) of early miscarriages are due to chromosomal abnormality in the conceptus.
- Autosomal trisomy is the commonest cytogenetic abnormality. Trisomy for every chromosome has reported. T
- he most common trisomy is trisomy 16. Polyploidy has observed in about 22% of abort uses.
- Monosomy X (45, X) is the single most common chromosomal abnormality in miscarriages.
- Structural chromosomal rearrangements observed in 2–4% of abort uses. These include translocation, deletion, inversion and ring formation.
- Other chromosomal abnormalities like mosaic, double trisomy, etc. found in about 4% of abort uses.[1]
Endocrine & Metabolic factors:
- Luteal Phase Defect (LPD) results in early miscarriage as implantation and placentation are not supporting adequately.
- Deficient progesterone secretion from corpus luteum or poor endometrial response to progesterone is the cause.
- Thyroid abnormalities: Overt hypothyroidism or hyperthyroidism associate with increased foetal loss. Thyroid auto-antibodies often increase.
- Diabetes mellitus when poorly controlled causes increased miscarriage.
- Cervico–uterine factors: These relate mostly to the second trimester abortions.
(1) Cervical ANATOMICAL ABNORMALITIES incompetence, either congenital or acquired is one of the commonest causes of midtrimester and recurrent abortion.
(2) Congenital malformation of the uterus in the form of bicornuate or septate uterus may be responsible for midtrimester recurrent miscarriages. Causes of foetal loss are: (i) reduced intra-uterine volume, (ii) reduced expansile property of the uterus, (iii) reduced placental vascularity when implanted on the septum and (iv) increased uterine irritability and contractility.
(3) Uterine (fibroid) especially of the submucous variety might be responsible not only for infertility but also for abortion. This is due to distortion or partial obliteration of the uterine cavity. Other causes are: decreased vascularity at the implantation site, red degeneration of fibroid and increased uterine irritability.
(4) Intrauterine adhesions interfere with implantation, placentation and foetal growth. Depending on the severity of adhesions, corporal or cervicoisthmic, patient suffers from amenorrhea, hypomenorrhea, infertility or recurrent abortion.
Infection
- The accepted causes of late as well as early abortions. Transplacental foetal infections occur with most microorganisms and foetal losses could be caused by any.
- Infections could be—(i) Viral: Rubella, cytomegalovirus, variola, vaccinia or HIV. (ii) Parasitic: Toxoplasma, malaria. (iii) Bacterial: Urea plasma, chlamydia, Brucella. Spirochetes hardly cause abortion before 20th week because of effective thickness of placental barrier.
Immunological disorders
- Antiphospholipid antibody syndrome (APAS) is due to the presence of antiphospholipid antibodies.
- These are: lupus anticoagulant (LAC), anticardiolipin antibodies (ACAs) and b-glycoprotein 1 antibodies (b-GP1).
- Mechanisms of pregnancy loss in women with APAS are:
(a) Inhibition of trophoblast function and differentiation
(b) Activation of complement pathway
(c) Release of local inflammatory mediators
(d) Thrombosis of uteroplacental vascular bed. Ultimate pathology is foetal hypoxia.
Autoimmunity
- Natural killer cells present in peripheral blood and that in the uterus are different functionally.
- There is no relationship between uNK cell number and future pregnancy outcome though uNK cells help trophoblast invasion, proliferation and angiogenesis.
- Human leukocyte antigen (HLA) incompatibility between couples or absence of maternal blocking antibodies is not considered as the cause of recurrent miscarriage. [1]
Maternal medical illness
- Cyanotic heart disease, hemoglobinopathies are associated with early miscarriage.
- PREMATURE RUPTURE OF THE MEMBRANES inevitably leads to abortion. Paternal factors: Sperm chromosomal anomaly (translocation) can cause miscarriage.
- Some women who miscarry recurrently may have normal pregnancies following marriage with a different man.
- Thrombophilia: Inherited thrombophilia causes both early and late miscarriages due to intravascular coagulation and thrombosis.
- Protein C resistance is the most common cause. Other conditions are: Protein C deficiency and hyperhomocysteinemia antithrombin III or prothrombin gene mutation.
Environmental factors
- Conclusions relating to environmental factors are difficult to establish.
- Cigarette smoking—increases the risk due to formation of carboxyhemoglobin and decreased oxygen transfer to the fetus.
- Alcohol consumption should be avoided or minimized during pregnancy.
- X-irradiation and antineoplastic drugs are known to cause abortion.
- X-ray exposure up to 10 rad is of little risk.
- Contraceptive agents—IUD in situ increases the risk whereas oral pills do not.
- Drugs, chemicals, noxious agents—aesthetic gases, arsenic, aniline, lead, formaldehyde increase the risk.
- Miscellaneous—Exposure to electromagnetic radiation from video display terminals does not increase the risk.
- Women can use hair dyes, watch television and fly in airlines during pregnancy.[1]
Unexplained
- In spite of the numerous factors mentioned, it is indeed difficult, in the majority, to pinpoint the exact cause of miscarriage.
- Too often, more than one factor is present.
- However, risk of abortion increases with increased maternal age.
- About 22% of all pregnancies detected by urinary hCG (peri-implantation) are lost, before the clinical diagnosis.
COMMON CAUSES OF MISCARRIAGE:
First trimester
(1) Genetic factors (50%).
(2) Endocrine disorders (e.g. LPD, thyroid abnormalities, diabetes).
(3) Immunological disorders
(4) Infection.
(5) Unexplained.
Second trimester
(1) Anatomic abnormalities i.e.
(a) Cervical incompetence (either congenital or acquired).
(b) Müllerian fusion defects (bicornuate uterus, septate
uterus).
(c) Uterine synechiae
(d) Uterine fibroid
(2) Maternal medical illness
(3) Unexplained
Types
Classification of Spontaneous abortion (Miscarriage)
Abortion is classified in to two parts i.e.
- Firstly, Spontaneous Abortion
- Secondly, Induced Abortion
Spontaneous Abortion is classified in to
A] Isolated Abortion i.e.
- Threatened
- Inevitable
- Complete
- Incomplete
- Missed
- Septic
B] Recurrent Abortion
Induced Abortion classified in to:
A] Legal (MTP) Abortion
- Unsafe
B] Illegal Abortion
Risk Factors
Risk factors :
Maternal Age: Advanced maternal age (over 35 years) is a well-established risk factor.
Prior Pregnancy Loss: A history of previous miscarriages increases the risk of subsequent losses.
Chromosomal Abnormalities: The majority of early miscarriages are attributed to chromosomal abnormalities in the developing embryo.
Uterine Abnormalities: Structural issues with the uterus, such as fibroids or congenital anomalies, can elevate the risk.
Medical Conditions: Certain medical conditions, including diabetes, thyroid disorders, and autoimmune diseases, can predispose to miscarriage.
Infections: Some infections, particularly those affecting the reproductive system, can increase the risk.
Environmental Exposures: Exposure to certain environmental toxins may also play a role.[6]
Pathogenesis
Pathogenesis :
The pathogenesis of spontaneous abortion is complex and multifactorial. Several factors can contribute to the development of spontaneous abortion, including:
- Chromosomal abnormalities: The most common cause of spontaneous abortion, accounting for approximately 50-70% of cases, particularly in the first trimester.
- Uterine abnormalities: Structural abnormalities of the uterus, such as fibroids or a septate uterus, can increase the risk of spontaneous abortion.
- Infections: Certain infections, such as toxoplasmosis, rubella, and cytomegalovirus, can increase the risk of spontaneous abortion.
- Endocrine abnormalities: Endocrine abnormalities, such as hypothyroidism or uncontrolled diabetes, can increase the risk of spontaneous abortion.
- Immunologic factors: Immunologic factors, such as antiphospholipid syndrome, can increase the risk of spontaneous abortion.
- Environmental factors: Exposure to certain environmental toxins, such as cigarette smoke or heavy metals, can increase the risk of spontaneous abortion.[6]
Pathophysiology
Pathophysiology of Spontaneous abortion (Miscarriage)
- In the early weeks, death of the ovum occurs first, followed by its expulsion.
- In the later weeks, maternal environmental factors are involved leading to expulsion of the fetus which may have signs of life but is too small to survive.
- Before 8 weeks: The ovum, surrounded by the villi with the decidual coverings, is expelled out intact.
- Sometimes, the external os fails to dilate so that the entire mass is accommodated in the dilated cervical canal and is called cervical miscarriage.
- Between 8 weeks and 14 weeks: Expulsion of the fetus commonly occurs leaving behind the placenta and the membranes. Additionally, A part of it may be partially separated with brisk hemorrhage or remains totally attached to the uterine wall.
- Beyond 14th week: The process of expulsion is similar to that of a “mini labour”.
- The fetus is expelled first followed by expulsion of the placenta after a varying interval.[1]
Clinical Features
Clinical Feature:
The clinical features of spontaneous abortion can vary depending on the stage of pregnancy at which it occurs. However, some of the most common symptoms include:
- Vaginal bleeding: This is the most common symptom of spontaneous abortion. The bleeding may be light or heavy, and it may be accompanied by clots.
- Cramping: Cramping is another common symptom of spontaneous abortion. The cramps may be mild or severe, and they may be similar to menstrual cramps.
- Passage of tissue: In some cases, women may pass tissue from the uterus. This tissue may be blood clots, or it may be fetal tissue.[7]
Sign & Symptoms
Sign & Symptoms of Spontaneous abortion (Miscarriage)
- Symptoms of spontaneous abortion include crampy pelvic pain, bleeding, and eventually expulsion of tissue.
- Late spontaneous abortion may begin with a gush of fluid when the membranes rupture.
- Hemorrhage is rarely massive. A dilated cervix indicates that abortion is inevitable.
- If products of conception remain in the uterus after spontaneous abortion, vaginal bleeding may occur, sometimes after a delay of hours to days.
- Infection may also develop, causing fever, pain, and sometimes sepsis.[3]
Clinical Examination
Clinical Examination:
The clinical examination of a patient with suspected spontaneous abortion involves a thorough assessment of her medical history, physical examination, and laboratory investigations.
Medical History
The medical history should include a detailed inquiry into the patient’s:
- Current pregnancy: The date of the last menstrual period, the presence of any pregnancy symptoms, and any abnormal vaginal bleeding or abdominal pain.
- Past obstetric history: Any previous pregnancies, miscarriages, or terminations.
- Gynecological history: Any history of sexually transmitted infections, pelvic inflammatory disease, or abnormal Pap smears.
- Medical history: Any chronic medical conditions, such as diabetes or hypertension, and any medications the patient is currently taking.
- Surgical history: Any previous abdominal or pelvic surgeries.
Physical Examination
The physical examination should include:
- Vital signs: Blood pressure, heart rate, respiratory rate, and temperature.
- Abdominal examination: Inspection, palpation, and percussion of the abdomen to assess for tenderness, masses, or organomegaly.
- Pelvic examination: A speculum examination to visualize the cervix and assess for any bleeding or discharge, and a bimanual examination to assess the size and position of the uterus and ovaries.
Laboratory Investigations
Laboratory investigations may include:
- Blood tests: A complete blood count to assess for anemia, a blood type and Rh factor to assess for Rh incompatibility, and a serum hCG level to confirm pregnancy and assess its viability.
- Urine tests: A urine pregnancy test to confirm pregnancy and a urine culture to assess for infection.
- Ultrasound: An ultrasound scan to visualize the uterus and assess the viability of the pregnancy.[7]
Diagnosis
Diagnosis of Spontaneous abortion (Miscarriage)
- Clinical criteria
- Usually, ultrasonography and quantitative beta subunit of human chorionic gonadotropin (beta-hCG).
- Diagnosis of threatened, inevitable, incomplete, or complete abortion is often possible based on clinical criteria and a positive urine pregnancy test.
- Ultrasonography and quantitative measurement of serum beta-hCG are usually also done to exclude ectopic pregnancy and to determine whether products of conception remain in the uterus (suggesting that abortion is incomplete rather than complete).
- However, results may be inconclusive, particularly during early pregnancy.[3]
- Missed abortion is suspected if the uterus does not progressively enlarge or if quantitative beta-hCG is low for gestational age or does not double within 48 to 72 hours.
- Missed abortion is confirmed if ultrasonography shows any of the following:
- Disappearance of previously detected embryonic cardiac activity
- Absence of such activity when the foetal crown-rump length is > 7 mm
- Absence of a foetal pole (determined by transvaginal ultrasonography) when the mean sac diameter (average of diameters measured in 3 orthogonal planes) is > 25 mm.
- For recurrent pregnancy loss , testing to determine the cause of abortion is necessary.
Differential Diagnosis
Differential Diagnosis:
- Ectopic pregnancy: Implantation outside the uterine cavity, often in the fallopian tube. Presents with abdominal pain, vaginal bleeding, and sometimes an adnexal mass.
- Gestational trophoblastic disease: Abnormal proliferation of trophoblastic tissue, including hydatidiform mole and choriocarcinoma. Presents with vaginal bleeding, often with excessive uterine enlargement and elevated hCG levels.
- Cervical, vaginal, or uterine pathology: Bleeding from lesions such as cervical polyps, cervicitis, or uterine fibroids can mimic spontaneous abortion.
- Implantation bleeding: Light bleeding that can occur around the time of expected menses due to implantation of the embryo into the endometrium.[7]
Complications
Complications :
Potential Complications
- Incomplete abortion: This occurs when some pregnancy tissue remains in the uterus. It can cause bleeding and infection and may require a procedure called dilation and curettage (D&C) to remove the remaining tissue.
- Hemorrhage: Heavy bleeding can occur during or after a miscarriage. It may require blood transfusions or other interventions to control bleeding.
- Infection: The uterus can become infected after a miscarriage, leading to a condition called septic abortion. This is a serious complication that requires prompt treatment with antibiotics.
- Asherman’s syndrome: In rare cases, scar tissue can form in the uterus after a miscarriage or D&C, leading to Asherman’s syndrome. This can cause infertility and other complications.
- Psychological impact: Miscarriage can have a significant emotional impact on both partners, leading to anxiety, depression, and grief.[7]
Investigations
Investigations:
In cases of recurrent spontaneous abortions, a comprehensive investigation is often initiated. This might include:
Chromosomal Analysis: Examining the chromosomes of both parents and the products of conception can identify any genetic abnormalities that may predispose to miscarriage.
Hormonal Assessment: Checking hormone levels, such as thyroid function and progesterone levels, can reveal any imbalances that might interfere with a healthy pregnancy.
Uterine Evaluation: Imaging techniques, such as ultrasound and hysteroscopy, can visualize the uterine cavity to detect any structural abnormalities, such as fibroids or polyps, that might hinder implantation or fetal development.
Infection Screening: Testing for infections, such as toxoplasmosis and cytomegalovirus, can identify any underlying infections that might contribute to miscarriage.
Immunological Testing: Evaluating the immune system’s response to pregnancy can reveal any autoimmune conditions or alloimmune factors that might negatively impact the developing fetus.[8]
Treatment
Treatment of Spontaneous abortion (Miscarriage)
- Observation for threatened abortion
- Uterine evacuation for inevitable, incomplete, or missed abortions
- Emotional support
- For inevitable, incomplete, or missed abortions, treatment is uterine evacuation or waiting for spontaneous passage of the products of conception. [3]
- Evacuation usually involves suction curettage at < 12 weeks, dilation and evacuation at 12 to 23 weeks, or medical induction at > 16 to 23 weeks (e.g., with misoprostol). The later the uterus evacuate, the greater the likelihood of placental bleeding, uterine perforation by long bones of the fetus, and difficulty dilating the cervix.
- These complications reduce by preoperative use of osmotic cervical dilators, misoprostol, or mifepristone.
- If complete abortion suspect, uterine evacuation need not done routinely. Additionally, Uterine evacuation can done if bleeding occurs and/or if other signs indicate that products of conception may be retained.
- After an either induced or spontaneous abortion, parents may feel grief and guilt. In detail, They should give emotional. [3]
- Spontaneous abortion probably occurs in about 10 to 15% of pregnancies.
- The cause of an isolated spontaneous abortion is usually unknown.
- A dilated cervix means that abortion is inevitable.
- Confirm spontaneous abortion and determine its type based on clinical criteria, ultrasonography, also quantitative beta-hCG.
- Uterine evacuation is eventually necessary for inevitable, incomplete, or missed abortions.
- Often, uterine evacuation is not needed for threatened also complete abortions.
- After spontaneous abortion, provide emotional support to the parents.[3]
Prevention
Prevention:
Lifestyle Modifications:
- Maintain a healthy weight: Being Higherweight or underweight can increase the risk of miscarriage. Aim for a healthy BMI before trying to conceive.
- Eat a balanced diet: A diet rich in fruits, vegetables, and whole grains provides essential nutrients for a healthy pregnancy.
- Avoid alcohol and tobacco: These substances can harm the developing fetus and increase the risk of miscarriage.
- Manage stress: Chronic stress can negatively impact pregnancy. Find healthy ways to manage stress, such as exercise, yoga, or meditation.
- Get enough sleep: Aim for 7-8 hours of sleep per night to support your overall health and well-being.
Medical Management:
- Control chronic conditions: If you have any chronic health conditions, such as diabetes or thyroid problems, ensure they are well-managed before and during pregnancy.
- Take prenatal vitamins: Prenatal vitamins provide essential nutrients, including folic acid, which can help prevent certain birth defects and potentially reduce the risk of miscarriage.
- Consult your doctor: If you have a history of miscarriages or other pregnancy complications, discuss your concerns with your doctor. They can provide personalized guidance and recommend any necessary interventions.[9]
Homeopathic Treatment
Homeopathic Treatment of Spontaneous abortion (Miscarriage)
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Spontaneous abortion (Miscarriage):
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Aconite nep
- Impending abortion either from anger or fright, fear that something terrible will happen to her.
- Dizzy especially on rising from a recumbent position, afraid to turn over, to move or to leave the bed.
Alteris
- Habitual tendency to abortion in feeble persons of lax fibre and anemic condition, even after hemorrhage has set in.
- Furthermore, Weight in uterine region, tendency to prolapses uteri.
- General weakness of mind also body.
- Weak either from long sickness or defective nutrition.
Ambra
- Threatening abortion, with tendency to convulsions, specifically in excitable women.[2]
Apis Mell
- Stinging pains in one or the other ovarian region, more and more frequent.
- All labour- pains are produced, sometimes flowing also finally abortus.
- Urine scanty, no thirst.
- Prolonged also difficult constipation.
- Miscarriage especially in third and fourth month; with profuse flow.
Arnica
- Abortus in consequence of a shock, injury.
- Particularly if she commences to flow, either with or without pain, or to have pains without flowing.
- A bruised feeling all over, so that it hurts her to move.
- Where the period of quickening has passed the motion of foetus hurts her.
Asarum
- Threatened abortion from excessive sensibility of all the nerves.
- From even imagining something unpleasant might happen to her, a disagreeable sensation is felt, momentarily arresting all her thoughts also functions.
Belladonna
- Threatened miscarriage with profuse hot hemorrhage.
- Backache, headache also the peculiar uterine tenesmus of the remedy .
- Violent aching of the body. Additionally, the least jar is painful.
Cimicifuga
- One of our most powerful retainers of abortion.
- The pains indication the threatened miscarriage flies across the abdomen from side to side doubling the patient up.
- It suits habitual abortion especially in women of a rheumatic diathesis.
Calcarea carb
- Leuco phlegm Asia, disposition to hemorrhages.
- Cold and damp feet, vertigo; additionally disposition to leucorrhoea.
- Painful nipples.
- Colic, pain in loins; In detail, varices of sexual organs.[2]
Cinamonum
- Useful for abortion from a strain or misstep with profuse hemorrhage also slight pain.
Caulophyllum
- A very useful remedy in false labour pains also also as a preventive of abortion.
- There is severe pain in the back and sides of the abdomen, feeble uterine contractions and scanty flow.
- Severe pains in back and loins; threatening abortion.
- Besides this, Great want of uterine tonicity; uterine contractions tormenting, irregular, feeble and attended with only slight loss of blood, menstrual irregularities after miscarriage.
- Habitual abortion from debility with passive hemorrhage.
Carbo-Veg
- Menses too pale and scanty, or too copious and premature, with varicose condition of sexual organs.
- Frequent headache, abdominal spasms.[2]
Sabina
- This is a remedy useful to prevent impending abortion occurring about the third month, ushered in by the appearance of blood, which is oftentimes the first symptom.
- Then follow pain in the small of the back, going around and through the pubes; there are forcing and dragging pains from the sacrum to the pubes.
- The flow is bright red and clotted.
- It is useful for metritis accompanied especially by flooding from miscarriage.
Secale core
- For miscarriage in the early months of pregnancy Secale may be the remedy, especially in feeble and cachectic women.
- It is useful for checking the tendency to miscarriage in the later months, when the muscular tissue of the womb largely develop.
- It indicated by frequent labour-like pains, a copious hemorrhage of black fluid blood, a wan sunken countenance, tingling and formication of the extremities and a desire for air.
Viburnum Oppulus
- Threatening miscarriage when the pains come from the back around to the lower part of the abdomen and go into the thighs.
- It will often stop these spasmodic pains.
- It is a remedy to use in frequent and early miscarriages.
Sepia
- It is one of our most important remedies as a preventive of miscarriage.
- It indicate by nervous irritability, laxness of tissues and a sense of weight in the anus.[2]
Diet & Regimen
Diet & Regimen of Spontaneous abortion (Miscarriage)
Often, there’s nothing you can do to prevent a miscarriage. Simply focus on taking good care of yourself and your baby:
- Seek regular prenatal care.
- Avoid known miscarriage risk factors — such as smoking, drinking alcohol and illicit drug use.
- Take a daily multivitamin.
- Limit your caffeine intake. A recent study found that drinking more than two caffeinated beverages a day appeared to be associated with a higher risk of miscarriage.[4]
Do’s and Don'ts
Do’s and Don’ts of Spontaneous Abortion:
Experiencing a spontaneous abortion, or miscarriage, can be an emotionally challenging time. Here are some essential do’s and don’ts to help guide you through this difficult period:
Do’s:
- Seek medical attention: If you suspect a miscarriage, consult your healthcare provider immediately. They can confirm the diagnosis and provide necessary care and guidance.
- Allow yourself to grieve: Miscarriage is a significant loss, and it’s essential to acknowledge your feelings and allow yourself to grieve. Don’t rush the healing process.
- Seek emotional support: Talk to your partner, family, friends, or a therapist about how you’re feeling. Sharing your emotions can be incredibly helpful during this time.
- Rest and take care of yourself: Your body needs time to heal, both physically and emotionally. Rest as much as you need, eat nutritious foods, and avoid strenuous activities.
- Follow your healthcare provider’s advice: They may provide specific instructions on how to manage any bleeding or discomfort and when you can resume normal activities.
- Consider joining a support group: Connecting with others who have experienced a miscarriage can provide comfort and understanding.
- Give yourself time to heal: Everyone heals at their own pace. Be patient with yourself and allow yourself the time you need to recover.
Don’ts:
- Blame yourself: Miscarriage is rarely caused by anything you did or didn’t do. It’s a natural occurrence, and you shouldn’t feel responsible.
- Isolate yourself: Don’t withdraw from your support system. Talking to loved ones can help you process your emotions and feel less alone.
- Rush into trying to conceive again: Give your body and mind time to recover before trying again. Talk to your doctor about when it’s safe to try again.
- Ignore your emotions: Don’t try to suppress your feelings or pretend that everything is okay. Acknowledging your emotions is an important part of the healing process.
- Compare your experience to others: Every miscarriage is different, and everyone experiences it in their own way. Don’t compare your journey to others.
Terminology
Terminology:
- Spontaneous Abortion: The medical term for the natural loss of a pregnancy before 20 weeks of gestation.
- Miscarriage: A more commonly used and less clinical term for spontaneous abortion, often preferred by patients.
- Intrauterine Pregnancy Loss: A newer, more neutral term used to describe the loss of a pregnancy within the uterus.
- Early Pregnancy Loss: A general term referring to pregnancy loss that occurs in the first trimester.
- Stillbirth: The loss of a pregnancy after 20 weeks of gestation.
- Complete Abortion: All products of conception (tissue) are expelled from the uterus.
- Incomplete Abortion: Only some products of conception are expelled, and some remain in the uterus.
- Inevitable Abortion: Symptoms cannot be stopped, and a miscarriage will happen.
- Threatened Abortion: Vaginal bleeding occurs during pregnancy, but the cervix remains closed, and the pregnancy may continue.
- Missed Abortion: The embryo or fetus has died, but there are no symptoms of miscarriage.
- Recurrent Pregnancy Loss (RPL): Three or more consecutive pregnancy losses.
Here are some common terminologies and their meanings used in homeopathic articles about spontaneous abortion, along with some additional terms specific to homeopathy:
General Terms:
- Spontaneous Abortion: The natural loss of a pregnancy before 20 weeks of gestation.
- Miscarriage: A more commonly used and less clinical term for spontaneous abortion.
- Early Pregnancy Loss: Refers to pregnancy loss that occurs in the first trimester.
- Recurrent Pregnancy Loss (RPL): Three or more consecutive pregnancy losses.
Homeopathic-Specific Terms:
- Remedy: A substance used in homeopathy to stimulate the body’s healing response.
- Potency: The strength or dilution of a homeopathic remedy.
- Repertorization: The process of matching a patient’s symptoms to the most appropriate homeopathic remedies.
- Constitutional Remedy: A remedy chosen based on the patient’s overall physical and emotional characteristics, rather than just specific symptoms.
- Miasm: A theoretical concept in homeopathy referring to an inherited predisposition to certain diseases or patterns of illness.
Other Relevant Terms:
- Vital Force: The innate healing energy of the body, according to homeopathic philosophy.
- Law of Similars: The principle that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
- Individualization: The process of tailoring homeopathic treatment to the unique characteristics of each patient.
Examples of usage in a homeopathic article:
- "The homeopathic remedy Sepia is often indicated for women experiencing recurrent miscarriages with a history of hormonal imbalances."
- "A constitutional approach to treating recurrent pregnancy loss involves identifying the patient’s underlying miasm and prescribing a remedy based on their overall picture."
- "Homeopathic remedies may be helpful in supporting the vital force after a miscarriage and promoting emotional healing."
It’s important to note
- Consult with both a qualified healthcare professional and a registered homeopath for any concerns related to pregnancy or miscarriage.
- Use caution when relying solely on online information.
References
References use for article around Spontaneous abortion (Miscarriage)
- DC Dutta’s Text Book of OBSTETRICS
- Homoeopathic Therapeutics By Lilienthal
- https://www.msdmanuals.com/en-in/professional/gyn ecology-and-obstetrics/abnormalities-of-pregnancy/spontaneous-abortion
- https://www.mayoclinic.org/diseases-conditions/pregnancy-loss-miscarriage/symptoms-causes.
- Kaur A, Gupta P, Kaur R. Epidemiology of spontaneous abortion. Indian J Community Med.
Williams Obstetrics
Edition: 25th Edition.Writers: F. Gary Cunningham, Kenneth J. Leveno, Steven L. Bloom, Jodi S. Dashe, Barbara L. Hoffman, Brian M. Casey, Catherine Y. Spong
- Spontaneous Abortion in Williams Obstetrics, 26th Edition, by Cunningham, F. Gary, et al. (2022)
- Prevention of Spontaneous Abortion in Williams Obstetrics, 26th Edition, by Cunningham, F. Gary, et al. (2022), McGraw Hill Medical.
Also Search As
Also Search As
Specific Search Terms:
Search Engines: Use search engines like Google, DuckDuckGo, etc., with queries such as:
- "homeopathic treatment for spontaneous abortion"
- "homeopathy and miscarriage"
- "homeopathic remedies for pregnancy loss"
- "homeopathic approach to recurrent miscarriage"
Homeopathic Websites and Forums: Explore websites dedicated to homeopathy, like the National Center for Homeopathy or Homeobook. Search within these sites using relevant keywords.
Homeopathic Journals and Publications: Look for articles in online or physical journals focused on homeopathy, such as Homeopathy or The Journal of the American Institute of Homeopathy.
Social Media: Search relevant hashtags on platforms like Twitter or Facebook (e.g., #homeopathymiscarriage, #homeopathictreatment).
Tips for Effective Searching:
Use synonyms: Include terms like "miscarriage" and "early pregnancy loss" in your searches.
Be specific: If looking for a particular remedy or aspect, add those terms (e.g., "homeopathy sepia miscarriage").
Filter results: Use search engine tools to filter by date, language, or type of content.
Check credibility: Assess the source’s reputation and author’s credentials.
Consult a homeopath: Discuss your findings with a qualified homeopath for personalized advice.
There are numerous ways to search for information on spontaneous abortion, using various search terms, resources, and strategies:
Search Terms:
Medical terms: Spontaneous abortion, miscarriage, early pregnancy loss, intrauterine fetal demise, blighted ovum
Lay terms: Pregnancy loss, baby loss, stillbirth (if applicable)
Specific aspects: Causes of miscarriage, symptoms of miscarriage, treatment options, emotional impact, recurrent miscarriage
Resources:
Search engines: Google, DuckDuckGo, Bing, etc.
Medical websites: Mayo Clinic, WebMD, National Institutes of Health, etc.
Patient support organizations: March of Dimes, Share Pregnancy & Infant Loss Support, etc.
Medical journals & databases: PubMed, Google Scholar, etc.
Social media: Relevant hashtags and support groups on platforms like Facebook, Instagram, etc.
Search Strategies:
Vary your search terms: Use a combination of medical and lay terms to get a wider range of results.
Be specific: If you’re looking for information on a particular aspect, include that in your search terms (e.g., "causes of recurrent miscarriage").
Use quotation marks: Enclose phrases in quotation marks to search for exact matches (e.g., "spontaneous abortion treatment").
Use Boolean operators: Combine search terms with AND, OR, and NOT to refine your search (e.g., "miscarriage AND symptoms").
Filter results: Use search engine tools to filter by date, language, or type of content.
Check source credibility: Make sure the information you find comes from reputable sources.
Additional Tips:
Consult with a healthcare professional: If you have any concerns about pregnancy loss or are experiencing symptoms, always consult with a healthcare professional.
Seek emotional support: If you’re struggling with the emotional impact of a miscarriage, reach out to support groups or mental health professionals.
Be mindful of triggering content: Be aware that some search results may contain graphic or emotionally distressing information.
By utilizing these various search terms, resources, and strategies, you can access a wealth of information on spontaneous abortion. Remember to be mindful of your emotional well-being and consult with healthcare professionals for personalized guidance and support.
Frequently Asked Questions (FAQ)
What is Spontaneous abortion?
Abortion is the expulsion or extraction from its mother of an embryo or fetus weighing 500 g or less when it is not capable of independent survival (WHO). This 500 g of foetal development is attained approximately at 22 weeks (154 days) of gestation. The expelled embryo or fetus is called abortus. The word miscarriage is the recommended terminology for spontaneous abortion.
What causes Spontaneous abortion?
Is homeopathy safe during pregnancy?
- Homeopathic remedies are generally considered safe during pregnancy when prescribed by a qualified practitioner. However, it is crucial to inform your healthcare provider about any homeopathic remedies you are taking, especially during pregnancy.
Can spontaneous abortions be prevented?
- In many cases, spontaneous abortions cannot be prevented. However, maintaining a healthy lifestyle, managing chronic health conditions, and avoiding certain risk factors can reduce the risk.
Can homeopathy prevent spontaneous abortion?
- While some homeopathic practitioners believe certain remedies may help support a healthy pregnancy, there is no scientific evidence to definitively prove that homeopathy can prevent spontaneous abortion. It’s essential to consult with a qualified healthcare professional for any concerns related to pregnancy.
What are the symptoms of Spontaneous abortion?
- Crampy pelvic pain, bleeding, and eventually expulsion of tissue.
- Gush of fluid when the membranes rupture
- Hemorrhage is rarely massive
Can homeopathy help with recurrent miscarriages?
- Some people explore homeopathy as a complementary therapy for recurrent miscarriages. While research on this topic is limited, certain homeopathic remedies may be suggested to address underlying imbalances that could contribute to recurrent pregnancy loss. It is important to work with a qualified homeopath and your healthcare provider in such cases.
Can a woman get pregnant again after a spontaneous abortion?
- Yes, most women who experience a miscarriage can go on to have healthy pregnancies in the future.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Spontaneous abortion?
Homeopathic Medicines for Spontaneous abortion
- Alteris
- Ambra
- Arnica
- Belladonna
- Cimicifuga
- Calcarea carb
- Cinamonum
- Caulophyllum
- Sabina
- Secale core
- Viburnum Oppulus
- Sepia
