Tension Headache (TTH)
Definition
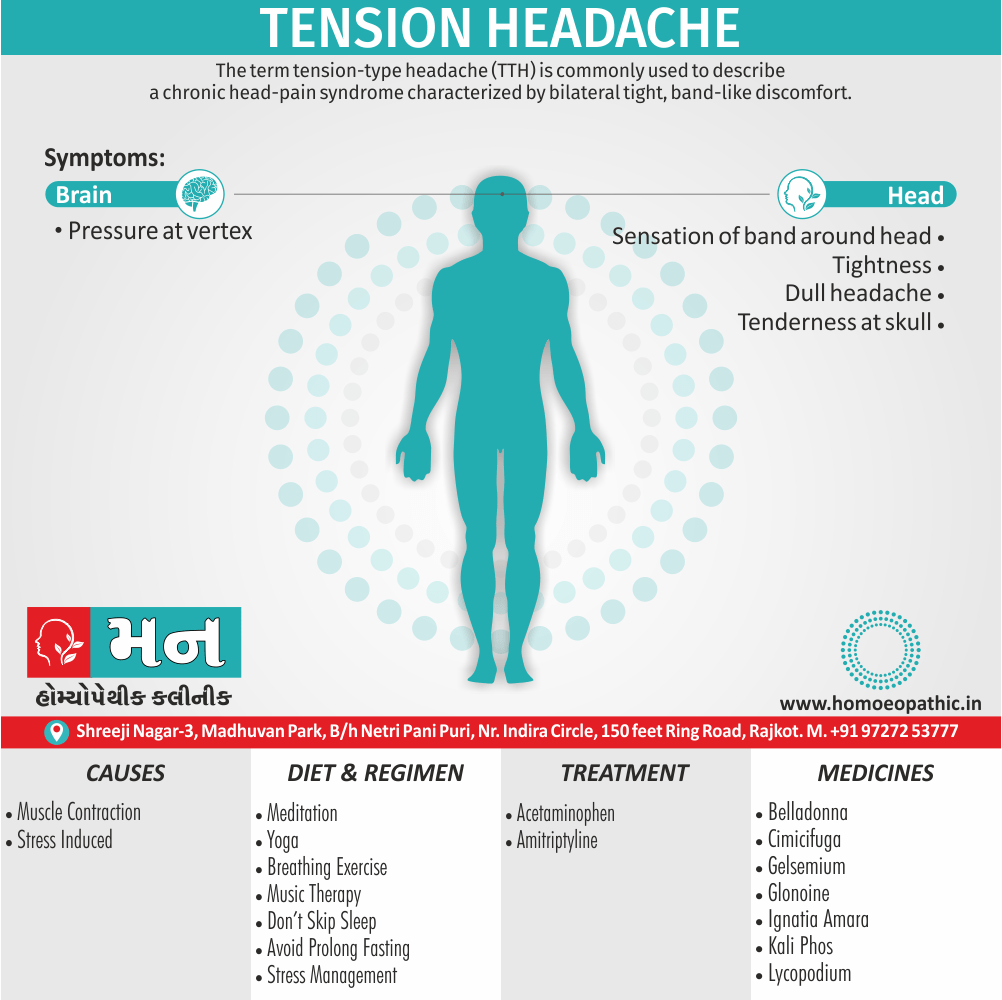
Tension Headache (TTH) is commonly used to describe a chronic head-pain syndrome characterized by bilateral tight, band-like discomfort.[2]
Synonyms for tension headache include:
- Stress headache
- Muscle contraction headache
- Ordinary headache
- Dull headache
- Aching head
- Tight head
- Band-like pressure
Depending on the specific context, you could also use more general terms like:
- Headache
- Head pain
- Cephalalgia (medical term)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do's and Don'ts
Terminology
References
Also Search As
Overview
Overview of Tension Headache
A useful clinical approach is to diagnose TTH in patients whose headaches are completely without accompanying features such as nausea, vomiting, photophobia, phonophobia, osmophobia, throbbing, and aggravation with movement.
Such an approach neatly separates migraine, which has one or more of these features and is the main differential diagnosis, from TTH.
The International Headache Society’s main definition of TTH allows an admixture of nausea, photophobia, or phonophobia in various combinations, although the appendix definition does not; this illustrates the difficulty in distinguishing these two clinical entities.
In clinical practice, dichotomizing patients on the basis of the presence of associated features (migraine) and the absence of associated features (in other words, TTH) is highly recommended.
In deed patients whose headaches fit the TTH phenotype and who have migraine at other times, along with a family history of migraine, migrainous illnesses of childhood, or typical migraine triggers to their migraine attacks, may be biologically different from those who have TTH headache with none of the features.
TTH May be infrequent (episodic) Or occur on 15 days or more a month (chronic).[2]
Nature of Headache:
The pain typically builds slowly, fluctuates in severity, and may persist more or less continuously for many days. The headache may be episodic or chronic (present >15 days per month). [2]
Epidemiology
Epidemiology
The epidemiology of tension-type headache (TTH) in India reveals a significant prevalence, impacting a substantial portion of the population. While specific figures can vary across different studies and regions, the overall picture points to TTH being a common headache disorder within the country.
Key Points:
High Prevalence: Studies indicate that the one-year prevalence of TTH in India ranges from approximately 34% to 35%. This suggests that nearly one-third of the Indian population experiences TTH within a given year.
Female Predominance: Similar to global trends, TTH appears to be more prevalent in females compared to males in India.
Impact on Quality of Life: TTH can significantly affect an individual’s quality of life, leading to reduced productivity, impaired daily functioning, and emotional distress.
Reference:
- Headache prevalence and demographic associations in the Delhi and National Capital Region of India: estimates from a cross-sectional nationwide population-based study (2024) – This study reported a one-year prevalence of 34.1% for TTH in the Delhi and National Capital Region.
Note:
- The prevalence of TTH can vary across different regions and populations within India.
- Further research is needed to explore the specific risk factors, triggers, and effective management strategies for TTH in the Indian context.
Understanding the epidemiology of TTH in India is crucial for developing targeted public health interventions, improving awareness, and enhancing the diagnosis and treatment of this prevalent headache disorder.[7]
Causes
Causes of Tension Headache (TTH):
Primary headaches are not normally due to an underlying medical condition.
Headaches are a physiological disorder and are not a psychological condition.
Research is ongoing to find the causes of tension-type headaches.
According to the National Health Service ( in other words, NHS), possible reasons for a tension-type headache may include i.e.:
- Stress
- Anxiety
- Lack of exercise
- Eyestrain or squinting
- Tiredness
- Missing meals
- Dehydration
- Regular exposure to loud noise
- Bright sunlight
- Poor posture
- Certain smells, such as perfumed products
Stress, anxiety, and depression may trigger jaw clenching, lack of sleep, or lack of exercise which could worsen the problem.[6]
Types
Types
Tension-type headaches are primarily classified into two main types based on their frequency of occurrence:
Episodic Tension-Type Headache:
These headaches occur less frequently, typically fewer than 15 days per month. They can last anywhere from 30 minutes to several days.
Chronic Tension-Type Headache:
This type is characterized by more frequent headaches, occurring on 15 or more days per month for at least three months.
This classification system helps healthcare professionals diagnose and manage tension-type headaches more effectively, tailoring treatment plans to the specific needs of each patient.[8]
Risk Factors
Risk factors
Female sex:
Women are more likely than men to develop tension-type headaches.
Family history of headache:
People with a family history of headache are more likely to develop tension-type headaches.
Stress:
Stress is a major trigger for tension-type headaches.
Anxiety and depression:
People with anxiety and depression are more likely to develop tension-type headaches.
Sleep disturbances:
Sleep disturbances, such as insomnia, can contribute to tension-type headaches.
Poor posture:
Poor posture can put strain on the muscles in the neck and shoulders, leading to tension-type headaches.
Jaw clenching or teeth grinding:
Jaw clenching or teeth grinding (bruxism) can also contribute to tension-type headaches.
Overuse of pain medications:
Overuse of pain medications can lead to rebound headaches, which can mimic tension-type headaches.
Understanding these risk factors can help individuals take steps to prevent or manage tension-type headaches. If you are experiencing frequent or severe headaches, it is important to consult with a healthcare professional to rule out any underlying medical conditions and develop an appropriate treatment plan. [9]
Pathogenesis
Pathogenesis
The exact pathogenesis of tension-type headache remains elusive, however, the prevailing theory centers on peripheral sensitization. This mechanism involves heightened sensitivity of peripheral nociceptors (pain receptors) in the pericranial muscles and connective tissues.
Key points:
- Muscle tenderness: Sustained contraction of pericranial muscles, often triggered by stress or poor posture, is believed to lead to local ischemia and the release of inflammatory mediators.
- Sensitization of nociceptors: These chemical signals sensitize peripheral nociceptors, lowering their activation threshold and amplifying pain signals.
- Central sensitization: In chronic cases, persistent nociceptive input may lead to central sensitization, where the central nervous system becomes more responsive to pain signals, further perpetuating the headache.
Understanding the pathogenesis of tension-type headache aids in developing targeted treatments that address both peripheral and central mechanisms of pain generation.[10]
Pathophysiology
Pathophysiology of Tension Headache (TTH)
- The pathophysiology of TTH incompletely understood.
- It seems likely that TTH is due to a primary disorder of central Nervous system pain modulation alone, unlike migraine, which involves a more generalized disturbance of sensory modulation.
- Data suggest a genetic contribution to TTH, but this may not be a valid finding: given the current diagnostic criteria, the studies undoubtedly included many migraine patients.
- The name tension-type headache implies that pain is a product of nervous tension, but there is no clear evidence for tension as an etiology.
- Muscle Contraction has considered to be a feature that distinguishes TTH from migraine, but there appear to be no differences in contraction between the two headache types.[2]
Clinical Features
Clinical Features
The clinical features of a tension-type headache typically include:
Bilateral location:
The pain is usually felt on both sides of the head.
Pressing or tightening quality:
The pain is often described as a feeling of pressure or tightness, like a band around the head.
Mild or moderate intensity:
The pain is typically mild or moderate in intensity, and it does not usually interfere with daily activities.
No aggravation by routine physical activity:
Unlike migraines, tension-type headaches are not usually made worse by physical activity.
Absence of nausea and vomiting:
Nausea and vomiting are not typically associated with tension-type headaches.
Possible photophobia or phonophobia:
Sensitivity to light (photophobia) or sound (phonophobia) may be present, but it is not as common as in migraines.
It is important to note that the clinical features of tension-type headaches can vary from person to person. If you are experiencing frequent or severe headaches, it is important to consult with a healthcare professional to rule out any underlying medical conditions and develop an appropriate treatment plan.[8]
Sign & Symptoms
Sign & Symptoms of Tension Headache (TTH):
- The pain of tension headache is usually characterized as ‘dull’, ‘tight’ or like a ‘pressure’, and there may be a sensation of a band round the head or pressure at the vertex.
- It is of constant character and generalized, but often radiates forwards from the occipital region.
- In contrast to migraine, the pain can remain unabated for weeks or months without interruption, although the severity may vary, and there is no associated vomiting or photophobia.
- Activities are usually continued throughout, and the pain may be less noticeable when the patient is occupied.
- The pain is usually less severe in the early part of the day, becoming more troublesome as the day goes on.
- Tenderness may be present over the skull vault or in the occiput but is easily distinguished from the triggered pains of trigeminal neuralgia and the exquisite tenderness of temporal arteritis.
- Analgesics may be taken with chronic regularity despite little effect, and may serve to perpetuate the symptoms.[1]
Clinical Examination
Clinical Examination
The clinical examination for tension-type headache focuses on ruling out other headache disorders and identifying any associated musculoskeletal tenderness:
- Neurological Examination: A thorough neurological examination is essential to exclude any secondary causes of headache, including focal neurological deficits, papilledema, or signs of meningeal irritation.
- Palpation of pericranial muscles: Gentle palpation of the scalp, neck, and shoulder muscles may reveal tenderness, particularly in the temporalis, trapezius, and sternocleidomastoid muscles.
- Evaluation of posture and range of motion: Assessing posture and neck range of motion can help identify any musculoskeletal abnormalities that may contribute to the headache.
- Temporomandibular joint (TMJ) assessment: Examining the TMJ for tenderness, clicking, or crepitus can help rule out TMJ disorders as a contributing factor.
It’s important to emphasize that the clinical examination for tension-type headache is largely unremarkable, with the primary focus on excluding other diagnoses. A detailed history and careful neurological assessment are crucial in establishing the diagnosis and guiding appropriate management.[11]
Diagnosis
Diagnosis of Tension Headache (TTH):
The diagnosis of tension-type headache primarily relies on the patient’s clinical presentation and thorough history, following the criteria outlined in the International Classification of Headache Disorders:
- Headache characteristics: The headache should present with the typical features of tension-type headache, including bilateral location, pressing or tightening quality, mild or moderate intensity, and absence of aggravation by routine physical activity.
- Exclusion of other diagnoses: The diagnosis necessitates the exclusion of other headache disorders, especially migraine and cervicogenic headache, through a detailed history and neurological examination.
- Absence of red flags: It is crucial to rule out any secondary causes of headache by assessing for "red flags," such as sudden onset, focal neurological symptoms, or systemic illness.
While no specific diagnostic tests exist for tension-type headache, additional investigations may be warranted in certain cases to rule out other conditions. These may include neuroimaging, blood tests, or referral to a specialist.
Early and accurate diagnosis of tension-type headache is essential for implementing appropriate management strategies and improving the patient’s quality of life.[8]
Differential Diagnosis
Differential Diagnosis
Migraine:
Migraine headaches are often unilateral, pulsating, and associated with nausea, vomiting, and sensitivity to light and sound.
Cervicogenic headache:
Cervicogenic headaches originate from the neck and are often associated with neck pain and limited neck range of motion.
Medication overuse headache:
Medication overuse headache is caused by the frequent use of pain medications, and it can mimic the symptoms of tension-type headache.
Temporomandibular joint (TMJ) disorders:
TMJ disorders can cause pain in the head, face, and neck, which can be mistaken for tension-type headache.
Sinusitis:
Sinusitis can cause pain and pressure in the forehead and cheeks, which can also be confused with tension-type headache.
Secondary headaches:
Secondary headaches are caused by an underlying medical condition, such as a brain tumor, aneurysm, or infection.
A thorough history and neurological examination are crucial in differentiating tension-type headache from other headache disorders. If any red flags are present, further investigations may be warranted to rule out secondary causes of headache.[6]
Complications
Complications
While tension-type headache itself is not typically associated with serious complications, its chronic and recurrent nature can lead to several indirect consequences:
Reduced quality of life:
Frequent or severe headaches can significantly impair daily functioning, affecting work, social activities, and overall well-being.
Increased risk of anxiety and depression:
Chronic pain, including tension-type headache, has been linked to an increased risk of developing anxiety and depression.
Medication overuse headache:
The overuse of pain medications to manage tension-type headache can paradoxically lead to medication overuse headache, a chronic and debilitating condition.
Sleep disturbances:
Tension-type headache can disrupt sleep patterns, leading to insomnia or other sleep problems, which can further exacerbate the headache.
It is important to recognize the potential impact of tension-type headache on various aspects of life and seek appropriate management to minimize these complications. Early diagnosis, effective treatment, and lifestyle modifications can significantly improve the quality of life for individuals with tension-type headache.[9]
Investigations
Investigation of Tension Headache (TTH):
If you have unusual or complicated headaches, your doctor may order tests to rule out serious causes of head pain, such as a tumor. Two common tests that can be used to image your brain include:
- Magnetic resonance imaging (MRI)-An MRI scan combines a magnetic field, radio waves and computer technology to produce clear images.
- Computerized tomography (CT)- A CT scan is a diagnostic imaging procedure that uses a series of computer-directed X-rays to provide a comprehensive view of your brain.[2]
Treatment
Treatment of Tension Headache (TTH):
- The pain of TTH can generally be managed with simple analgesics such as acetaminophen, aspirin, or NSAIDs.
- Behavioral approaches including relaxation can also be effective.
- Clinical studies have demonstrated that triptans in pure TTH are not helpful, although triptans are effective in TTH when the patient also has migraine.
- For chronic TTH, amitriptyline is the only proven treatment; other tricyclics, selective serotonin reuptake inhibitors, and the benzodiazepines have not been shown to be effective.
- There is no evidence for the efficacy of acupuncture.
- Placebo-controlled trials of on a botulinum toxin type A in chronic TTH were negative.[2]
Prevention
Prevention
Stress management:
Implementing stress reduction techniques, such as mindfulness meditation, yoga, or deep breathing exercises, can help prevent headaches triggered by stress.
Regular exercise:
Engaging in regular physical activity promotes overall well-being and can reduce muscle tension, lowering the risk of tension-type headaches.
Good posture:
Maintaining good posture while sitting, standing, and working can help prevent muscle strain and reduce the likelihood of headaches.
Adequate sleep:
Ensuring sufficient and restful sleep is crucial for overall health and can help prevent headaches associated with sleep deprivation.
Healthy diet:
A balanced diet rich in fruits, vegetables, and whole grains can contribute to overall well-being and potentially reduce the frequency of headaches.
Avoiding triggers:
Identifying and avoiding personal triggers, such as certain foods, caffeine, or alcohol, can help prevent headaches.
In addition to these lifestyle modifications, seeking professional help for stress management, anxiety, or depression can further contribute to preventing tension-type headaches. It is also important to consult with a healthcare professional to rule out any underlying medical conditions and discuss appropriate preventive medications if necessary. [12]
Homeopathic Treatment
Homeopathic Treatment of Tension Headache
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Tension Headache:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Kali Phos
- Kali Phos top grade medicine for tension headache triggered by stress, anxiety also emotional disturbances.
- It also works well in case a tension headache link to depression.
- Symptoms like sadness, excessive weeping, weakness, exhaustion, a sensation of a heavyweight in the back of the head also sensitivity to noise indicate the need for Kali Phos.
Cimicifuga Racemosa
- Cimicifuga Racemosa a medicine prepare from the roots of a plant named ‘black cohosh’ of natural order Ranunculaceae.
- It a well indicate homeopathic medicine for a tension headache with contracted neck muscles.
- The pain is present in the entire head also radiates to back of the neck and the shoulders.
- This is attended with soreness of the neck also shoulders.[5]
Gelsemium Sempervirens
- Gelsemium Sempervirens a natural medicine prepare especially from the plant yellow jasmine.
- This plant belongs to family Loganiaceae, also bark of its root is used to make the medicine.
- This medicine use for tension headaches where the person feels as if a band tie tightly across the forehead.
- Along with this, there is a dull pain in the head.
- A sensation of weight, pressure, also heaviness in the head is also present.
- In most cases, pain begins in neck muscles that extend over the entire head.
- Applying pressure also sleeping tends to relieve the headache.
Epiphegus
- Generally, Epiphegus a medicine prepare from the fresh plant named ‘beech drop’ of the order Orobanchaceae.
- It is a prominent medicine to treat a tension headache triggered by overexertion and fatigue.
- A headache appears in the temples of the head.
- Hunger may precede a headache.
- A peculiar feature increase salivation with constant spitting.
- Good sleep may bring relief especially, from the headache.
Glonoinum
- Glonoinum is a beneficial medicine for tension headache triggered by sunlight.
- A headache in the front, back of the head and also behind the ears appears.
- In some cases, there is a pain in the nape of the neck that extends to the top of the head.
- Congestion, heat, and soreness are felt in the head. Lastly, The headache may get better after sleep.
Nux Vomica
- Nux Vomica is a highly recommended medicine for tension headache triggered by alcohol intake.
- The pain appears on the forehead, vertex (top of head) and occiput.
- Mental irritability, scalp sensitivity on touch, also mental strain triggering a tension headache are the main symptoms indicating the need for Nux Vomica.
- This medicine is also suitable for treating tension headache that gets triggered by the intake of coffee.
Ignatia Amara
- Ignatia Amara a suitable medicine for a tension headache trigger by smoking.
- Sometimes smelling tobacco may also trigger a tension headache.
- The pain from the head may extend down the neck.
- This may attend with a tender scalp.
- Stooping may worsen a headache.
- Sleeplessness may also present.
- Ignatia Amara is also recommended for tension headaches associated with depression.
Belladonna
- Belladonna is a natural medicine prepared from a plant named ‘deadly nightshade.’
- The natural order of this plant is Solanaceae.
- It is a very useful medicine for tension headache that develops from cold and Sinusitis.
- Fullness in the head, pain in forehead, back and side of the head, fluent coryza and sneezing are the characteristic symptoms.
- Light and noise may worsen the headache, while pressure tends to relieve the headache.[5]
Lycopodium Clavatum
- Lycopodium Clavatum is a medicine prepared from the plant ‘club moss’ belonging to the family Lycopodiaceae.
- It works well for tension headaches triggered especially by skipping or missing meals.
- Symptoms include a headache in the back of the head also over the eyes.
- Pain from the head may extend down the neck with weakness. Additionally, This is attended with soreness of the scalp.
- It may get better specifically by lying down.
Ruta Graveolens
- Ruta Graveolens a medicine recommended for tension headaches triggered specifically by eye strain.
- It plant-based medicine prepare from the plant ‘garden rue’ belonging to the family Rutaceae.
- Pressure in the forehead, pain in the forehead that extends to the temples, aching eyes, a pressure in the eye orbits, heat in the head, anxiety, also restlessness are the characteristic symptoms that indicate towards this medicine.
Coffea Cruda
- Coffea Cruda a well-indicate medicine for tension headache triggered by noise.
- The head feels tight, and there is a heaviness in the forehead above eyes.
- Motion and light tend to worsen the headache.
- A tension headache that trigger by certain smells also treat with Coffea Cruda.
Carbolic Acid
- Carbolic Acid is a prominent medicine for tension headache attended with scalp tenderness.
- There is a headache with a sensation as if a tight band stretch over the forehead from temple to temple.
- There is fullness in the head with dull aching.
- The scalp is tender to touch, and there may a pain in the neck.[5]
Diet & Regimen
Diet & Regimen
Diet:
Stay hydrated: Dehydration is a common trigger for tension headaches. Aim for 8 glasses of water a day, and consider electrolyte drinks if you’ve been sweating.
Limit trigger foods: Some people find that certain foods trigger their headaches. Common culprits include:
Alcohol: Especially red wine
Caffeine: While it can help some headaches, withdrawal can trigger others.
Processed foods: Those high in nitrates (like hot dogs) or MSG
Aged cheeses:
Artificial sweeteners:
Magnesium-rich foods: Magnesium may help prevent headaches. Good sources include leafy greens, nuts, seeds, and whole grains.
B vitamins: Foods rich in B vitamins, like whole grains, legumes, and eggs, can help support nerve health.
Regimen:
Stress management: Stress is a major contributor to tension headaches. Incorporate relaxation techniques into your routine, such as:
Exercise: Regular physical activity can release endorphins and reduce stress.
Yoga and meditation: These practices can help calm the mind and body.
Deep breathing exercises:
Progressive muscle relaxation:
Sleep hygiene: Aim for 7-9 hours of quality sleep each night. Establish a regular sleep schedule and create a relaxing bedtime routine.
Posture: Poor posture can contribute to muscle tension in the neck and shoulders, leading to headaches. Be mindful of your posture throughout the day.
Heat therapy: Apply a warm compress or take a warm bath to relax tense muscles.
Over-the-counter pain relief: Ibuprofen or acetaminophen can provide temporary
relief.
Do's and Don'ts
Do’s and Don’ts
Tension Headache Do’s & Don’ts
Do’s:
- Manage Stress: Practice relaxation techniques like deep breathing, meditation, or yoga to reduce stress levels, a major trigger for tension headaches.
- Maintain Good Posture: Pay attention to your posture, especially when sitting for extended periods, to avoid muscle tension in the neck and shoulders.
- Get Regular Exercise: Engage in physical activity regularly, as it can help relieve muscle tension and promote overall well-being.
- Prioritize Sleep: Ensure you get adequate and quality sleep each night, as sleep deprivation can trigger headaches.
- Eat Healthy: Maintain a balanced diet with regular meals to avoid fluctuations in blood sugar levels, which can sometimes trigger headaches.
- Stay Hydrated: Drink plenty of water throughout the day to prevent dehydration, a potential headache trigger.
- Apply Heat or Cold: Use a warm compress or take a hot shower to relax tense muscles. Alternatively, apply a cold compress to your forehead or temples for pain relief.
- Over-the-Counter Pain Relief: Consider using over-the-counter pain relievers like ibuprofen or acetaminophen for occasional tension headaches.
Don’ts:
- Don’t Overuse Pain Medications: Avoid relying on pain medications too frequently, as this can lead to rebound headaches.
- Avoid Caffeine and Alcohol: Limit or avoid caffeine and alcohol consumption, as they can trigger or worsen headaches.
- Don’t Skip Meals: Skipping meals, especially breakfast, can lead to low blood sugar levels, which can trigger headaches.
- Don’t Clench Your Jaw or Grind Your Teeth: Be mindful of jaw clenching or teeth grinding, as these habits can contribute to tension headaches.
- Avoid Triggers: If you identify specific triggers for your headaches, such as certain foods or environmental factors, avoid them.
- Don’t Ignore Chronic Headaches: If you experience frequent or severe tension headaches, consult a doctor to rule out other underlying medical conditions and discuss treatment options.
Remember:
- The above are general recommendations. It’s best to consult with your doctor for personalized advice and treatment plans.
- Lifestyle modifications and stress management techniques are often effective in preventing and managing tension headaches.
- If your headaches are severe, persistent, or accompanied by other symptoms, seek medical attention promptly.
Terminology
Terminology
Here are some key terminologies and their meanings commonly used in articles about tension headaches:
Tension-Type Headache (TTH)
The most common type of primary headache, characterized by a dull, aching pain on both sides of the head, often described as a feeling of pressure or tightness.
Episodic TTH
TTH occurring less than 15 days per month.
Chronic TTH
TTH occurring on 15 or more days per month for at least 3 months.
Primary Headache
A headache that is not caused by another underlying medical condition.
Secondary Headache
A headache caused by another underlying medical condition, such as a brain tumor, infection, or head injury.
Pericranial Muscles
The muscles surrounding the skull, including the temporalis, frontalis, occipitalis, and neck muscles.
Nociceptors
Sensory receptors that detect and transmit pain signals.
Peripheral Sensitization
A process where nociceptors become more sensitive to stimuli, leading to increased pain perception.
Central Sensitization
A process where the central nervous system becomes more responsive to pain signals, leading to increased pain perception and a lowered pain threshold.
Photophobia
Sensitivity to light.
Phonophobia
Sensitivity to sound.
Aura
Sensory disturbances, such as visual changes or tingling, that may precede a migraine headache.
Prodrome: Early symptoms, such as fatigue or mood changes, that may occur before a migraine headache.
Comorbidity: The presence of two or more medical conditions in the same individual.
Analgesics: Pain-relieving medications.
Prophylactic Medications
Medications used to prevent headaches from occurring.
Relaxation Techniques
Methods used to reduce stress and muscle tension, such as meditation, yoga, and deep breathing exercises.
Biofeedback
A technique that helps individuals learn to control bodily functions, such as muscle tension and heart rate, through feedback from monitoring devices.
Understanding these terms will enable you to better comprehend and interpret information presented in articles about tension headaches.
Here are some terminologies and their meanings that are commonly used in homeopathic articles about tension headaches:
Remedy
A homeopathic medicine prepared from natural substances and used to treat specific symptoms and conditions.
Potency
The strength or dilution of a homeopathic remedy.
Proving
A systematic process of observing and recording the symptoms produced by a homeopathic remedy in healthy individuals.
Repertory
A reference book that lists symptoms and the homeopathic remedies associated with them.
Materia Medica
A comprehensive collection of information about the properties and effects of homeopathic remedies.
Constitutional Remedy
A remedy that matches the overall physical, mental, and emotional characteristics of an individual.
Aggravation
A temporary worsening of symptoms after taking a homeopathic remedy, often considered a positive sign of the remedy’s action.
Miasm
A predisposing factor or inherited weakness that influences susceptibility to certain diseases.
Vital Force
The inherent life energy or self-healing mechanism within the body.
Law of Similars
The fundamental principle of homeopathy, which states that "like cures like."
Individualization
The process of selecting the most appropriate homeopathic remedy based on the unique symptoms and characteristics of the individual.
Potentization
The process of diluting and succussing (shaking) a homeopathic remedy to increase its potency.
Succussion
The process of vigorously shaking a homeopathic remedy during its preparation.
Trituration
The process of grinding a solid substance into a fine powder for homeopathic preparation.
Nosode
A homeopathic remedy prepared from diseased tissue or bodily fluids.
Understanding these terminologies will help you to better understand and interpret information presented in homeopathic articles about tension headaches.
References
References use for Tension Headache (TTH):
- https://www.researchgate.net/publication/5754613_Tension-type_headache_Current_research_and_clinical_management
- Harrisons_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- https://www.webmd.com/migraines-headaches/relaxation
- https://www.chiropracticsolutionsspringfield.com/tension-headaches-
- https://www.drhomeo.com/tension-headache/tension-headaches-homeopathic-treatment/
- https://www.medicalnewstoday.com/articles/313020#causes
- Headache prevalence and demographic associations in the Delhi and National Capital Region of India: estimates from a cross-sectional nationwide population-based study (2024).
- The International Classification of Headache Disorders, 3rd edition (beta version) Headache Classification Committee of the International Headache Society ,(2013), Publication: Cephalalgia
- Harrison’s Principles of Internal Medicine, 20th EditionAuthors: Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo, (2018), Publication: McGraw Hill Professional.
- Brainstorm: Secrets of the Brain
Author: Daniel J. Siegel, M.D.
(2013), Publication: Penguin Random House. - Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9th Edition
Authors: Judith E. Tintinalli, J. Stephan Stapczynski, O. John Ma, Donald M. Yealy, Garth D. Meckler, David M. Cline
(2020), Publication: McGraw Hill Professional - Mayo Clinic Family Health Book, 5th Edition Authors: The Mayo Clinic, (2019)
Publication: Mayo Clinic Press
Also Search As
Also Search As
People can search for homeopathic articles on tension headaches using various methods:
Online Search Engines
Use specific keywords:
- "homeopathic remedies tension headache"
- "homeopathy for tension headache"
- "tension headache treatment homeopathy"
- Include additional terms like "natural remedies," "alternative medicine," or "holistic approach."
Explore reputable websites:
- National Center for Homeopathy (NCH)
- Homeopathic Educational Services (HES)
- Homeopathy Plus
- Websites of renowned homeopathic practitioners or organizations
Homeopathic Libraries or Resource Centers
- Visit local homeopathic libraries or clinics: Inquire about resources and articles on tension headaches
- Ask homeopathic practitioners for recommendations: They may have specific articles or journals to suggest
Social Media and Online Forums
- Join homeopathy groups and communities: Ask for article recommendations or share relevant articles you find
- Follow homeopathic practitioners or organizations: They may post links to informative articles
Additional Tips
- Use advanced search operators: Use quotation marks for exact phrases or minus signs to exclude certain terms to refine your search results.
- Pay attention to source credibility: Look for articles from reputable sources and authors with expertise in homeopathy.
- Consult a homeopathic practitioner: They can provide personalized recommendations and information on homeopathic treatment options for tension headaches.
By utilizing a combination of these methods and resources, individuals can find valuable information on homeopathic approaches to managing and treating tension headaches. Remember to critically evaluate any information you find and consult with a qualified homeopathic practitioner for personalized guidance and treatment.
There are numerous ways to search for information on tension headaches, each with its own advantages:
Search Engines
- Google, Bing, etc. – Use keywords like "tension headache," "tension headache symptoms," "tension headache treatment," or "tension headache causes."
- Use specific phrases: To get more targeted results, try phrases like "tension headache vs migraine" or "tension headache home remedies."
Medical Websites & Databases
- Reputable health websites: Mayo Clinic, WebMD, Healthline, etc. These sites often provide detailed information on symptoms, causes, and treatment options.
- Medical databases: PubMed, Google Scholar. These databases contain scholarly articles and research papers on tension headaches.
Social Media
- Hashtags: Search relevant hashtags on platforms like Twitter or Instagram (e.g., #tensionheadache, #headacherelief).
- Support groups: Join online communities or forums to connect with others experiencing tension headaches and share information.
Books and Publications
- Medical textbooks: Look for information in neurology or general medicine textbooks.
- Health magazines: Many health magazines offer articles on common health concerns like tension headaches.
Health Professionals
- Doctor: Consult your doctor for a personalized assessment and treatment plan.
- Pharmacist: Your pharmacist can offer advice on over-the-counter medications for tension headaches.
Remember to consider the reliability of the information source. Look for information from reputable medical organizations and healthcare professionals. If you have any concerns about tension headaches, don’t hesitate to seek professional medical advice.
Frequently Asked Questions (FAQ)
What is Tension Headache?
The term tension-type headache (TTH) is commonly used to describe a chronic head-pain syndrome characterized by bilateral tight, band-like discomfort.
Can tension headaches be prevented?
Yes, tension headaches can often be prevented by managing stress, getting regular exercise, maintaining good posture, and getting enough sleep.
What are the causes of Tension Headache?
- Stress
- Anxiety
- Lack of exercise
- Eyestrain or squinting
- Tiredness
- Missing meals
- Dehydration
- Regular exposure to loud noise
What are the symptoms of Tension Headache?
- Pain- ‘dull’, ‘tight’ or like a ‘pressure’
- Constant character and generalized
- Pain can remain unabated for weeks or months without interruption
Homeopathic Medicines used by Homeopathic Doctors in treatment of Tension Headache?
Homoeopathic medicine for Tension headache
- Kali Phos
- Cimicifuga Racemosa
- Gelsemium
- Glonoinum
- Nux Vomica
- Ignatia Amara
- Belladonna
