Threatened Miscarriage
Definition
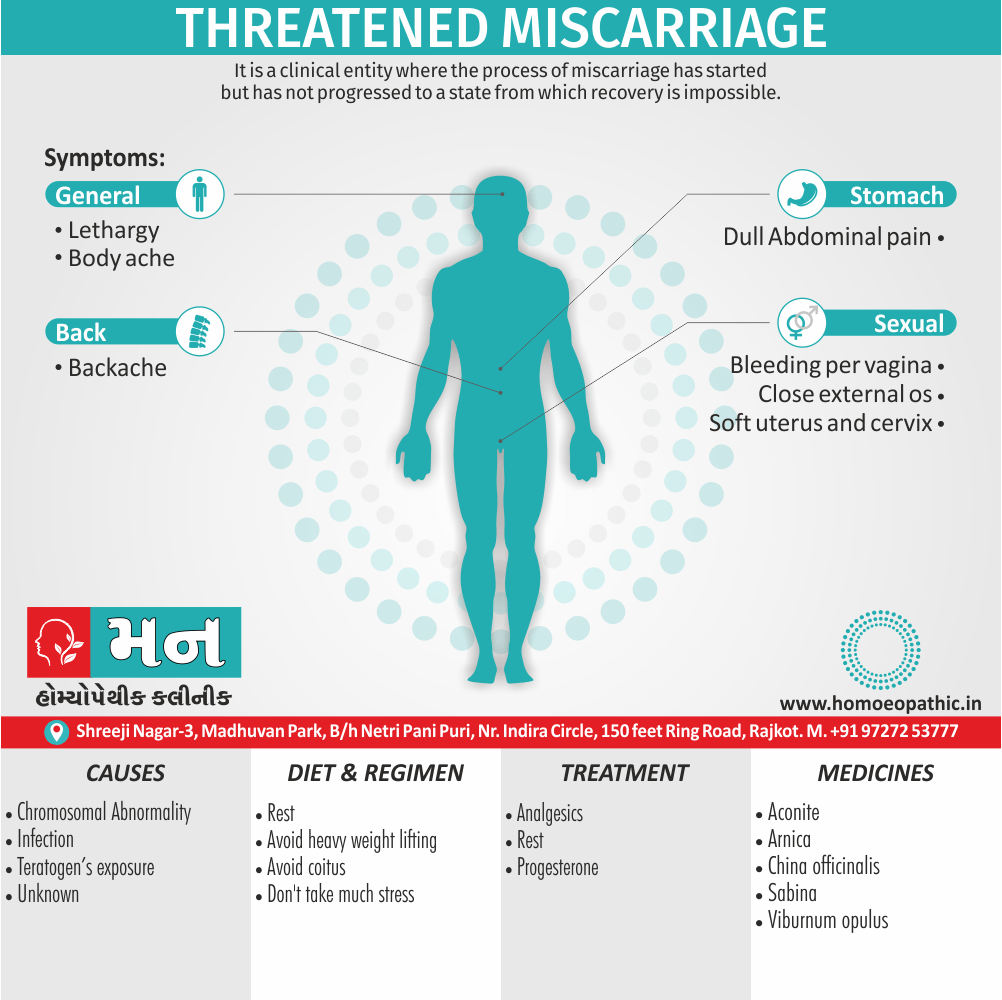
Threatened Miscarriage is a clinical entity where the process of miscarriage has started but has not progressed to a state from which recovery is impossible. [1]
A threatened miscarriage is a condition where vaginal bleeding occurs during the first 20 weeks of pregnancy, potentially indicating a risk of miscarriage. Although it can be alarming, a threatened miscarriage doesn’t always result in the loss of the pregnancy.
There are several related terms and phrases that may be used:
Threatened abortion: This is an older term that was once commonly used, but it is now considered less appropriate due to the negative connotations associated with the word "abortion."
Threatened early pregnancy loss: This term more accurately describes the potential outcome of a threatened miscarriage, as it emphasizes the early stage of pregnancy.
Bleeding in early pregnancy: This is a more general term that can refer to various causes of bleeding during the first trimester, including threatened miscarriage, implantation bleeding, and other conditions.
It is important to note that these terms are not always interchangeable, and the specific terminology used may depend on the context and the individual’s preference. For example, some people may prefer the term "threatened early pregnancy loss" because it is more neutral and less stigmatizing than "threatened abortion."
If you are experiencing any bleeding or other symptoms during pregnancy, it is crucial to consult with your healthcare provider to determine the cause and receive appropriate care.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prognosis
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview:
A threatened miscarriage refers to vaginal bleeding during pregnancy, typically before 20 weeks gestation, with a closed cervix and a viable fetus.
It’s a concerning situation but doesn’t necessarily mean a miscarriage will occur. In fact, most women who experience a threatened miscarriage go on to have healthy pregnancies.[3]
Epidemiology
Epidemiology:
Threatened miscarriage is a common complication in early pregnancy in India.
It has been reported to occur in approximately 14-21% of all pregnancies. The risk of threatened miscarriage increases with advancing maternal age, and in some cases, paternal age. A large study in India observed a significant increase in the incidence of early miscarriage with advanced maternal age, from 10-15% in women aged 20 to 34 years to 51% in women aged 40 to 44 years.[4]
Causes
Causes:
- The exact etiology not always known. It widely accept that the vast majority of spontaneous abortions cannot prevent or modified likely because they are due to chromosomal abnormalities in at least half of all cases.
- For pregnancy losses that determine to have a normal chromosomal makeup, termed euploid abortions, maternal and paternal factors play a more significant role. Optimization of maternal health before pregnancy, correcting structural abnormalities of the uterus, and minimizing exposure to teratogens or infections during early pregnancy can reduce the risks for spontaneous abortion.
- When optimizing maternal health, special consideration should be given to chronic illnesses such as diabetes and thyroid disease, as well as extremes of weight and use of tobacco products, alcohol, or illicit drugs.
Other causes
- Some studies have shown that folic acid supplementation immediately before and during early pregnancy may reduce the risk of spontaneous abortion.
- It has also been shown in several studies that increasing paternal age is associated with increased risk for pregnancy loss, likely due to increased chromosomal abnormalities.
- Women should also educate about reducing the risk of traumatic events and should be screened for risk for intimate partner violence.
- It is reasonable to recommend preconception counseling to modify these risk factors.[1]
Types
Types:
1. Threatened Miscarriage with Subchorionic Hematoma:
- This involves vaginal bleeding in early pregnancy with the presence of a subchorionic hematoma (blood clot) on ultrasound.
- Reference: "Threatened Miscarriage" – StatPearls – NCBI Bookshelf (2023)
2. Threatened Miscarriage with Cervical Insufficiency:
- This presents with bleeding and/or contractions, potentially with a dilated cervix, suggesting a weakened cervix that may lead to miscarriage.
- Reference: "Cervical Insufficiency" – ACOG Practice Bulletin (2013)
3. Threatened Miscarriage with Underlying Chromosomal Abnormalities:
- While not clinically apparent, genetic testing might reveal fetal chromosomal issues increasing the risk of miscarriage.
- Reference: "Chromosomal Abnormalities and Early Pregnancy Loss" – Fertility and Sterility (2012)
4. Asymptomatic Threatened Miscarriage:
- This is a rare scenario where a routine ultrasound identifies a potential issue (e.g., low fetal heart rate) despite the absence of bleeding or pain, warranting close monitoring.[5]
Risk Factors
Risk factors :
- Chromosomal Abnormalities: Genetic problems in the developing fetus are a major cause of early pregnancy loss, including threatened miscarriages.
- Implantation Issues: Difficulties with the embryo attaching securely to the uterine lining can lead to bleeding and a threatened miscarriage.
- Hormonal Imbalances: Inadequate levels of progesterone, a hormone crucial for maintaining pregnancy, can contribute to a threatened miscarriage.
- Uterine Abnormalities: Structural issues with the uterus, such as fibroids or a septum, can interfere with implantation and increase the risk of miscarriage.
- Infections: Certain infections, such as bacterial vaginosis or sexually transmitted infections, have been associated with an increased risk of miscarriage.
- Maternal Health Conditions: Chronic conditions like diabetes, autoimmune diseases, or thyroid problems can affect pregnancy and increase the risk of complications, including threatened miscarriage.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and drug use can harm the developing fetus and contribute to pregnancy loss.
- Advanced Maternal Age: The risk of miscarriage, including threatened miscarriage, increases with maternal age, particularly after age 35.
- Previous Miscarriage: A history of previous miscarriages can increase the risk of experiencing another one.[6]
Pathogenesis
Pathogenesis:
Chromosomal Abnormalities: The most common cause of early pregnancy loss, accounting for around 50-70% of cases. These abnormalities can disrupt the normal development of the embryo or fetus, leading to miscarriage. (American College of Obstetricians and Gynecologists, 2023)
Implantation Defects: Inadequate or abnormal implantation of the embryo into the uterine lining can compromise its access to essential nutrients and oxygen, potentially resulting in miscarriage.
Endocrine Imbalances: Hormonal fluctuations, particularly low levels of progesterone, can destabilize the pregnancy and increase the risk of miscarriage. (Mayo Clinic, 2023)
Infectious and Inflammatory Processes: Infections of the reproductive tract or systemic infections can trigger an inflammatory response, potentially compromising the pregnancy and leading to miscarriage.
Immunological Factors: In some cases, the maternal immune system may mistakenly attack the developing embryo or fetus, contributing to miscarriage.
Uterine Abnormalities: Structural anomalies of the uterus, such as fibroids or congenital malformations, can impede proper implantation and development of the pregnancy, leading to miscarriage.[3]
Pathophysiology
Pathophysiology:
- Compromised Implantation: Aneuploidy can disrupt the intricate process of embryo implantation in the endometrium. Trophoblast cells, responsible for invading the maternal tissue and establishing placental connections, may function abnormally, leading to inadequate placental development.
- Impaired Placental Function: Even if implantation occurs, aneuploidy can hinder the placenta’s ability to perform its critical functions, such as nutrient and oxygen exchange between mother and fetus. This can result in fetal growth restriction or demise.
- Decidual Breakdown: Aneuploidy can also trigger changes in the decidua, the specialized endometrium that supports pregnancy. These changes can lead to premature decidual breakdown and separation of the placenta from the uterus, resulting in bleeding and miscarriage.
Other potential contributors to threatened miscarriage:
- Subchorionic Hemorrhage: Bleeding between the chorion (outermost fetal membrane) and the uterine wall can disrupt placental attachment and trigger uterine contractions, potentially leading to miscarriage.
- Uterine Abnormalities: Structural issues like fibroids or a septate uterus can interfere with implantation and placental development, increasing the risk of miscarriage.
- Endocrine Imbalance: Hormonal fluctuations, particularly low progesterone levels, can compromise the endometrial lining and impact placental function, potentially contributing to miscarriage.
- Immunologic Factors: In some cases, the maternal immune system may misidentify the fetus as foreign and attack it, leading to pregnancy complications and potential miscarriage.
- Infections: Certain infections, particularly those affecting the reproductive tract, can increase the risk of miscarriage.[7]
Clinical Features
Clinical Features:
- Vaginal Bleeding: The hallmark symptom, ranging from light spotting to heavier flow.
- Closed Cervical Os: The cervix remains closed, indicating the pregnancy is still intact.
- First Half of Pregnancy: Typically occurs before 20 weeks gestation.
- Possible Cramping: May or may not experience mild uterine cramping.
Important Considerations:
- Severity of Bleeding: The amount of bleeding does not necessarily correlate with the outcome.
- Pain: While mild cramping may be present, severe pain can indicate a more serious problem.
- Other Symptoms: Nausea, vomiting, or fever may suggest an infection or other complications.
Prompt Evaluation:
Any vaginal bleeding during pregnancy warrants prompt medical evaluation to assess the viability of the pregnancy and identify any underlying causes.[7]
Sign & Symptoms
Sign And Symptoms:
The patient, having symptoms suggestive of pregnancy, complains of i.e.:
(1) Firstly, Bleeding per vaginum is usually slight and may be brownish or bright red in color. On rare occasion, the bleeding may be brisk, especially in the late second trimester. The bleeding usually stops spontaneously.
(2) Secondly, Pain: Bleeding is usually painless but there may be mild backache or dull pain in lower abdomen. Pain appears usually following hemorrhage.
Pelvic examination should be done as gently as possible i.e.-
(a) Speculum examination reveals- Bleeding if any, escapes through the external os. Differential diagnosis includes cervical ectopy, polyps or carcinoma, ectopic pregnancy and molar pregnancy.
(b) Digital examination reveals- The closed external os. The uterine size corresponds to the period of amenorrhea. The uterus also cervix feel soft. Pelvic examination is avoided when ultrasonography is available [1]
Clinical Examination
Clinical Examination:
History taking:
- Detailed menstrual history to confirm gestational age
- Onset, duration, and amount of vaginal bleeding
- Associated symptoms such as abdominal pain or cramping
- Past obstetric and gynecological history, including previous miscarriages, ectopic pregnancies, or pelvic infections
- Medical and surgical history, including any chronic illnesses or medications
- Lifestyle factors such as smoking, alcohol consumption, and drug use
Physical examination:
- Vital signs assessment, including blood pressure, pulse rate, and temperature
- Abdominal examination to assess for tenderness, guarding, or masses
- Pelvic examination to evaluate cervical dilatation, effacement, and bleeding
- Speculum examination to visualize the cervix and assess for any bleeding or discharge
- Bimanual examination to assess uterine size, tenderness, and adnexal masses
Investigations:
- Transvaginal ultrasound to assess fetal viability, gestational age, and identify any abnormalities such as subchorionic hematoma or retained products of conception
- Blood tests to measure serum hCG levels and assess for anemia or infection
- Other investigations as indicated, such as karyotyping or thrombophilia screening[7]
Diagnosis
Diagnosis:
(1) Firstly, Blood—for hemoglobin, hematocrit, ABO and Rh grouping. Blood transfusion may be required if abortion becomes inevitable and anti-D gamma globulin has to be given in Rh-negative nonimmunized women.
(2) Secondly, Urine for immunological test of pregnancy is not helpful as the test remains positive for a variable period even after the fetal death.
Ultrasonography (TVS) findings may be:
- A well-formed gestation ring with central echoes from the embryo indicating healthy fetus.
- Observation of fetal cardiac motion. With this there is 98% chance of continuation of pregnancy.
- A blighted ovum evidence by loss of definition of the gestation sac, smaller mean gestational sac diameter, absent fetal echoes and absent fetal cardiac movements. Serum progesterone value of 25 ng/mL or more generally indicates a viable pregnancy in about 95% of cases. Serial serum hCG level is helpful to assess the fetal well-being. Ectopic pregnancy must rule out during investigations [2]
Differential Diagnosis
Differential Diagnosis:
- Ectopic Pregnancy: This is a life-threatening condition where the fertilized egg implants outside the uterus, most commonly in the fallopian tube. Symptoms can include abdominal pain and vaginal bleeding.
- Cervical Polyp: These are benign growths on the cervix that can bleed, especially after intercourse.
- Molar Pregnancy: This is a rare condition where abnormal tissue grows in the uterus instead of a fetus. It can cause vaginal bleeding and an abnormally high level of hCG (human chorionic gonadotropin).
- Inevitable Miscarriage: This occurs when the cervix has dilated and the miscarriage is in progress.
- Incomplete Miscarriage: This is when some, but not all, of the pregnancy tissue has passed.[8]
Complications
Complications:
Miscarriage: The most significant complication of a threatened miscarriage is the loss of the pregnancy. While many women with threatened miscarriage go on to have healthy pregnancies, the risk of miscarriage is higher than in pregnancies without bleeding or cramping.
Preterm Labor and Delivery: In some cases, threatened miscarriage can lead to preterm labor and delivery. This is more likely if the bleeding is heavy or accompanied by severe cramping. Premature babies face a variety of health challenges, including breathing difficulties, feeding problems, and developmental delays.
Infection: Rarely, a threatened miscarriage can lead to an infection of the uterus or amniotic sac. This can cause fever, chills, and abdominal pain. If left untreated, an infection can be life-threatening.
Psychological Distress: Experiencing a threatened miscarriage can be emotionally distressing. Women may feel anxious, depressed, or guilty. It’s important to seek support from loved ones, healthcare providers, or a therapist during this difficult time.[7]
Investigations
Investigations:
- Ultrasound examination: To assess fetal cardiac activity, gestational age, and identify any abnormalities.
- Maternal blood tests: To measure human chorionic gonadotropin (hCG) levels and assess progesterone levels if indicated.
- Cervical examination: To evaluate for cervical dilation or signs of infection.
- Other investigations: May be considered based on clinical presentation and include testing for infections, genetic abnormalities, or anatomical abnormalities."[7]
Treatment
Treatment:
- Rest- The patient should in bed for few days until bleeding stops. Prolonged restriction of activity has got no therapeutic value.
- Drugs- Relief of pain may ensure by diazepam 5 mg tablet twice daily. There is some evidence that treatment with progesterone improves the outcome. Progesterone induces immunomodulation to shift the Th-1 (proinflammatory response) to Th-2 (anti-inflammatory response). Use of hCG is not preferred.[7]
Prognosis
The prognosis:
(1) In about two-thirds, the pregnancy continues beyond 28 weeks.
(2) In the rest, it terminates either as inevitable or missed miscarriage. If the pregnancy continues, there increase frequency of preterm labor, placenta previa, intrauterine growth restriction of the fetus and fetal anomalies. Blighted ovum It is a sonographic diagnosis. There is absence of fetal pole in a gestational sac with diameter of 3 cm or more. Uterus is to evacuate once the diagnosis made.[1]
Prevention
Prevention:
- Bed rest: Although commonly recommended, there is no evidence that bed rest prevents progression to miscarriage.
- Progesterone supplementation: May be considered in women with a history of recurrent miscarriages, but its effectiveness in preventing threatened miscarriage is unclear.
- Cervical cerclage: May be indicated in women with cervical insufficiency, but its role in preventing threatened miscarriage is controversial.[7]
Homeopathic Treatment
Homoeopathic treatment of Threatened abortion
Homeopathic medicines are individualized, selected based on the individual case history of the patient, by taking into consideration the cause like hormonal imbalance, nutritional factor, emotional stress, the nature of the patient, and other factors which may be acting as a maintaining cause in the Threatened Abortion.
Threatened abortion, as it is a problem, requires a constitutional as well as acute remedy to control bleeding. Homeopathy focuses on the root cause of the problem and helps in the treatment of Threatened abortion. A well-chosen homeopathic remedy helps in controlling the amount of blood loss and, abdominal pain.
Medicines:
Aconite
- Threatened abortion from anger, especially fright; fears that something terrible is going to happen her; dizziness on rising from a recumbent position.
Arnica
- Threatened abortion as a result of fall, blow, shock, concussion, particularly when blood comes out without pain. *Sore pain all over body as if from a bruise.[2]
Belladonna
- Severe bearing down, as if everything would protrude through vulva; additionally pains come on suddenly and cease suddenly.
Caulophyllum
- With severe pain in back and loins but uterine contraction feeble; slight flow. Habitual abortion from uterine atony.
China
- If hemorrhage continues after abortion and there is giddiness, drowsiness and fainting.
- Extremely useful in removing the after-effects of hemorrhage, such as, heaviness in head, ringing in ears, coldness of extremities.
Sabina
- Threatened miscarriage, esp. during third month with pain commencing in the small of back and going round and through the pubes.
- Pain runs through from sacrum to pubes. Bright red, clotted flow of blood or bright red blood, partly fluid and partly clotted, increasing with every motion.
Viburnum
- Threatened abortion with intense cramping pains in uterus and bearing down.[2]
Diet & Regimen
Diet And Regimen:
For Threatened abortion
Diet:
Focus on nutrient-dense foods: Prioritize whole foods rich in vitamins, minerals, and antioxidants to support your overall health and the developing baby.
Fruits and vegetables: Aim for a variety of colorful produce for essential vitamins and fiber.
Lean protein: Include sources like poultry, fish, beans, and lentils for cell growth and repair.
Whole grains: Opt for whole-grain bread, pasta, and rice for sustained energy and fiber.
Healthy fats: Include avocados, nuts, seeds, and olive oil for essential fatty acids.
Hydration: Drink plenty of water to maintain fluid balance and support blood volume.
Limit processed foods: Reduce intake of sugary drinks, fast food, and processed snacks, which offer little nutritional value.
Regimen:
Rest: Listen to your body and prioritize rest. Avoid strenuous activities and heavy lifting.
Reduce stress: Engage in relaxation techniques like deep breathing, meditation, or prenatal yoga to manage stress levels.
Pelvic rest: Your doctor may advise avoiding sexual intercourse for a period to minimize any potential strain on the cervix.
Follow medical advice: Strictly adhere to your healthcare provider’s recommendations and any prescribed medications.
Emotional support: Seek emotional support from your partner, family, friends, or a therapist during this challenging time.
Do’s and Don'ts
The Do’s & Don’ts
Do’s:
- Seek medical attention immediately: If you experience any bleeding during pregnancy, contact your healthcare provider right away. They can assess the situation and provide guidance on the next steps.
- Get plenty of rest: Bed rest is often recommended during a threatened miscarriage to reduce the risk of further complications.
- Follow your doctor’s instructions: Your doctor may prescribe medications or recommend specific lifestyle changes to help manage the situation. It’s important to follow their instructions carefully.
- Stay hydrated: Drink plenty of fluids to avoid dehydration, which can worsen symptoms.
- Eat a healthy diet: A balanced diet rich in nutrients can help support your body during this time.
- Manage stress: Stress can negatively impact your pregnancy. Find healthy ways to manage stress, such as meditation, yoga, or spending time in nature.
- Seek emotional support: Talk to your partner, family, friends, or a therapist about your feelings. Sharing your concerns can help you cope with the emotional challenges of a threatened miscarriage.
Don’ts:
- Do Not panic: Although bleeding can be alarming, remember that many women experience it and go on to have successful pregnancies.
- Don’t engage in strenuous activity: Avoid heavy lifting, exercise, or any activity that puts stress on your body.
- Have Not sexual intercourse: Your doctor may advise against sexual intercourse until the bleeding stops and the risk of miscarriage decreases.
- Don’t use tampons or douche: These can increase the risk of infection.
- Don’t ignore any changes in symptoms: If you experience increased bleeding, severe pain, or any other concerning symptoms, contact your doctor immediately.
- Should’t self-medicate: Do not take any medications or supplements without consulting your doctor first.
- Don’t blame yourself: A threatened miscarriage is not your fault. There are many factors that can contribute to it, and it’s essential to be kind to yourself during this time.
Terminology
Terminology:
Threatened Miscarriage:
- Meaning: Vaginal bleeding during the first 20 weeks of pregnancy, signifying a potential risk of miscarriage. Although it can be alarming, it’s important to remember that many women who experience bleeding continue to have healthy pregnancies.
Miscarriage:
- Meaning: The spontaneous loss of a pregnancy before the 20th week.
Vaginal Bleeding:
- Meaning: The discharge of blood from the vagina. In the context of threatened miscarriage, it can vary in amount and color, ranging from light spotting to heavier flow.
First 20 weeks of pregnancy:
- Meaning: The initial period of pregnancy, which is crucial for the development of the fetus. A threatened miscarriage typically occurs within this timeframe.
Healthcare Provider:
- Meaning: Refers to a doctor, midwife, or any qualified medical professional who provides care during pregnancy.
Bed Rest:
- Meaning: A period of rest in bed, often recommended to reduce physical exertion and stress on the body during a threatened miscarriage.
Medications:
- Meaning: Drugs or pharmaceutical products prescribed by a doctor to manage symptoms or address underlying causes of a threatened miscarriage.
Lifestyle Changes:
- Meaning: Modifications to daily habits or routines, such as diet, exercise, or stress management techniques, recommended to support a healthy pregnancy.
Hydration:
- Meaning: The process of maintaining adequate fluid intake in the body, essential for overall health and well-being during pregnancy.
Healthy Diet:
- Meaning: A balanced and nutritious eating pattern that provides essential vitamins, minerals, and energy to support both the mother and the developing fetus.
Stress Management:
- Meaning: Techniques or practices used to cope with and reduce stress levels, promoting emotional and physical well-being during pregnancy.
Emotional Support:
- Meaning: Assistance and understanding provided by loved ones, therapists, or support groups to help manage the emotional challenges associated with a threatened miscarriage.
Strenuous Activity:
- Meaning: Physical activities that involve intense exertion or effort, which can put stress on the body and potentially increase the risk of complications during a threatened miscarriage.
Sexual Intercourse:
- Meaning: The act of engaging in sexual activity, which may be advised against during a threatened miscarriage to reduce the risk of further complications.
Tampons and Douching:
- Meaning: Feminine hygiene products that can increase the risk of infection and should be avoided during a threatened miscarriage.
Self-medicate:
- Meaning: The practice of taking medications or supplements without consulting a healthcare professional, which can be dangerous and should be avoided, especially during pregnancy.
Homoeopathic Terminology:
Threatened Miscarriage:
- Meaning: This refers to vaginal bleeding during the first 20 weeks of pregnancy, which may or may not lead to an actual miscarriage (loss of the pregnancy).
Homeopathic Remedies:
- Meaning: These are natural substances, often highly diluted, used in homeopathy to stimulate the body’s healing response.
Repertory:
- Meaning: A reference book used by homeopaths to find remedies based on specific symptoms.
Materia Medica:
- Meaning: A detailed collection of information about the properties and uses of homeopathic remedies.
Miasm:
- Meaning: A theoretical concept in homeopathy referring to an underlying predisposition to certain diseases or patterns of illness.
Constitutional Remedy:
- Meaning: A remedy chosen based on the individual’s overall physical, mental, and emotional characteristics, rather than just specific symptoms.
Potency:
- Meaning: The level of dilution of a homeopathic remedy. Higher potencies are considered more powerful but also require more careful prescribing.
Aggravation:
- Meaning: A temporary worsening of symptoms after taking a remedy, which is sometimes seen as a sign that the remedy is working.
Amelioration:
- Meaning: An improvement in symptoms after taking a remedy.
Provings:
- Meaning: Experiments conducted to determine the effects of a remedy on healthy individuals.
References
Refereneces:
- DC DUTTA Text book of Gynaecology
- The Homoeopathic Prescriber by K. C. Bhanja
American College of Obstetricians and Gynecologists [https://www.acog.org/womens-health/faqs/early-pregnancy-loss]
Clinical Journal of Obstetrics and Gynecology
- "Incidental Findings on First-Trimester Ultrasound" – Ultrasound in Obstetrics & Gynecology (2016)
American College of Obstetricians and Gynecologists: Early Pregnancy Loss (2020)–https://www.acog.org/womens-health/faqs/early-pregnancy-loss
"Williams Obstetrics," 26th Edition (2021)
- Beckmann, C. R. B., Ling, F. W., Barzansky, B. M., Herbert, W. N., Laube, D. W., & Smith, R. P. (2020). Obstetrics and Gynecology (8th ed.). Wolters Kluwer.
Also Search As
Also Searched As:
Online Search Engines:
- Use specific search terms:
- "homeopathy threatened miscarriage"
- "homeopathic remedies threatened abortion"
- "homeopathy for preventing miscarriage"
- Specify reliable sources:
- Include phrases like "peer-reviewed articles" or "scientific studies" in your search to find credible sources.
- Look for articles on websites of reputable homeopathic organizations or institutions.
Homeopathic Resources:
- Homeopathic websites and blogs: Many homeopathic practitioners and organizations have websites or blogs where they share information and articles. Search for those specializing in women’s health or pregnancy.
- Homeopathic journals: Search for articles in peer-reviewed homeopathic journals. These may require access through a library or professional association.
- Homeopathic books: Consult books on homeopathy and women’s health, looking for chapters or sections on threatened miscarriage.
Consulting a Homeopathic Practitioner:
- Ask for recommendations: A qualified homeopath can provide you with relevant articles or research on the topic. They can also tailor their advice to your specific situation.
Search engines:
- Simple and direct:
- "threatened miscarriage"
- "bleeding during early pregnancy"
- "signs of possible miscarriage"
- More specific questions:
- "what to do if I have bleeding in first trimester"
- "can a threatened miscarriage resolve itself?"
- "threatened miscarriage vs. inevitable miscarriage"
- Focus on reliable sources:
- Add "mayo clinic" or "cleveland clinic" to your query to filter for reputable medical websites.
- Look for websites ending in .gov or .edu, or those from well-known medical organizations.
Frequently Asked Questions (FAQ)
What is Threatened Miscarriage?
Definition
Threatened Miscarriage is a clinical entity where the process of miscarriage has started but has not progressed to a state from which recovery is impossible.
Can a threatened miscarriage be prevented?
In some cases, certain lifestyle changes and medical interventions can help reduce the risk of a threatened miscarriage. It’s essential to maintain a healthy lifestyle, manage stress, and attend regular prenatal appointments.
What are the symptoms of Threatened Miscarriage?
Symptoms
- Bleeding per vaginum
- Mild backache or dull pain in lower abdomen
Can homeopathy prevent a threatened miscarriage?
Yes, many women who experience a threatened miscarriage go on to have healthy pregnancies. It’s important to follow your doctor’s advice and take care of yourself during this time.
How long does it take to recover from a threatened miscarriage?
The recovery time varies depending on the individual and the severity of the situation. It may take a few days to a few weeks for the bleeding to stop and for the body to heal.
Can I still have a healthy pregnancy after a threatened miscarriage?
Yes, many women who experience a threatened miscarriage go on to have healthy pregnancies. It’s important to follow your doctor’s advice and take care of yourself during this time.
How can I cope with the emotional impact of a threatened miscarriage?
Yes, many women who experience a threatened miscarriage go on to have healthy pregnancies. It’s important to follow your doctor’s advice and take care of yourself during this time.
Are there any lifestyle changes that can help during a threatened miscarriage?
Yes, certain lifestyle changes can be helpful. These include getting plenty of rest, managing stress, eating a nutritious diet, staying hydrated, and avoiding strenuous activities.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Threatened Miscarriage?
homoeopathic medicines for threatened abortion
- Aconite
- Arnica
- Belladonna
- Caulophyllum
- China
- Sabina
- Viburnum
