Urticaria (Hives)
Definition
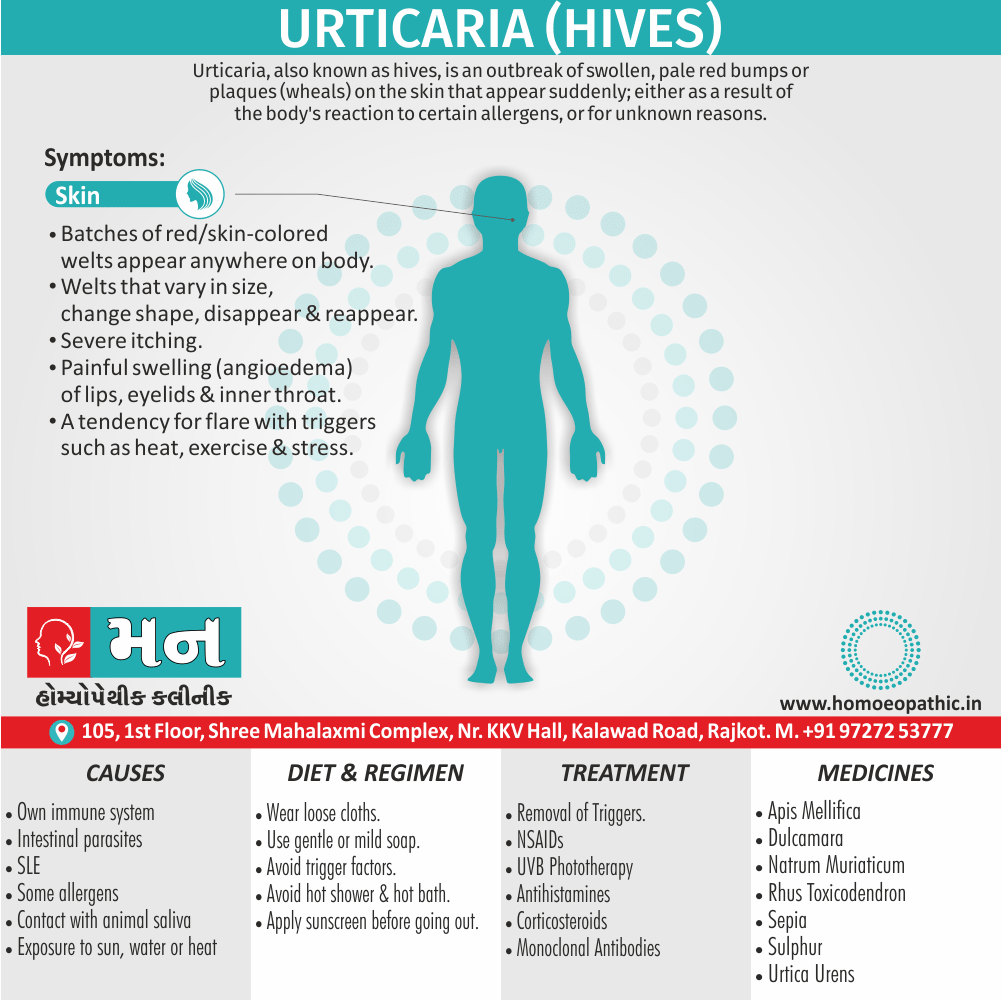
Urticaria, also known as hives, is an outbreak of swollen, pale red bumps or plaques (wheals) on the skin that appear suddenly; either as a result of the body’s reaction to certain allergens, or for unknown reasons. [3]
Urticaria, commonly known as hives, is a skin condition characterized by red, itchy welts.
While there isn’t an exact synonym for urticaria, it’s sometimes referred to as:
- Nettle rash: This term comes from the fact that the rash often resembles the sting of a nettle plant.
- Wheals: This is a more medical term for the raised, itchy bumps that characterize urticaria.
- Welts: A more common term for the raised, itchy bumps.
Please note that "hives" is the most widely used and understood term for this condition.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Urticaria (Hives)
It is also known as urticaria, welts, weals, or nettle rash.

Generalized Urticaria
- When an allergic reaction occurs, the body releases a protein called histamine.
- When histamine is release, the tiny blood vessels known as capillaries leak fluid.
- Moreover, The fluid accumulates in the skin and causes a rash.
- It is not contagious. [2]
- Hives usually cause itching, but may also burn or sting.
- They can appear anywhere on the body.
- Besides this, Hives vary in size (from a pencil eraser to a dinner plate), and may join together to form larger areas known as plaques.
- They can last for hours, or up to one day before fading.
- Urticaria (‘hives’) is cause by localise dermal oedema secondary to a temporary increase in capillary permeability.
- Lastly, If oedema involves subcutaneous or submucosal layers, the term angioedema is use.
Other factors
- Angioedema is similar to hives, but the swelling occurs beneath the skin instead of on the surface.
- Angioedema is characterize by deep swelling around the eyes and lips and sometimes of the genitals, hands, and feet.
- It generally lasts longer than hives, but the swelling usually goes away in less than 24 hours.
- Rarely, angioedema of the throat, tongue, or lungs can block the airways, causing difficulty breathing & may become life threatening. [3]
- Acute urticaria may associate with angioedema of the lips, face, tongue, throat and, rarely, wheezing, abdominal pain, headaches and even anaphylaxis.
- Urticaria present for less than 6 weeks is considered to be acute, also chronic if it continues for more than 6 weeks.
- Individual weals last for less than 24 hours; additionally if they persist, urticarial vasculitis needs to be considered. [1]b
Epidemiology
Epidemiology of Urticaria (Hives)
The epidemiology of urticaria in India indicates a significant burden, with an estimated lifetime prevalence of about 20%. A 2014 study on chronic urticaria in children found spontaneous urticaria as the most common type, and diverse triggers, including physical stimuli, food allergies, drugs, and infections. Most children responded to non-sedating antihistamines, but some needed additional therapies.
Other studies support a high lifetime prevalence and highlight acute urticaria as more common than chronic. The research continues to explore triggers, comorbidities, and quality of life impact, aiming to improve prevention and treatment in India.
Reference: Godse K, et al. Clinico-epidemiological features of chronic urticaria in children: A retrospective analysis of 296 children from a tertiary care institute in Northern India. Indian J Dermatol Venereol Leprol 2014;80:320-4. [7]
Causes
Causes of Acute & Chronic Urticaria (Hives):
- Autoimmune: Due to antibodies that cross-link the IgE receptor on mast cells
- Allergens: In foods, medications and inhalants
- Drugs
- Contact: e.g. latex, animal saliva
- Physical: e.g. heat, cold, pressure, sun, sweat, water
- Infection: e.g. intestinal parasites
- Others: e.g. systemic lupus erythematosus (SLE), pregnancy
- Idiopathic: Chronic spontaneous urticaria and angioedema
- Hepatitis B
- SLE
- Idiopathic [1]
Types
Types of Urticaria (Hives)
Acute urticaria:
- They are hives or swelling lasting less than 6 weeks.
- The most common causes are foods, medicines, latex, also infections.
- Insect bites or a disease may also be responsible.
- The most common foods that cause hives are nuts, chocolate, fish, tomatoes, eggs, fresh berries, soy, wheat, and milk.
- Fresh foods cause hives more often than cooked foods.
- Certain food additives also preservatives may also be to blame.
Chronic urticaria:
- They are hives or swelling that lasts more than 6 weeks.
- The cause is usually harder to find than in acute cases.
- The causes can be similar to those of acute urticaria but can also include your immune system, chronic infections, hormonal disorders, and tumors.
Physical urticaria:
- These are hives caused by direct physical stimulation of the skin; for example, cold, heat, sunlight, vibration, pressure, sweating, and exercise.
- They usually happen right where the skin was affected and rarely appear anywhere else. Most appear within 1 hour after exposure.
Dermatographism:
- These are hives that form after firmly stroking or scratching the skin.
Hereditary angioedema:
- It is painful swelling under the skin.
- It runs in families. [3]
Risk Factors
Risk factors of Urticaria (Hives)
- Atopy: Individuals with a personal or family history of atopy (allergic conditions such as asthma, eczema, or allergic rhinitis) are at an increased risk.
- Female Sex: Urticaria is more common in women than men, particularly chronic spontaneous urticaria.
- Autoimmune Diseases: There is a recognized association between urticaria and certain autoimmune conditions, including thyroid disease, systemic lupus erythematosus, and Sjögren’s syndrome.
- Infections: Both viral and bacterial infections can trigger or exacerbate urticaria.
- Medications: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), antibiotics, and angiotensin-converting enzyme (ACE) inhibitors, can induce urticaria.
- Physical Stimuli: Physical urticarias are triggered by specific stimuli, such as heat, cold, pressure, or sunlight.
- Stress: Emotional stress can worsen existing urticaria or act as a trigger in susceptible individuals.
Please note that this is not an exhaustive list, and other factors may also play a role in the development of urticaria. It is always recommended to consult a qualified healthcare professional for personalized advice and management of any health condition.[6]
Pathogenesis
Pathogenesis of Urticaria (Hives)
1. Mast Cell Activation:
- Mast cells, located in the skin and other tissues, play a central role in urticaria.
- Various triggers, including allergens, physical stimuli, or autoimmune processes, can lead to mast cell activation.
- Activated mast cells release histamine and other inflammatory mediators, resulting in increased vascular permeability and the characteristic wheals and angioedema.
2. Histamine and Other Mediators:
- Histamine is a potent vasodilator that causes blood vessels to widen, leading to increased blood flow and leakage of fluid into the surrounding tissues.
- This results in the formation of the raised, itchy wheals seen in urticaria.
- Other mediators released from mast cells, such as prostaglandins and leukotrienes, also contribute to the inflammatory response and symptoms of urticaria.
3. Immunological and Non-Immunological Pathways:
- Urticaria can be triggered by both immunological and non-immunological mechanisms.
- Immunological urticaria is often associated with IgE-mediated allergic reactions, where allergens bind to IgE antibodies on mast cells, triggering their activation.
- Non-immunological urticaria can be triggered by various factors, including physical stimuli, medications, and certain foods, which directly activate mast cells or other inflammatory pathways.
4. Chronic Urticaria:
- The pathogenesis of chronic urticaria is less well understood.
- Autoimmune mechanisms are thought to play a significant role, with autoantibodies targeting IgE receptors or other components of the immune system, leading to chronic mast cell activation.
5. Other Factors:
- Genetic predisposition, environmental factors, and underlying medical conditions can also contribute to the development and severity of urticaria.
Understanding the complex pathogenesis of urticaria is crucial for developing effective treatments and management strategies for this common and often distressing condition.[6]
Pathophysiology
Pathophysiology of Urticaria (Hives)
The pathophysiology of urticaria involves the following key events:
Mast Cell Degranulation:
The primary event in urticaria is the activation and degranulation of mast cells, which are immune cells found in the skin and other tissues.
Mediator Release:
Mast cell degranulation leads to the release of various inflammatory mediators, primarily histamine. Histamine causes blood vessels to dilate and become leaky, resulting in the characteristic wheals (hives) of urticaria.
Vascular Changes:
The increased vascular permeability leads to plasma leakage into the surrounding tissues, causing swelling (edema) and the raised appearance of the wheals.
Sensory Nerve Stimulation:
Histamine and other mediators also stimulate sensory nerves in the skin, causing the intense itching (pruritus) associated with urticaria.
Additional Mediators:
Besides histamine, mast cells release other mediators like prostaglandins and leukotrienes, which further contribute to the inflammatory response and symptoms.
Immunological and Non-Immunological Triggers:
Mast cell degranulation can be triggered by both immunological (allergic) and non-immunological mechanisms. In allergic urticaria, allergens bind to IgE antibodies on mast cells, leading to their activation. Non-immunological triggers can include physical stimuli, medications, and certain foods.
Key Points:
- Central Role of Mast Cells: The activation and degranulation of mast cells are central to the pathophysiology of urticaria.
- Histamine: Histamine is the primary mediator responsible for the vascular changes and itching associated with urticaria.
- Vascular Leakage: Increased vascular permeability leads to plasma leakage and edema, forming the wheals.
- Multiple Triggers: Urticaria can be triggered by both immunological and non-immunological mechanisms.
Understanding the pathophysiology of urticaria helps guide the development of effective treatments aimed at blocking mast cell degranulation, inhibiting histamine release, or counteracting the effects of inflammatory mediators.[6]
Clinical Features
Clinical Features of Urticaria (Hives)
The clinical features of urticaria typically include:
Wheals:
The hallmark of urticaria is the appearance of wheals, which are raised, itchy, and often transient skin lesions. They can vary in size and shape, from small, round bumps to large, irregular patches.
Erythema:
The wheals are usually surrounded by a red flare (erythema) due to the dilation of blood vessels.
Pruritus:
Intense itching (pruritus) is a common and often distressing symptom of urticaria.
Angioedema:
In some cases, urticaria may be accompanied by angioedema, which is a deeper swelling of the skin and subcutaneous tissues, often affecting the face, lips, tongue, or extremities.
Distribution:
Urticaria can affect any part of the body, but it often occurs on the trunk, limbs, and face.
Duration:
The duration of individual wheals is usually less than 24 hours, but new wheals may continue to appear.
Additional features that may be present in some cases include:
Dermographism:
In dermographism, wheals appear after firm stroking or scratching of the skin.
Systemic Symptoms:
In rare cases, urticaria may be associated with systemic symptoms such as fever, joint pain, or abdominal discomfort.
Chronic Urticaria:
Chronic urticaria is defined as urticaria lasting for more than 6 weeks. It can have a significant impact on quality of life due to the persistent itching and discomfort.
It is important to note that the clinical features of urticaria can vary depending on the underlying cause and individual factors. If you are experiencing symptoms of urticaria, it is recommended to consult a qualified healthcare professional for diagnosis and appropriate management.[6]
Sign & Symptoms
Sign & Symptoms of Urticaria (Hives)
- Batches of red or skin-colored welts (wheals), which can appear anywhere on the body.
- Welts that vary in size, change shape, move around, disappear and reappear over short periods of time.
- The bumps; red or skin-colored “weals” with clear edges usually appear suddenly and go away just as quickly.
- Itching, which may severe.
- Painful swelling (angioedema) of the lips, eyelids and inside the throat.
- A tendency for signs and symptoms to flare with triggers such as heat, exercise and stress. [3]
Clinical Examination
Clinical Examination of Urticaria (Hives)
The clinical examination for urticaria primarily focuses on identifying the characteristic skin lesions and assessing their distribution and severity.
Key aspects of the clinical examination include:
Inspection:
- Careful examination of the skin to identify wheals, which are typically raised, itchy, and transient skin lesions.
- Note the size, shape, distribution, and duration of the wheals.
- Look for any associated angioedema, which presents as deeper swelling of the skin and subcutaneous tissues.
Dermographism:
- Lightly stroke or scratch the skin with a blunt object to assess for dermographism, a condition where wheals appear in response to physical stimulation.
Systemic Symptoms:
- Inquire about any associated systemic symptoms such as fever, joint pain, or abdominal discomfort.
Triggers:
- Ask the patient about potential triggers for their urticaria, including recent medications, food intake, infections, or exposure to physical stimuli.
Additional considerations during the clinical examination may include:
Assessment of Disease Severity:
- Evaluate the extent and severity of the urticaria, including the number and size of wheals, the presence of angioedema, and the impact on the patient’s quality of life.
Identification of Underlying Cause:
- Consider possible underlying causes for the urticaria, such as allergies, infections, autoimmune diseases, or medications.
Evaluation for Comorbidities:
- Assess for the presence of any associated conditions, such as atopic dermatitis, asthma, or allergic rhinitis.
The clinical examination plays a crucial role in diagnosing urticaria and guiding further investigations to identify any underlying causes or triggers. It also helps determine the severity of the condition and tailor appropriate management strategies.
Diagnosis
Diagnosis of Urticaria (Hives)
A health professional can diagnose acute urticaria by examining the rash on the skin.
The doctor will probably ask about:
- When and where the episode began
- Whether there has an insect bite
- Whether the patient lives or works in a place where potential triggers may exist, such as latex gloves, chemicals, or animals
- Any medications the patient has taking, including herbal supplements
- Patient’s medical history
- Any family history of urticaria
Allergy tests of patient’s blood and skin should done to find out whether there is an allergy to specific substances, such as chemicals, dust mites, or some food.
Investigations should guide by the history and possible causes but are often negative, particularly in acute urticaria.
Some or all of the following may be appropriate:
- Full blood count: Eosinophilia in parasitic infection or drug cause.
- Erythrocyte sedimentation rate (ESR) or plasma viscosity: Elevated in vasculitis.
- Urea and electrolytes, thyroid and liver function tests, iron studies: May reveal an underlying systemic disorder.
- Total IgE and specific IgE to possible allergens: e.g. shellfish, peanut, house dust mite.
- Antinuclear factor: Positive in systemic lupus erythematosus (SLE) and often positive in urticarial vasculitis.
- Complement C3 and C4 levels: If these are low due to complement consumption, C1 esterase inhibitor activity should be measured.
- Skin biopsy: If urticarial vasculitis is suspect.
- Challenge tests: To confirm physical urticarias. [1]
Differential Diagnosis
Diffrential Diagnosis of Urticaria
The differential diagnosis for urticaria includes various conditions that can present with similar skin lesions or symptoms.
Key considerations in the differential diagnosis include:
Angioedema:
- While often associated with urticaria, angioedema can also occur independently.
- It presents as deeper swelling of the skin and subcutaneous tissues, often affecting the face, lips, tongue, or extremities.
Vasculitis:
- Certain types of vasculitis can mimic urticaria, particularly urticarial vasculitis, which presents with persistent, painful wheals that may leave behind bruising or pigmentation.
Bullous Pemphigoid:
- This autoimmune blistering disease can sometimes present with urticarial lesions before the development of blisters.
Drug Eruptions:
- Various medications can cause skin reactions that resemble urticaria, including maculopapular eruptions, fixed drug eruptions, and erythema multiforme.
Insect Bites:
- Insect bites can cause localized urticarial reactions, but they typically have a central punctum and may be associated with other symptoms like pain or swelling.
Mastocytosis:
- In rare cases, urticaria pigmentosa, a form of mastocytosis, can present with persistent brown or reddish-brown macules or papules that urticate upon rubbing.
Other conditions that may need to be considered in the differential diagnosis include:
Hereditary Angioedema:
- A rare genetic condition characterized by recurrent episodes of angioedema without associated urticaria.
Urticarial Dermatitis:
- A chronic inflammatory skin condition characterized by persistent, itchy, and often eczematous lesions.
Psychogenic Urticaria:
- Urticaria triggered or exacerbated by psychological factors, such as stress or anxiety.
Accurate diagnosis is essential for appropriate management of urticaria and any underlying conditions. A thorough clinical examination, along with a detailed history and relevant investigations, helps differentiate urticaria from other potential diagnoses.[6]
Complications
Complications
While urticaria is generally a self-limiting condition, it can occasionally lead to certain complications:
Angioedema:
- This is the most common complication, involving swelling of deeper tissues, particularly the face, lips, tongue, and eyelids.
- It can cause airway obstruction, posing a serious risk if the larynx is affected.
Anaphylaxis:
- Although rare, urticaria can be associated with anaphylaxis, a severe, life-threatening allergic reaction characterized by widespread hives, difficulty breathing, and circulatory collapse.
Psychological Impact:
- Chronic urticaria can significantly affect quality of life due to persistent itching, sleep disturbances, and social limitations. This can lead to anxiety, depression, and decreased overall well-being.
Impaired Daily Activities:
- Severe or chronic urticaria can interfere with daily activities, work, and social interactions, further contributing to psychological distress.
Secondary Infections:
- In rare cases, excessive scratching of urticarial lesions can lead to secondary bacterial infections.
Scarring:
- Urticarial vasculitis, a rare variant of urticaria, can sometimes cause scarring due to inflammation of blood vessels in the skin.
Systemic Complications:
- While uncommon, urticaria can be associated with systemic manifestations in certain cases, such as fever, joint pain, or gastrointestinal symptoms.
It’s important to recognize these potential complications and seek prompt medical attention if any concerning symptoms arise. Early diagnosis and appropriate management can help prevent or minimize the impact of these complications.[6]
Investigations
Investigations of Urticaria (Hives)
The investigation of urticaria aims to identify any underlying causes or triggers, assess the severity of the condition, and guide appropriate management.
Key investigations may include:
Detailed History:
- A comprehensive history is crucial to identify potential triggers, such as recent medications, food intake, infections, or exposure to physical stimuli.
- The duration and severity of symptoms, as well as any associated systemic manifestations, should be assessed.
Physical Examination:
- A thorough skin examination is necessary to identify the characteristic wheals and assess their distribution and severity.
- Dermographism should be tested for by lightly stroking the skin.
Laboratory Tests:
- Basic blood tests, including a complete blood count (CBC) and erythrocyte sedimentation rate (ESR), may be performed to screen for underlying infections or inflammatory conditions.
- Allergy testing, such as skin prick tests or specific IgE blood tests, may be considered if an allergic trigger is suspected.
- Autoantibody testing may be indicated in cases of chronic urticaria to assess for autoimmune causes.
Other Investigations:
- Depending on the clinical presentation and suspected underlying cause, additional investigations may be warranted. These could include imaging studies, biopsies, or specialized tests for specific triggers or associated conditions.
The choice of investigations should be tailored to the individual patient, taking into account the clinical presentation, duration of symptoms, and suspected underlying cause. A step-wise approach is often recommended, starting with basic investigations and progressing to more specialized tests as needed.[6]
Treatment
Treatment
- Removal or treatment of any trigger is essential, although this may not identified in the majority of cases.
- Urticaria may precipitate by aspirin, NSAIDs, codeine and opioids, and it is advisable to suggest alternatives such as paracetamol.
- In chronic urticaria, non-sedating antihistamines, such as fexofenadine, loratadine or cetirizine, are usually beneficial.
- If, after 2 weeks, there is lack of response, an alternative non-sedating antihistamine should be used and an H2-blocker, such as cimetidine or ranitidine, is often added.
- Mast cell stabilisers or leukotriene receptor antagonists, such as montelukast, may added for more recalcitrant disease.
- For chronic urticaria, narrowband UVB phototherapy is valuable.
- Systemic corticosteroids are widely prescribe for urticaria, but often need to use at high doses and are only appropriate for occasional short courses.
Other treatments
- Patients with a history of life-threatening anaphylaxis, as in peanut or wasp sting allergy, should carry a self administered adrenaline (epinephrine) injection kit. [1]
- Antidepressants: The tricyclic antidepressant doxepin (Zonalon), use in cream form, can help relieve itching. This drug may cause dizziness and drowsiness.
- Asthma drugs with antihistamines: Medications that interfere with the action of leukotriene modifiers may helpful when used with antihistamines. Examples are montelukast (Singulair) and zafirlukast (Accolate).
- artificial (monoclonal) antibodies: The drug omalizumab (Xolair) is very effective against a type of difficult-to-treat chronic hives. It’s an injectable medicine that’s usually given once a month.
- Immune-suppressing drugs. Options include cyclosporine (Gengraf, Neoral, others) and tacrolimus (Astagraf XL, Prograf, Protopic). [4]
Lifestyle and home remedies:
Chronic hives can go on for months and years.
They can interfere with sleep, work and other activities.
The following precautions may help prevent or soothe the recurring skin reactions of chronic hives:
- Wear loose, light clothing.
- Avoid scratching or using harsh soaps.
- Soothe the affected area with a bath, fan, cool cloth, lotion or anti-itch cream.
- Keep a diary of when and where hives occur, what you were doing, what you were eating, and so on. This may help you and your doctor identify triggers.
- Avoid known triggers.
- Apply sunscreen before going outside. [4]
Prevention
Prevention of Urticaria
The prevention of urticaria focuses on identifying and avoiding triggers, as well as managing any underlying conditions that may contribute to the development of hives.
Key preventive measures include:
Identify and Avoid Triggers:
Keep a detailed diary of symptoms and potential triggers to identify any patterns or associations.
Once triggers are identified, take steps to avoid them, such as:
- Avoiding known allergens or irritants.
- Taking precautions to prevent physical urticaria, such as wearing loose clothing and avoiding excessive heat or cold exposure.
- Managing stress through relaxation techniques or seeking professional help if needed.
Manage Underlying Conditions:
If urticaria is associated with an underlying condition, such as an infection or autoimmune disease, proper management of that condition can help prevent or reduce the frequency and severity of hives.
Medication Review:
If urticaria is suspected to be drug-induced, a review of current medications with a healthcare professional is essential.
Alternative medications may be considered if necessary.
General Preventive Measures:
Maintain good overall health through a balanced diet, regular exercise, and adequate sleep.
Avoid scratching or rubbing the affected skin, as this can worsen symptoms.
Use gentle, fragrance-free skincare products.
Consider using antihistamines prophylactically if triggers are unavoidable or unpredictable.
It’s important to note that the effectiveness of preventive measures can vary depending on the individual and the underlying cause of urticaria. Working closely with a healthcare professional to develop a personalized prevention plan is crucial for managing this condition and minimizing its impact on quality of life.[6]
Homeopathic Treatment
Homoeopathic Treatment
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Urticaria :
Apis Mellifica – top grade medicine for urticaria:
- Apis Mellifica is best prescribe for urticaria when symptoms include marked itching also burning.
- A characteristic stinging pain in the urticarial eruptions is also observed.
- The skin is extremely sensitive to the touch.
- This is one of the best medicines for urticaria that gets triggered in heat.
- Going out in the either open air or cold applications bring some relief.
- And is also a top-rated medicine for urticaria that arises following an insect bite.
Natrum Muriaticum – for urticaria triggered by exercise and sun exposure:
- For treating urticaria triggered by exercise, Natrum Mur is a great option.
- The person who needs Natrum Mur will get large hives on the skin from exertion.
- This is attend with violent itching also burning.
- Natrum Mur is also one of the most effective medicines especially for solar urticaria that arises from exposure to the sun.
Astacus Fluviatilis & Urtica Urens – excellent homeopathic medicine for urticaria:
- Urtica Urens also Astacus Fluviatilis work wonders in treating urticaria.
- The choice between the two is made based on unique symptoms.
- Urticaria that appears every year, in the same season, is best treated with Urtica Urens.
- Another key symptom associated with Urtica Urens is urticaria with intense burning and formication on the skin.
- Urtica Urens also shows great results in urticaria that alternates with rheumatism.
- Apart from this, urtica is also the ideal medicine for treating urticaria from eating shellfish.
- Astacus Fluviatilis is well indicated where urticaria is attended with liver complaints.
- The person prescribed astacus will have itching over his entire body, with a marked stinging sensation on the skin.
Rhus Tox & Sepia Succus – for urticaria from cold exposure (cold-induced urticaria):
- Both are highly effective medicines for treating urticaria resulting from exposure to cold.
- Marked sensitivity to cold is found in persons needing rhus tox also sepia succus.
- Key symptoms that will decide in favor of medicine rhus tox is urticaria from cold exposure with itching and smarting sensation.
- Warm applications provide some relief especially from itching.
- The characteristic symptom to look out for while prescribing Sepia Succus is urticaria from going in cool open air.
- Being in a warm room brings relief.
- Urticarial eruptions with itching, which is not relieve especially by scratching, is another guiding feature for use of Sepia Succus.
Sulphur & Apis Mellifica – for urticaria triggered by heat:
- Persons with urticaria that gets triggered by exposure to heat will benefit greatly from Sulphur and Apis Mellifica.
- In detail, Sulphur is select for urticarial eruptions arising from heat exposure and attended with itching and burning.
- Scratching worsens the itching.
- In some cases, even washing may worsen the itching.
- Most persons prescribed Sulphur will notice a worsening of itching towards the evening.
- It is also the best solution for urticaria cases that have been suppressed with ointments in the past.
- Apis Mellifica is rate among the best medicines for urticaria triggered specifically by heat, with marked itching, burning, also stinging in the eruptions.
- Cold applications may bring relief from symptoms in some cases.
- Lastly, Some persons prescribed Apis for urticaria will feel better by going out in the open air.
Bovista Lycoperdon & Calcarea Phosphoricum – for urticaria triggered by water:
- Generally, Bovista Lycoperdon and Calcarea Phos are prominently indicated medicines for treating urticaria set off by coming into contact with water (water induced urticaria).
- Furthermore, Some features unique to bovista lycoperdon are urticaria on waking in the morning time and attended with diarrhea.
- Homeopathic medicine calcarea phosphorica is suggest where contact with cold water leads to urticarial eruptions.
Rhus Tox & Dulcamara – For urticaria from scratching (dermatographic urticaria)
- For urticaria from severe scratching, Rhus Tox also Dulcamara are very useful Homeopathic medicines.
- Where urticaria leads to red, swollen skin with itching, burning and smarting, you know Homeopathic medicine Rhus Tox will show best results.
- Rubbing worsens the symptoms in this case.
- Rhus Tox is also well indicate for urticaria resulting from getting wet.
- Dulcamara is the best choice in case of violent itching in the urticarial eruptions.
- Use of Dulcamara is also suggested for urticaria arising from exposure to cold and that which gets triggered in wet weather. [5]
Diet & Regimen
Diet & Regimen of Urticaria
the role of diet and regimen in managing urticaria is primarily focused on identifying and avoiding potential triggers and maintaining overall health to support the immune system.
Key recommendations include:
Identify and Eliminate Trigger Foods:
- If a food allergy is suspected as a trigger for urticaria, an elimination diet may be recommended to identify the culprit food.
- This involves avoiding certain foods for a period of time and then gradually reintroducing them to observe any reactions.
- Common trigger foods include nuts, shellfish, eggs, dairy products, and certain fruits.
Consider a Low-Histamine Diet:
- Some individuals with chronic urticaria may benefit from a low-histamine diet, which involves avoiding foods that are high in histamine or that trigger histamine release.
- Examples of high-histamine foods include fermented foods, aged cheeses, processed meats, and certain fish.
Maintain a Healthy Lifestyle:
- A balanced diet rich in fruits, vegetables, and whole grains is important for overall health and immune function.
- Regular exercise and stress management techniques, such as meditation or yoga, can also help reduce the frequency and severity of urticaria.
Avoid Alcohol and Smoking:
- Alcohol and smoking can worsen urticaria symptoms and should be avoided.
Stay Hydrated:
- Drinking plenty of water is important for skin health and overall well-being.
It’s important to note that dietary recommendations may vary depending on the individual and the specific triggers for their urticaria. Consulting a registered dietitian or healthcare professional can provide personalized guidance on dietary modifications and lifestyle changes to manage urticaria effectively.[6]
Do’s and Don'ts
Do’s & Don’ts
Urticaria Do’s and Don’ts
Do’s:
- Identify and avoid triggers: Keep a diary to track possible triggers like foods, medications, or environmental factors. Once identified, try to avoid them.
- Take antihistamines: These medications can help reduce itching and swelling associated with hives. Consult your doctor for the right dosage and type.
- Apply cool compresses: Applying cool compresses or taking cool showers can soothe itchy skin.
- Wear loose-fitting clothes: Tight clothes can irritate the skin and worsen hives. Opt for loose, comfortable clothing made from natural fibers.
- Manage stress: Stress can trigger or worsen hives. Practice stress-reducing techniques like yoga, meditation, or deep breathing exercises.
- Keep skin moisturized: Dry skin can worsen itching. Apply a fragrance-free moisturizer regularly.
- Seek medical advice: If you have severe or persistent hives, consult a doctor to rule out any underlying causes and discuss treatment options.
- Carry an epinephrine auto-injector: If you have a history of severe allergic reactions, carry an epinephrine auto-injector in case of anaphylaxis.
Don’ts:
- Scratch: Scratching can worsen hives and lead to secondary infections.
- Use hot water: Hot showers or baths can irritate the skin and exacerbate itching.
- Wear tight clothing or jewelry: These can rub against the skin and trigger hives.
- Use harsh soaps or detergents: Opt for gentle, fragrance-free products to avoid irritating the skin.
- Consume alcohol or spicy foods: These can trigger or worsen hives in some people.
- Smoke: Smoking can irritate the skin and contribute to inflammation.
- Ignore severe symptoms: Seek immediate medical attention if you experience difficulty breathing, swelling of the face or throat, or other signs of anaphylaxis.
Remember, these are general recommendations. It is crucial to consult your doctor for personalized advice and treatment for urticaria.
Terminology
Terminology
Here are some terminologies and their meanings commonly used in articles about Urticaria:
Urticaria
Also known as hives, it is a skin condition characterized by itchy, raised welts or wheals that appear and disappear relatively quickly.
Angioedema
A similar condition to urticaria but involves swelling of deeper layers of skin, often affecting the face, lips, tongue, and throat. It can be dangerous if it affects breathing.
Wheals
The raised, itchy, and often transient skin lesions characteristic of urticaria.
Erythema
Redness of the skin caused by increased blood flow in superficial capillaries.
Pruritus
Intense itching, a common and often distressing symptom of urticaria.
Dermographism
A type of urticaria where wheals appear after firm stroking or scratching of the skin.
Acute Urticaria
Urticaria lasting less than 6 weeks.
Chronic Urticaria
Urticaria persisting for more than 6 weeks.
Chronic Spontaneous Urticaria (CSU)
The most common type of chronic urticaria, with no identifiable trigger.
Inducible Urticaria
Urticaria triggered by specific stimuli, such as heat, cold, pressure, or exercise.
Mast Cells
Immune cells in the skin and other tissues that release histamine and other inflammatory mediators, leading to urticaria symptoms.
Histamine
A chemical released by mast cells that causes blood vessels to dilate and become leaky, resulting in the characteristic wheals of urticaria.
Antihistamines
Medications that block the action of histamine, used to treat urticaria.
Anaphylaxis
A severe, life-threatening allergic reaction that can sometimes be associated with urticaria.
Understanding these terminologies will help you better comprehend articles and discussions about urticaria, its causes, symptoms, and treatment options.
Here are some terminologies and their meanings commonly used in homeopathic articles about Urticaria:
Acute Urticaria:
A sudden onset of urticaria that typically resolves within six weeks. It’s often associated with identifiable triggers like allergens or infections.
Chronic Urticaria:
Urticaria persisting for more than six weeks, with or without identifiable triggers. It’s often associated with underlying health conditions or imbalances.
Suppression:
In homeopathy, suppression refers to the temporary relief of symptoms without addressing the underlying cause, potentially leading to deeper or more chronic health issues.
Miasm:
A fundamental concept in homeopathy, representing a predisposition to certain diseases or disease patterns. Understanding the miasm helps in selecting the most suitable remedy.
Constitutional Remedy:
A remedy chosen based on the individual’s overall physical, mental, and emotional characteristics, aiming to treat the root cause of the disease and promote long-term health.
Aggravation:
A temporary worsening of symptoms after taking a homeopathic remedy, often seen as a positive sign indicating that the remedy is working.
Proving:
A systematic process in homeopathy where healthy individuals take a substance and carefully record their symptoms, helping to understand the substance’s therapeutic potential.
Repertory:
A reference book listing symptoms and the remedies associated with them, used by homeopaths to select appropriate remedies.
Materia Medica:
A collection of detailed information about the therapeutic properties and provings of various homeopathic remedies.
Some homeopathic remedies commonly mentioned in relation to urticaria include:
- Apis Mellifica: Useful for urticaria with stinging, burning pains, and swelling, often worse from heat and better from cold applications.
- Urtica Urens: Derived from stinging nettle, it’s often used for urticaria with intense itching and burning, especially after exposure to irritants or allergens.
- Rhus Toxicodendron: Indicated for urticaria with restlessness, intense itching, and symptoms worse at night and from cold, damp weather.
- Arsenicum Album: Helpful for urticaria with burning and restlessness, often accompanied by anxiety and weakness.
- Dulcamara: Used for urticaria triggered or aggravated by damp, cold weather.
Remember, homeopathic treatment should be individualized and guided by a qualified homeopathic practitioner. Self-treatment is discouraged, as it can lead to improper remedy selection and potential complications.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition) Ch. 28
- https://www.medicalnewstoday.com/articles/157260.php
- https://www.webmd.com/skin-problems-and-treatments/guide/hives-urticaria-angioedema#1
- https://www.mayoclinic.org/diseases-conditions/chronic-hives/diagnosis-treatment/drc-20352723
- https://www.drhomeo.com/skin-problem/urticaria-and-homeopathic-treatment/
- "Rook’s Textbook of Dermatology, 10th Edition" by Burns T, Breathnach S, Cox N, Griffiths C published in 2020 by Wiley-Blackwell,
- Godse K, et al. Clinico-epidemiological features of chronic urticaria in children: A retrospective analysis of 296 children from a tertiary care institute in Northern India. Indian J Dermatol Venereol Leprol 2014;80:320-4.
Also Search As
Also Search As
People can search for homeopathic articles on Urticaria using a variety of methods:
Online Search Engines:
Use specific keywords:
"homeopathic treatment for urticaria"
"homeopathy for hives"
"homeopathic remedies for urticaria"
"urticaria case studies homeopathy"
Use advanced search operators:
Add "filetype:pdf" to find research articles or case studies in PDF format.
Use quotation marks to search for an exact phrase, e.g., "homeopathic management of urticaria."
Search on reputable homeopathic websites:
National Center for Homeopathy (NCH)
Homeopathy Research Institute (HRI)
British Homeopathic Association (BHA)
Homeopathic Libraries and Databases:
Visit a local homeopathic library or clinic to access books, journals, and other resources.
Search online databases like:
HomBRex (Homeopathic Bibliographic Repertory Extended)
The American Institute of Homeopathy Library
Social Media and Forums:
Join online homeopathic communities and forums to connect with practitioners and patients discussing urticaria.
Follow homeopathic organizations and practitioners on social media for updates and articles.
Additional Tips:
Look for articles published in peer-reviewed homeopathic journals for evidence-based information.
Consider consulting a qualified homeopathic practitioner for personalized guidance and treatment recommendations.
By utilizing these methods and resources, individuals can access a wealth of information on the homeopathic approach to urticaria and make informed decisions about their healthcare.
There are several ways to search for information about urticaria, catering to various needs and levels of expertise:
General Web Search:
Search engines like Google, Bing, or DuckDuckGo are a good starting point.
Use keywords like "urticaria," "hives," "skin rash," or "itchy welts."
Add specific symptoms or concerns to refine your search, e.g., "urticaria causes" or "urticaria treatment."
Medical Websites and Databases:
Reputable health websites:
Mayo Clinic, WebMD, Healthline, NHS, mddoctorsclinic, etc.
They provide reliable information on causes, symptoms, diagnosis, and treatment options.
Medical databases:
PubMed, Google Scholar, etc.
These offer access to scientific articles and research papers for in-depth knowledge.
Image Search:
Use image search engines like Google Images or specialized medical image websites.
This helps visualize different types of urticaria and compare them to your symptoms.
Social Media & Forums:
Online communities and support groups can provide personal experiences and insights from people living with urticaria.
Be cautious about information shared online and always verify with healthcare professionals.
Books and Libraries:
Medical textbooks and dermatology books offer detailed information about urticaria.
Local libraries or university libraries may have resources on skin conditions.
Consulting a Healthcare Professional:
The most reliable way to get personalized information and treatment recommendations.
Doctors can diagnose, identify triggers, and suggest suitable treatment options.
Tips for Effective Searching:
Use specific and relevant keywords.
Consider using advanced search operators (e.g., quotation marks, filetype).
Look for credible sources, such as medical websites, research articles, or reputable organizations.
Be aware of the date of publication, especially for online resources, as medical information can change over time.
Remember, information found online should not replace professional medical advice. If you suspect you have urticaria, always consult a qualified healthcare professional for proper diagnosis and treatment.
Frequently Asked Questions (FAQ)
What is Urticaria (Hives)?
Urticaria, also known as hives, is an outbreak of swollen, pale red bumps or plaques (wheals) on the skin that appear suddenly; either as a result of the body’s reaction to certain allergens, or for unknown reasons.
Is urticaria contagious?
No, urticaria is not contagious and cannot be spread from person to person.
Give the types of Urticaria?
- Acute urticaria
- Chronic urticaria
- Physical urticaria
- Dermatographism
- Hereditary angioedema
What are the main causes of Urticaria (Hives)?
- Autoimmune
- Allergens
- Drugs
- Contact
- Physical: e.g. heat, cold, pressure, sun, sweat, water
- Infection: intestinal parasites
- Others: systemic lupus erythematosus (in other words, SLE), pregnancy
- Idiopathic
What are the symptoms of Urticaria (Hives)?
- Batches of red or skin-colored
- Welts that vary in size, change shape, move around, disappear and reappear
- The bumps; red or skin-colored “weals”
- Itching, which may severe.
- Painful swelling of the lips, eyelids and inside the throat.
- Flare with triggers
Homeopathic Medicines used by Homeopathic Doctors in treatment of Urticaria (Hives)?
Homeopathic Medicines :
- Apis Mellifica
- Natrum Muriaticum
- Urtica Urens
- Rhus Tox
- Sepia
- Sulphur
- Bovista Lycoperdon
- Dulcamara
