Vaginismus
Definition:
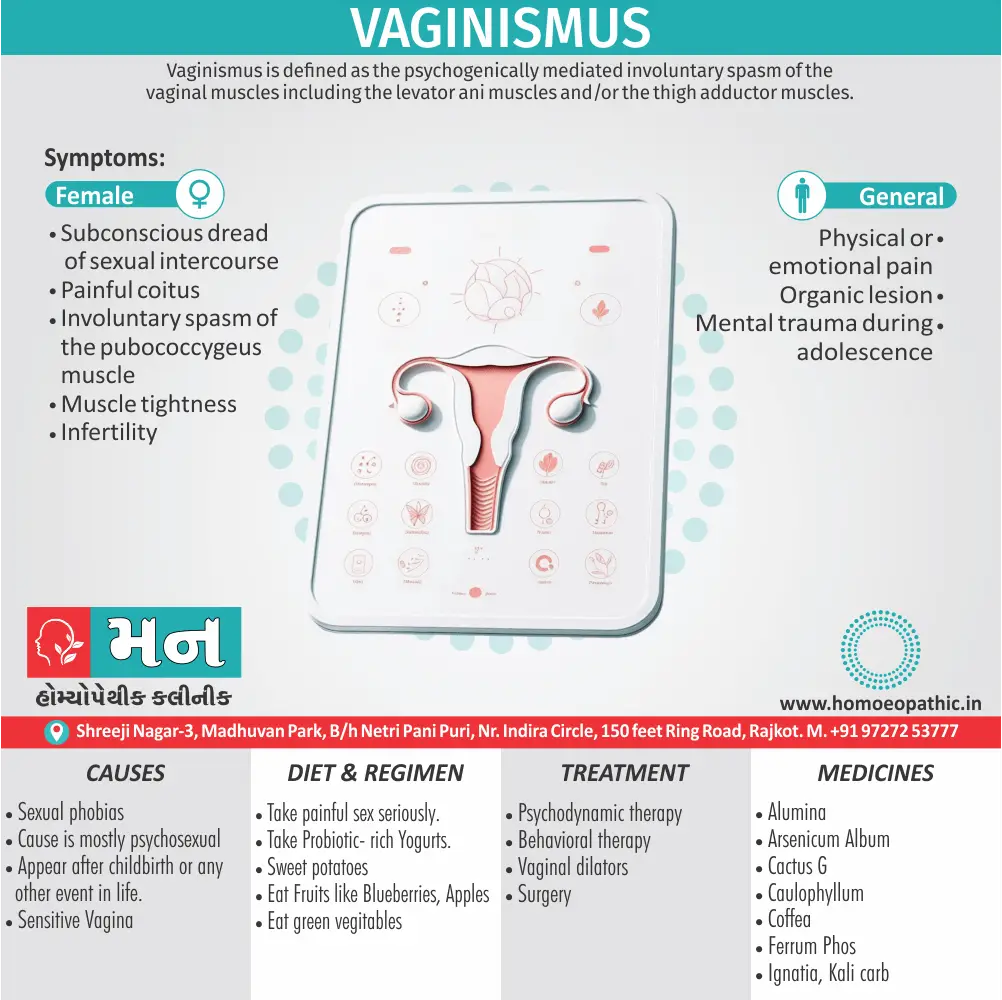
Vaginismus is defined as the psychogenically mediated involuntary spasm of the vaginal muscles including the levator ani muscles and/or the thigh adductor muscles. This results in inability of penetrative sexual intercourse. [1]
Vaginismus is a condition where the muscles around the vagina involuntarily tighten, causing pain and discomfort during sexual intercourse or other vaginal penetration. There isn’t a direct synonym for vaginismus, but it can be described in other ways:
Genito-pelvic pain/penetration disorder (GPPPD): This is a broader term that encompasses vaginismus and other conditions causing pain in the genital or pelvic area during sexual activity.
Vaginal muscle spasm: This describes the physical symptom of the muscles tightening.
Painful sexual intercourse: This is a more general term that could include vaginismus as a possible cause.
Please note that vaginismus is the most specific and accurate term for this condition.
Overview
Epidemiology
Causes
Risk Factors
Types
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview Vaginismus:
- Vaginismus is regarded as hyperaesthesia which leads to spasm of the sphincter vagina.
- There are two types of vaginismus.
- In primary vaginismus there is no organic lesion present.
- In secondary vaginismus some obvious painful lesion in the region of the genital tract can be found on examination.
- It is thus easy for organic dyspareunia to lead to a protective spasm in order to avoid the pain of coitus.
- Removal of the cause will cure this condition. [2]
Epidemiology
Epidemiology
While accurate statistics on the prevalence of vaginismus in India are limited, some studies suggest that it affects a significant portion of the female population. Here’s a summary of the epidemiology with references and publication years:
Bulbuli AS, Kokate VA. Prevalence of Vaginismus in Reproductive Age group: Observational Study. J South Asian Feder Obst Gynae 2024;16(2):198–201
- This study found that 28% of participants had primary vaginismus and 30% had secondary vaginismus.
Other estimates
- Some sources suggest that vaginismus may affect up to 5 to 17% of Indian women.
- There’s evidence suggesting a higher occurrence among those with limited access to sexual health education and judgment-free resources.
Key points to note:
- The stigma surrounding female sexuality in India can make it difficult for women to seek help, potentially leading to underreporting.
- More research is needed to obtain a clearer picture of the epidemiology of vaginismus in India.
It’s important to remember that these figures are estimates, and the actual prevalence may vary.[8]
Causes
Causes of Vaginismus:
Primary
- Nothing has entered into the woman’s vagina ever.
- The vagina is normal anatomically and physiologically.
- The cause is mostly psychosexual in origin.
- There is often presence of a subconscious fear of sexual intercourse (sexual phobias).
Secondary
- Vaginismus usually appear after childbirth or any other event in life.
- There is usually some local painful lesions.
- Such lesions include vulvitis, lacerations of the hymen, tender scar on the perineum or narrow vaginal introitus. [1]
Risk Factors
Risk factor of Vaginismus:
- Anxiety disorders.
- Childbirth injuries Like vaginal tears.
- Prior surgery.
- Fear of sex
- Negative feelings about sex
- Rape/trauma. [2]
Types
Types of Vaginismus:
- Primary Vaginismus
- Secondary Vaginismus
Pathogenesis
Pathogenesis of vaginismus
The development of vaginismus is a complex process, often involving an interplay of physical and psychological factors. It’s characterized by involuntary muscle contractions of the pelvic floor muscles surrounding the vaginal opening, making penetration painful or impossible.
Predisposing Factors: These create a vulnerability to developing vaginismus. Examples include:
- Early Life Experiences: Negative sexual messages, strict upbringing, or sexual trauma.
- Anxiety or Phobias: General anxiety disorders, or specific phobias related to sex or penetration.
- Relationship Issues: Poor communication, lack of trust, or history of sexual difficulties with a partner.
Precipitating Factors: These trigger the onset of vaginismus.
- Painful First Sexual Experience: This can create a fear response and lead to anticipatory anxiety about future sexual encounters.
- Medical Conditions: Infections, inflammation, or gynecological surgeries can cause pain, contributing to muscle tension and vaginismus.
- Stressful Life Events: Major life changes, relationship difficulties, or work-related stress can exacerbate anxiety and trigger vaginismus.
Perpetuating Factors: These factors maintain the cycle of vaginismus.
- Fear-Avoidance Cycle: Fear of pain leads to avoidance of sexual activity, which further reinforces the fear.
- Muscle Tension: Chronic muscle tension and guarding of the pelvic floor muscles can become habitual.
- Negative Cognitions: Catastrophic thoughts about sex and penetration can contribute to anxiety and muscle tension.
Understanding this complex pathogenesis allows for a more comprehensive approach to treatment, addressing both physical and psychological components.[9]
Pathophysiology
Pathophysiology of Vaginismus:
- Vaginismus is a psychogenic phenomenon that expresses itself by spasm of the muscle of the vagina.
- Starting with slight contraction at the beginning of intercourse, to extreme cases in which the spasm causes severe pain.
- Adduction of the thighs and opisthotonos and does not allow the introduction of the male sexual organ or even a fingertip into the vagina. [3]
Clinical Features
Clinical Features of Vaginismus
The clinical presentation of vaginismus can vary depending on the individual and the severity of the condition. However, some common features include:
- Painful or Impossible Penetration: This is the hallmark symptom of vaginismus. Women may experience pain or discomfort during any attempt at penetration, including sexual intercourse, gynecological exams, or tampon insertion.
- Involuntary Muscle Contraction: The primary physical manifestation is the involuntary tightening or spasm of the muscles surrounding the vaginal opening.
- Burning or Stinging Sensation: Some women may describe a burning or stinging sensation during attempted penetration.
- Fear or Anxiety: Due to the anticipation of pain, many women with vaginismus experience fear or anxiety related to sexual activity or gynecological examinations.
- Avoidance of Sexual Activity: To avoid the pain and discomfort associated with penetration, women may avoid or limit sexual activity altogether.
- Relationship Difficulties: The inability to engage in sexual intercourse can strain relationships and lead to emotional distress for both partners.
This handbook extensively explores the clinical aspects of vaginismus, emphasizing the following:
- The pain experienced can range from mild discomfort to severe, sharp pain.
- The involuntary muscle contractions can be so strong that penetration is physically impossible.
- The fear and anxiety associated with vaginismus can be debilitating and lead to significant distress.
- The condition can negatively impact a woman’s self-esteem, body image, and overall quality of life.
Understanding these clinical features is crucial for accurate diagnosis and the development of effective treatment plans that address both the physical and psychological aspects of vaginismus.[10]
Sign & Symptoms
Sign & Symptoms of Vaginismus
- Involuntary spasm of the pubococcygeus muscle.
- Muscle tightness
- Physical or emotional pain.
- Organic lesion
- Mental trauma during adolescence
- Subconscious dread of sexual intercourse.
- Painful coitus
- Infertility. [2]
Clinical Examination
Clinical Examination of Vaginismus
The clinical examination for vaginismus involves a careful and sensitive approach to assess both the physical and psychological aspects of the condition. It’s crucial to establish trust and rapport with the patient to ensure a comfortable and informative experience.
Key Components of the Examination:
- Detailed History: A thorough discussion about the patient’s medical, sexual, and psychological history is essential. This includes:
- Onset and duration of symptoms.
- Specific triggers or situations that worsen the pain or muscle contractions.
- Impact on sexual function and quality of life.
- Previous treatments or interventions.
- Any history of trauma, abuse, or negative sexual experiences.
- Physical Examination: A gentle and respectful physical examination is conducted to assess the pelvic floor muscles and rule out other potential causes of pain. This may involve:
- External examination of the vulva and surrounding areas.
- Internal examination using a single finger or a small speculum, if tolerated by the patient.
- Assessment of muscle tone and tenderness in the pelvic floor muscles.
- Observation of any involuntary muscle contractions during attempted penetration or touch.
- Psychological Assessment: A brief psychological assessment can help identify any anxiety, fear, or negative beliefs related to sex or penetration.
This book highlights the importance of a comprehensive approach to the clinical examination of vaginismus, emphasizing:
- The need for a relaxed and supportive environment.
- The use of clear communication and explanations throughout the examination.
- The option to stop or modify the examination at any time if the patient experiences discomfort.
- The referral to a mental health professional if psychological factors are contributing to the condition.
Remember:
- The clinical examination should be tailored to the individual patient’s needs and comfort level.
- The goal is to obtain a clear understanding of the patient’s symptoms and develop an appropriate treatment plan.
- A multidisciplinary approach involving both medical and psychological professionals often yields the best outcomes.[11]
Diagnosis
Diagnosis of Vaginismus
- While diagnosis of the secondary one is not so difficult but to find out the cause of the primary one, examination under anesthesia may be required.
- If the two fingers can be easily introduced through the vaginal introitus, the calibre of the vagina is proved normal. [1]
Differential Diagnosis
Differential Diagnosis of Vaginismus
While vaginismus presents with distinct clinical features, it’s crucial to consider other potential causes of pain or difficulty with penetration. A thorough differential diagnosis ensures accurate identification and appropriate management.
Possible differential diagnoses include:
- Vulvodynia: Chronic vulvar pain without an identifiable cause.
- Vestibulodynia: Pain localized to the vestibule (entrance) of the vagina.
- Infections: Vaginal or urinary tract infections can cause pain or discomfort.
- Inflammation: Conditions like lichen sclerosus or atrophic vaginitis can lead to inflammation and pain.
- Endometriosis: Endometrial tissue growth outside the uterus can cause pelvic pain, sometimes affecting intercourse.
- Pelvic floor dysfunction: Tight or overactive pelvic floor muscles can contribute to pain and difficulty with penetration.
- Psychological factors: Anxiety, depression, or past trauma can contribute to or exacerbate sexual difficulties.[9]
Complications
Complications of Vaginismus
While vaginismus primarily manifests as pain or difficulty with penetration, its impact can extend beyond the physical realm, affecting various aspects of a woman’s life.
Potential complications include:
- Sexual Dysfunction: Vaginismus can lead to difficulties or complete inability to engage in sexual intercourse, impacting sexual satisfaction and intimacy.
- Relationship Difficulties: The inability to have intercourse can strain relationships and create feelings of frustration, guilt, or inadequacy for both partners.
- Emotional Distress: The persistent pain, fear, and anxiety associated with vaginismus can lead to depression, anxiety disorders, and decreased self-esteem.
- Fertility Challenges: For couples trying to conceive, vaginismus can make achieving pregnancy difficult or impossible without medical intervention.
- Gynecological Examination Challenges: The fear and anticipation of pain can make routine gynecological exams or procedures incredibly distressing and difficult to complete.
- Reduced Quality of Life: The cumulative impact of physical, emotional, and relational difficulties can significantly reduce a woman’s overall quality of life.
This book delves into the broader implications of vaginismus, stating that the condition can:
- "Lead to sexual avoidance and dissatisfaction."
- "Contribute to relationship problems and marital discord."
- "Result in psychological distress, including anxiety and depression."
- "Create difficulties with fertility and conception."
- "Interfere with routine gynecological care."
It’s essential to recognize the potential complications of vaginismus and seek timely treatment to prevent long-term negative consequences.
Remember:
- The impact of vaginismus can be significant, affecting physical, emotional, and relational well-being.
- Early intervention and comprehensive treatment can help manage the condition and minimize complications.
- Support from healthcare professionals, therapists, and partners is crucial in navigating the challenges associated with vaginismus.[12]
Investigations
Investigation of Vaginismus
- Psychosexual History: Diagnosis begins with a comprehensive psychosexual history. Understanding the patient’s experiences, distress levels, anxiety, and self-reported difficulties with penetration is crucial.
- Distress and Anxiety: The degree of distress and anxiety related to penetration is more central to the diagnosis than muscle tone. Patients often experience fear, anticipation, and pain associated with attempted penetration.
- Genital Examination: At some point during the evaluation, a genital examination may be necessary to exclude any organic pathology. This examination helps rule out physical disorders that might contribute to vaginismus.
- Holistic Approach: Information on sexual function and pelvic anatomy should be provided to all patients. Treatment options, such as using “vaginal trainers” of gradually increasing size, can help achieve penetrative intercourse. [5]
Treatment
Treatment of Vaginismus
Primary
- Psychodynamic therapy: Main causes of fear are removed.
- To educate and to gain confidence of the couple.
- This may take time.
- Behavioral therapy: Dilatation of the vaginal introitus digitally followed by introduction of gradually increasing size of the dilators is to be done.
- Plastic vaginal trainers (Pseudopenises) with graduated sizes can help her to remove her fear.
- This will gain her confidence that her vagina is anatomically of normal caliber.
- Vaginal dilators: Daily introduction of the dilators (pseudopenises) for 1–2 weeks and to keep it inside for 10–15 minutes is enough before she is allowed to attempt coital act.
- Surgery: A classic case of vaginismus needs no surgery.
- However, surgery may be required, if the hymen is found tight hymenectomy or Fenton’s operation (operation to enlarge the introitus), if the introitus is narrow.
Secondary
- The local lesion is to be treated medically or surgically. [1]
Prevention
Prevention of Vaginismus
- Give information about genital anatomy and the female sexual response
- Individual therapy to explore and resolve predisposing factors
- Couple therapy where couples collude to maintain the problem
- Gradual desensitization using such items as fingers, tampon covers, specifically designed vaginal Amielle dilators – plus plenty of synthetic lubrication.
- Gradually move to penile penetration with the woman maintaining control. [4]
Homeopathic Treatment
Homoeopathic Treatment of
Vaginismus :
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
- A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
- The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
- The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines :
- The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
- So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines
1. Alumina:
- Stitches in left side of vulva, extending as far as chest; beating, throbbing pain in vagina.
2. Arsenicum album:
- Lancinations from abdomen into vagina; burning as if hot coals were in vagina, preventing sleep.
3. Cactus G:
- Constriction of vagina, preventing coition, being brought on by merely touching the oversensitive parts, but going off in a few minutes.
4. Caulophyllum:
- Excessively irritable vagina; intense and continued pain and spasms; aphthous vaginitis and spasmodic pains in uterus; burning leucorrhoea with weakness and exhaustion.
5. Coffea:
- Oversensitiveness of vagina; aversion to intercourse on account of pain it produces.
6. Ferrum Phos:
- Pain in vagina during coition or vaginal examination.
7. Ignatia:
- Intense sore pain at entrance of vagina during coition; acute darting pain in vulva, only during day; constant burning heat in vagina, (<) before menses; great dysmenia before and after menses; hysteria.
8. Kali Carb:
- Persistent and severe constriction of vagina; pinching pain in vagina during embrace; itching of vulva.[6]
Diet & Regimen
Diet and Regimen
For Vaginismus
Diet:
- Hydration is Key: Staying well-hydrated helps with natural lubrication, which can make any kind of vaginal entry more comfortable. Aim for plenty of water throughout the day.
- Focus on Gut Health: A healthy gut microbiome is linked to overall health, including vaginal health. Consider incorporating:
- Probiotic-rich foods: Yogurt, kefir, sauerkraut, kimchi
- Prebiotic foods: These feed the good bacteria in your gut. Examples include onions, garlic, bananas, and asparagus.
- Probiotic-rich foods: Yogurt, kefir, sauerkraut, kimchi
- Reduce Inflammatory Foods: While research is limited, some experts suggest that reducing inflammatory foods might help with pelvic pain in general. This could include limiting processed foods, sugary drinks, and excessive red meat.
Regimen:
- Pelvic Floor Exercises: These are crucial! Think of them as physical therapy for your pelvic floor muscles. They help you:
- Gain awareness: Learn to identify and isolate those muscles.
- Improve control: Learn to consciously relax and contract the muscles, which is key to overcoming involuntary spasms.
- Increase strength and flexibility: This can reduce pain and improve overall pelvic floor function.
- Resources: Look for resources like books, videos, or apps that guide you through pelvic floor exercises. A pelvic floor physical therapist can provide personalized instruction.
- Mindfulness and Meditation: Even a few minutes a day can make a difference.
- Deep Breathing Exercises: Practice diaphragmatic breathing to calm your nervous system.
- Yoga: Combines physical postures with breathwork and mindfulness.
Stress Management is Essential: Stress and anxiety are major triggers for vaginismus. Incorporate relaxation techniques into your daily routine:
- Prioritize Sleep: Adequate sleep is crucial for physical and emotional well-being, both of which impact vaginismus.
- Hydration is Key: Staying well-hydrated helps with natural lubrication, which can make any kind of vaginal entry more comfortable. Aim for plenty of water throughout the day.
Do’s and Don'ts
Do’s and Don’ts
Vaginismus Do’s and Don’ts
Do’s
- Seek professional help: Consult a healthcare professional specializing in sexual health or pelvic floor dysfunction. They can provide a diagnosis, educate you about the condition, and recommend appropriate treatment options.
- Educate yourself: Learn as much as you can about vaginismus from reliable sources. Understanding the condition can help reduce fear and anxiety.
- Communicate with your partner: Open communication with your partner about your condition is crucial. It fosters understanding, support, and helps explore alternative forms of intimacy.
- Practice relaxation techniques: Techniques like deep breathing, meditation, and mindfulness can help reduce stress and anxiety, which can worsen vaginismus symptoms.
- Engage in pelvic floor physical therapy: A pelvic floor physical therapist can teach you exercises and techniques to relax and control your pelvic floor muscles.
- Consider therapy or counseling: Cognitive-behavioral therapy (CBT) or sex therapy can help address the psychological aspects of vaginismus, such as anxiety, fear, or past trauma.
- Use dilators: Gradual desensitization using vaginal dilators can help you become more comfortable with penetration and reduce muscle tension.
- Be patient and persistent: Treatment for vaginismus takes time and effort. Be patient with yourself and celebrate small victories along the way.
- Maintain a healthy lifestyle: Regular exercise, a balanced diet, and adequate sleep contribute to overall well-being and can help manage stress and anxiety.
Don’ts
- Don’t feel ashamed or embarrassed: Vaginismus is a common condition, and it’s not your fault. Don’t hesitate to seek help.
- Not force penetration: Trying to force penetration can worsen pain and anxiety, making the condition more challenging to treat.
- Don’t rush treatment: Give yourself time to heal and progress at your own pace.
- Don’t isolate yourself: Talk to your partner, trusted friends, or a therapist about your feelings and concerns.
- Not give up on intimacy: Explore alternative ways to express intimacy with your partner, such as cuddling, massage, or oral sex.
Terminology
Terminology
Vaginismus: The involuntary tightening or spasm of the muscles surrounding the vaginal opening, making penetration painful or impossible.
Pelvic Floor Muscles: The group of muscles that support the pelvic organs, including the bladder, uterus, and rectum. They also play a role in sexual function.
Dyspareunia: Painful sexual intercourse. Vaginismus is a specific type of dyspareunia.
Penetration: The insertion of an object into the vagina, such as a penis, finger, tampon, or speculum.
Involuntary Muscle Contraction: The tightening of the muscles without conscious control. In vaginismus, this happens in the pelvic floor muscles during attempted penetration.
Anticipatory Anxiety: Anxiety or fear experienced before a situation, such as in anticipation of sexual activity or a gynecological exam.
Phobia: An intense and irrational fear of a specific object or situation.
Trauma: A deeply distressing or disturbing experience.
Dilators: Smooth, graduated objects used to gently stretch the vaginal opening and help women with vaginismus become more comfortable with penetration.
Pelvic Floor Physical Therapy: Specialized physical therapy that focuses on relaxing and strengthening the pelvic floor muscles.
Cognitive-Behavioral Therapy (CBT): A type of therapy that helps individuals identify and change negative thoughts and behaviors.
Sex Therapy: A type of therapy that focuses on addressing sexual problems and improving sexual function.
Multidisciplinary Approach: An approach to treatment that involves multiple healthcare professionals, such as gynecologists, physical therapists, and mental health professionals.
Other related terms that may be encountered include:
Vulvodynia: Chronic vulvar pain without an identifiable cause.
Vestibulodynia: Pain localized to the vestibule (entrance) of the vagina.
Genito-Pelvic Pain/Penetration Disorder (GPPPD): A broader diagnostic category that includes vaginismus and other conditions causing pain with sexual activity or penetration.
References
References
- DC Dutta’s Textbook of Gynecology.
- Gynacology VG Padubidri.
- The Pathophysiology and Etiology of Vaginismus – ScienceDirect
- Dewhurst_s_Textbook_of_Obstetrics_and_Gynaecology_7th_ed
- 186284 (bmj.com)
- Persistent and severe constriction of vagina; pinching pain in vagina during embrace; itching of vulva.
- How to Cope with Vaginismus (with Pictures) – wikiHow
- Bulbuli AS, Kokate VA. Prevalence of Vaginismus in Reproductive Age group: Observational Study. J South Asian Feder Obst Gynae 2024;16(2):198–201
- Textbook of Female Sexual Function and Dysfunction: Diagnosis and Treatment" (2nd Edition), Irwin Goldstein, Cindy Meston, Susan Davis, Lori Brotto, 2013, CRC Press.
- Handbook of Sexual Dysfunction in Women: Assessment and Treatment, Sandra R. Leiblum, Raymond C. Rosen, 2006, The Guilford Press.
- Female Sexual Pain Disorders: Evaluation and Management, Andrew Goldstein, Irwin Goldstein, Caroline Pukall, 2009, Informa Healthcare.
- Women’s Sexual Health (2nd Edition), Sheryl A. Kingsberg, Carolyn M. Clancy, 2010, Jones & Bartlett Learning.
Also Search As
Also search as
Online Search Engines:
Use specific keywords:
"Vaginismus homeopathy"
"Homeopathic treatment for vaginismus"
"Homeopathic remedies for vaginismus"
"Vaginismus case studies homeopathy"
Include additional search terms:
"Research"
"Articles"
"Studies"
"Journals"
Use advanced search operators:
filetype:pdf (to find PDF articles)
site:.edu or site:.org (to focus on academic or organizational websites)
Homeopathic Databases and Journals
Search within reputable homeopathic databases and journals, such as:
The American Journal of Homeopathic Medicine
Homeopathy (journal)
The National Center for Homeopathy
The British Homeopathic Association
Homeopathic Practitioner Websites and Blogs
Many homeopathic practitioners have websites or blogs where they share information and articles. Search for practitioners specializing in women’s health or sexual dysfunction.
Social Media and Forums
Search on social media platforms (Facebook, Twitter, etc.) or homeopathic forums for discussions and articles on vaginismus.
Libraries
Visit your local library or university library and search their catalog or databases for homeopathic books and journals related to vaginismus.
Tips:
Be specific in your search terms.
Use a variety of search methods.
Evaluate the credibility of the sources you find.
Consult a qualified homeopathic practitioner for personalized advice and treatment.
Frequently Asked Questions (FAQ)
What is vaginismus?
Vaginismus is a condition where the muscles around the vaginal opening involuntarily tighten or spasm, making penetration painful or impossible.
What causes vaginismus?
Vaginismus often stems from a combination of physical and psychological factors, including past trauma, anxiety, relationship issues, or negative sexual experiences.
Can vaginismus be cured ?
Yes, vaginismus is treatable. With appropriate therapy and support, most women can overcome the condition and enjoy a healthy sexual life.
What are the symptoms of vaginismus?
The primary symptom is pain or difficulty with penetration. Other symptoms may include burning, stinging, muscle tightness, and anxiety related to sexual activity.
How is vaginismus diagnosed?
Diagnosis involves a thorough medical and sexual history, a gentle physical examination, and potentially a psychological assessment.
Can homeopathy help with vaginismus?
Explore the potential benefits of homeopathy for vaginismus, including addressing the physical and emotional aspects of the condition.
What homeopathic remedies are used for vaginismus
Discover commonly used homeopathic remedies for vaginismus and their potential actions on the physical and emotional symptoms.
What homeopathic remedies are used for vaginismus
Discover commonly used homeopathic remedies for vaginismus and their potential actions on the physical and emotional symptoms.
Is homeopathic treatment for vaginismus safe?
Understand the safety profile of homeopathic remedies and the importance of consulting a qualified practitioner for personalized treatment.
