Mood Disorders
Definition:
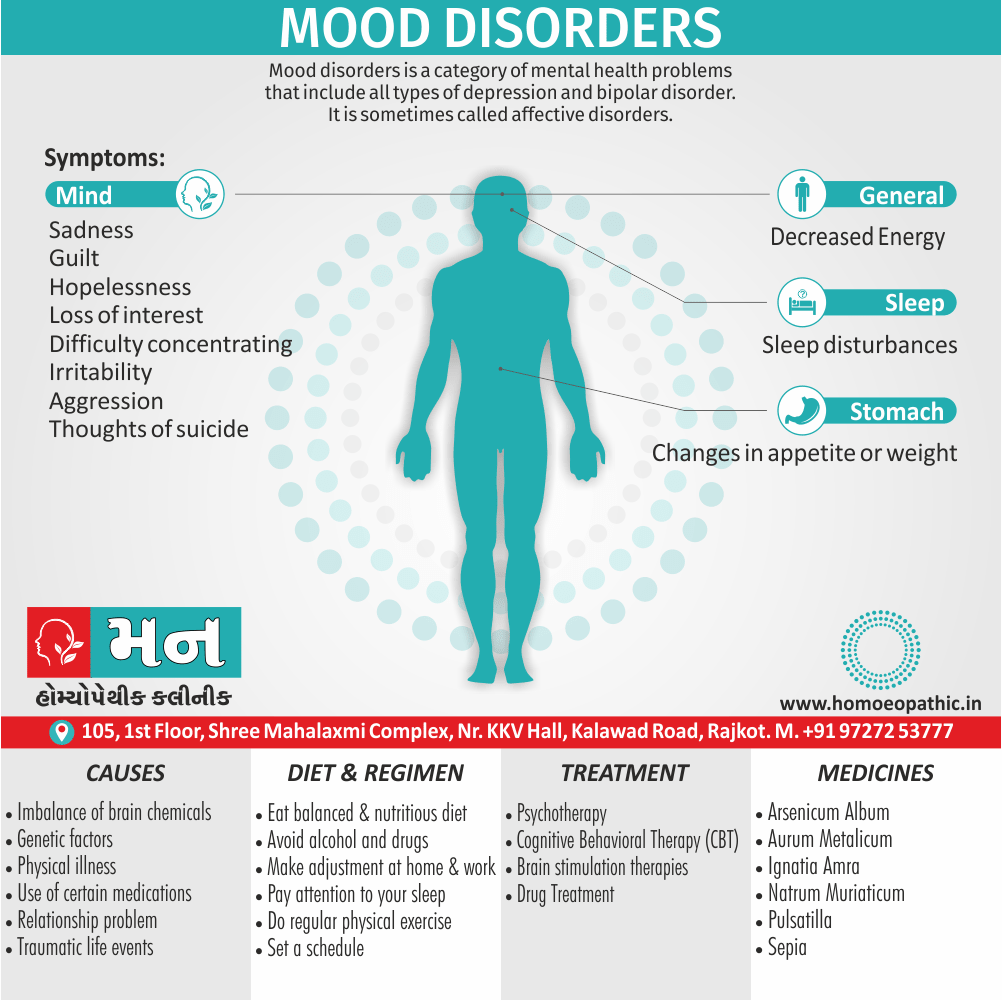
Mood disorders is a category of mental health problems that include all types of depression and bipolar disorder. Additionally, It is sometimes called affective disorders.
There are several synonyms for mood disorder, some more clinical and some more general. Here are a few options:
- Affective disorder: This is a more technical term for mood disorder, and it is used in the Diagnostic and Statistical Manual of Mental Disorders (DSM) .
- Emotional disorder: This is a more general term that can refer to any condition that affects a person’s emotions.
- Bi-polar disorder: This is a specific type of mood disorder that is characterized by episodes of mania (elevated mood) and depression (low mood).
- Major depressive disorder: This is another specific type of mood disorder that is characterized by persistent feelings of sadness or hopelessness.
It’s important to note that some of the more general synonyms for mood disorder, such as "craziness" or "lunacy," can be stigmatizing. It’s best to use more clinical terms or more specific terms to describe the type of mood disorder that someone is experiencing.
Frequently Asked Questions (FAQ)
Overview
Epidemiology
Causes
Risk Factors
Pathogenesis
Pathophysiology
Types
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Mood Disorder:
During the 1980, mental health professionals began to recognize symptoms of mood disorders in children and adolescents, as well as adults.
However, children and adolescents do not necessarily experience or exhibit the same symptoms as adults. It is more difficult to diagnose mood disorders in children, especially because children are not always able to express how they feel.
Today, clinicians also researchers believe that mood disorders in children and adolescents remain one of the most under-diagnosed mental health problems.
At any age, mood disorders put individuals at risk for other conditions, that may persist long after, the initial episodes of depression resolved
Epidemiology
Epidemiology of Mood disorders
The National Mental Health Survey of India (2015-16) provides a comprehensive overview of the prevalence and patterns of mood disorders in the country. It found that:
- The prevalence of any mood disorder was 2.7%, with depressive disorders being the most common (2.1%).
- Mood disorders were more prevalent in females (3.0%) than in males (2.4%).
- The prevalence of mood disorders increased with age, peaking in the 40-49 age group.
- Urban residents had a slightly higher prevalence of mood disorders (2.8%) compared to rural residents (2.6%). [2]
Reference:
- National Mental Health Survey of India, 2015-16. Ministry of Health and Family Welfare, Government of India.
Another study, "Prevalence and socioeconomic impact of depressive disorders in India: multisite population-based cross-sectional study" (published in 2019) provides further insights:
- The prevalence of current depressive disorder was 4.7%, while the lifetime prevalence was 10.6%.
- Females (5.3%) were more likely than males (3.9%) to have current depressive disorder.
- Depressive disorders were associated with significant disability, impaired quality of life, and economic burden. [3]
Reference:
- Gururaj, G., Varghese, M., Benegal, V., & others. (2019). Prevalence and socioeconomic impact of depressive disorders in India: multisite population-based cross-sectional study.
Please note that these are just a few examples of the available research on the epidemiology of mood disorders in India. The exact prevalence rates and patterns can vary depending on the study methodology and population sampled.
Causes
Causes
What causes mood disorders is not well known.
- Basically, mood disorders are chemicals in the brain, call endorphins that are responsible for positive moods.
- Other chemicals in the brain, called neurotransmitters, regulate endorphins.
- Most likely, depression ( and other )mood disorders is cause by a chemical imbalance in the brain.
- Life events (such as unwanted changes in life) may also contribute to a depressed mood.
- Affective disorders aggregate in families also considered to be multifactorial inherited.
- Multi-factor inheritance means that "many factors" are involved. Additionally, The factors are usually both genetic and environmental, where a combination of genes from both parents, in addition to unknown environmental factors, produces the trait or condition.
- Often one gender (either male or female) affected more frequently than the other in multi-factor traits.
- There appears to be a different threshold of expression, which means that one gender is more likely to show the problem, over the other gender.
Risk Factors
Risk factors of Mood Disorders
- Anyone can feel sad or depressed at times. However, mood disorders are more intense also difficult to manage than normal feelings of sadness.
- Children, adolescents, or adults who have a parent with a mood disorder have a greater chance of also having a mood disorder.
- However, life, events and stress can expose or exaggerate feelings of sadness or depression, making the feelings more difficult to manage .
- Sometimes, life’s problems can trigger depression. In detail, Being fired from a job, getting divorced, losing a loved one, death in the. family, also , financial trouble, to name a few, all can be difficult also coping with the pressure may be troublesome.
- These life events and stress can bring on feelings of either sadness or depression or make a mood disorder harder to manage.
Other factors
- The chance for depression in females in the general population is nearly twice as high (12 per cent) as it is for males (6.6 per cent). Once a person in the family has this diagnosis, the chance for their siblings or children to have the same diagnosis is increase.
- In addition, relatives of persons with depression are also at increase risk for bipolar disorder (excited depression).
- The chance for excited depression ( or bipolar disorder) in males and females in the general population is about 1 per cent. Once a person in the family has this diagnosis, the chance for their siblings or children to have the same diagnosis increased. In addition, relatives of persons with wild depression are also at increased risk for depression.
Pathogenesis
Pathogenesis of Mood Disorder
The pathogenesis of mood disorders is complex and multifactorial, involving interactions between genetic, biological, environmental, and psychological factors.
There is no single definitive reference that covers all aspects comprehensively, but here are two highly regarded books that delve into the topic in depth:
- The American Psychiatric Association Publishing Textbook of Mood Disorders (Second Edition)
- Editors: Charles B. Nemeroff, Alan F. Schatzberg, Natalie Rasgon, Stephen M. Strakowski
- Year of Publication: 2022
- Publisher: American Psychiatric Association Publishing
This textbook provides a comprehensive overview of mood disorders, including their epidemiology, genetics, neurobiology, and treatment. It covers major depressive disorder and bipolar disorder extensively, exploring their underlying mechanisms and potential therapeutic targets. [4]
- Kaplan & Sadock’s Comprehensive Textbook of Psychiatry (Tenth Edition)
- Editors: Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz
- Year of Publication: 2017
- Publisher: Wolters Kluwer
This comprehensive textbook covers a wide range of psychiatric disorders, including mood disorders. It provides detailed information on the etiology, clinical presentation, diagnosis, and treatment of various mood conditions, drawing upon a wealth of research and clinical experience. [5]
Both of these books offer valuable insights into the pathogenesis of mood disorders, albeit with different focuses and approaches. The APA Textbook specifically targets mood disorders, while Kaplan & Sadock’s offers a broader perspective within the context of general psychiatry.
Pathophysiology
Pathophysiology of Mood Disorders
- Neurotransmitter systems: The roles of serotonin, norepinephrine, dopamine, glutamate, and GABA in mood regulation.
- Neuroendocrine systems: The hypothalamic-pituitary-adrenal (HPA) axis and its dysregulation in mood disorders.
- Neurocircuitry: The brain regions and neural pathways implicated in the development and maintenance of mood disorders.
- Genetics: The genetic contributions to mood disorders and the interaction between genes and environment.
- Neuroinflammation: The role of inflammation in mood disorders and its potential as a therapeutic target. [6]
Types
Types of Mood disorders
The following are the most common types of mood disorders:
1. Major depression: a two week period of a either depressed or irritable mood or a noticeable decrease in interest or pleasure in usual activities, along with other signs of a mood disorder.
2. Dysthymia (in other words, dysthymic disorder): chronic, low-grade, depressed or irritable mood for at least one year.
3. Excited depression (in other words, bipolar disorder) at least one episode of a depressed or irritable mood and at least one period of a maniacal (persistently elevated) mood.
4. Mood disorder due to a general medical condition-many medical illnesses (for example; cancer, injuries, infections, and chronic medical illnesses) can trigger symptoms of depression.
5. Substance induced mood disorder-symptoms of depression that are due to the effects of medication, drug abuse, exposure to toxins, or other forms of treatment.
The classification of affective disorders in ICD-10 and DSM-IV:
ICD-10 | DSM-IV |
| unbalanced episode | wild episode |
Depressive episode Major Moderate Severe | Major depressive episode |
| Bi-polar affective disorder | Bi-polar disorders |
| Persistent mood (affective) states | |
| Cyclothymia | Cyclothymia |
| Dysthymia | Dysthymia |
Clinical Features
Clinical Features of Mood Disorders
- Major Depressive Disorder: Persistent sadness or loss of interest in activities, along with other symptoms such as changes in sleep, appetite, energy levels, concentration, and feelings of worthlessness or guilt.
- Bi-polar I Disorder: Episodes of mania (elevated or irritable mood, increased energy, racing thoughts, impulsive behavior) alternating with episodes of major depression.
- Bi-polar II Disorder: Episodes of hypomania (less severe form of mania) alternating with episodes of major depression.
- Persistent Depressive Disorder (Dysthymia): Chronic depressed mood lasting for at least two years, along with other symptoms such as changes in appetite, sleep, and energy levels.
- Cyclothymic Disorder: Chronic fluctuations between hypomanic and depressive symptoms, but not meeting the criteria for full-blown episodes of mania or major depression.
- Other Specified or Unspecified Bi-polar and Related Disorder: Mood disturbances that cause significant distress or impairment, but do not meet the full criteria for any of the above disorders. [7]
Sign & Symptoms
Sign & Symptoms of Mood disorders
Depending upon age also the type of mood disorder present, a person may exhibit different symptoms of depression. The following are the most common symptoms of a mood disorder. However, each individual may experience symptoms differently.
Symptoms may include:
1. Persistent feelings of sadness.
2. Feeling either hopeless or helpless.
3. Having low self-esteem.
4. Feeling inadequate.
5. Excessive guilt.
6. Feelings of wanting to die.
7. Loss of interest in usual activities or activities once enjoyed.
8. Difficulty with relationships.
9. Sleep disturbances (i.e., insomnia, hypersomnia).
10. Changes in appetite or weight.
11. Decreased energy.
12. Difficulty concentrating.
13. A decrease in the ability to make decisions.
14. Either Suicidal thoughts or attempts.
Other Symptoms:
15. Frequent physical complaints (i.e., headache, stomach ache, fatigue).
16. Running away or threats of running away from home.
17. Hypersensitivity to either failure or rejection.
18. Irritability, hostility, aggression.
19. In mood disorders, these feelings appear more intense than what a person may normally feel from time to time.
20. It is also of concern if these feelings continue over a period of time, or interferes with an individual’s interest in family, friends, community, or work.
21. Any person who expresses thoughts of suicide should be evaluated immediately.
22. The symptoms of mood disorders may resemble other conditions or psychiatric problems. In detail, Physician should make proper diagnosis for that.
Clinical Examination
Clinical Examination
The clinical examination of mood disorders is a multifaceted process that involves a thorough assessment of the patient’s history, mental state, and physical health.
- History taking: Eliciting information about the patient’s current symptoms, past psychiatric history, family history, medical history, and social history.
- Mental state examination (MSE): Assessing the patient’s appearance, behavior, mood, affect, speech, thought process, thought content, perception, cognition, and insight.
- Risk assessment: Evaluating the patient’s risk of suicide, self-harm, and harm to others.
- Physical examination: Screening for medical conditions that may contribute to or mimic mood disorders. [8]
Diagnosis
Diagnosis
The DSM-5-TR provides comprehensive diagnostic criteria and guidelines for various mood disorders, including:
- Major Depressive Disorder (MDD): Characterized by a persistent depressed mood or loss of interest in activities, along with other symptoms like changes in sleep, appetite, energy levels, and concentration.
- Bi-polar I Disorder: Characterized by manic episodes (elevated or irritable mood, increased energy, racing thoughts, impulsive behavior) alternating with major depressive episodes.
- Bi-polar II Disorder: Characterized by hypomanic episodes (less severe form of mania) alternating with major depressive episodes.
- Persistent Depressive Disorder (Dysthymia): Characterized by a chronic depressed mood lasting for at least two years, with additional symptoms like changes in appetite, sleep, and energy.
- Cyclothymic Disorder: Characterized by chronic fluctuations between hypomanic and depressive symptoms, but not meeting full criteria for mania or major depression.
- Premenstrual Dysphoric Disorder (PMDD): Characterized by mood swings, irritability, and other symptoms that occur in the week before menstruation.
The DSM-5-TR also includes diagnostic criteria for other specified and unspecified mood disorders, which are diagnosed when a person’s symptoms cause significant distress or impairment but do not meet the full criteria for any of the specific mood disorders listed above.
In addition to the DSM-5-TR, clinicians may also refer to other resources to aid in the diagnosis of mood disorders, such as:
- International Classification of Diseases (ICD-11): A globally recognized classification system for all diseases, including mental disorders.
- Clinical interviews: Structured or semi-structured interviews designed to assess a person’s mood and other symptoms.
- Rating scales: Standardized questionnaires used to quantify the severity of a person’s mood symptoms. [7]
Differential Diagnosis
Differential Diagnosis of Mood disorders
- Major Depressive Disorder (MDD): Differentiating MDD from other mood disorders, medical conditions (e.g., hypothyroidism), and substance-induced disorders.
- Bi-polar Disorder: Distinguishing between bi-polar I and bi-polar II disorders, as well as other conditions with mood fluctuations (e.g., cyclothymic disorder, borderline personality disorder).
- Persistent Depressive Disorder (Dysthymia): Differentiating dysthymia from MDD, adjustment disorder with depressed mood, and personality disorders.
- Other Mood Disorders: Exploring differential diagnoses for conditions like premenstrual dysphoric disorder, substance/medication-induced mood disorders, and mood disorders due to another medical condition. [5]
Complications
Complications of Mood disorders
- Suicide: Mood disorders, particularly major depressive disorder and bipolar disorder, significantly increase the risk of suicide. The book discusses the risk factors, warning signs, and prevention strategies for suicide in individuals with mood disorders.
- Substance Use Disorders: People with mood disorders are at higher risk of developing substance use disorders as a form of self-medication or due to shared underlying vulnerabilities. The book explores the complex relationship between mood disorders and substance abuse.
- Anxiety Disorders: Co-occurring anxiety disorders are common in individuals with mood disorders, and can exacerbate the symptoms and impair functioning. The book discusses the diagnosis and management of anxiety disorders in the context of mood disorders.
- Physical Health Problems: Mood disorders can increase the risk of various physical health problems, such as cardiovascular disease, diabetes, and chronic pain. The book explores the bidirectional relationship between mood disorders and physical health.
- Cognitive Impairment: Mood disorders can affect cognitive function, including attention, memory, and executive functions. The book discusses the assessment and management of cognitive impairment in individuals with mood disorders.
- Social and Occupational Impairment: Mood disorders can significantly impact a person’s relationships, work, and overall quality of life. The book explores the social and occupational consequences of mood disorders and strategies for improving functioning. [5]
Investigations
Investigations of Mood disorders
Including:
Clinical Assessment:
- Detailed history: A thorough psychiatric history, including the onset, duration, and severity of symptoms, past psychiatric and medical history, family history, and social history.
- Mental status examination (MSE): A systematic assessment of the patient’s appearance, behavior, mood, affect, speech, thought process, thought content, perception, cognition, and insight.
- Rating scales: Standardized questionnaires such as the Beck Depression Inventory (BDI) or Hamilton Rating Scale for Depression (HAM-D) can be used to quantify the severity of depressive symptoms.
Laboratory Tests:
- Complete blood count (CBC): To rule out anemia, infection, or other hematological conditions.
- Thyroid function tests (TFTs): To rule out hypothyroidism or hyperthyroidism, which can present with mood symptoms.
- Liver function tests (LFTs): To assess liver function and rule out any liver disease that could contribute to mood disturbance.
- Renal function tests (RFTs): To assess kidney function and rule out any kidney disease that could contribute to mood disturbance.
- Electrolyte levels: To assess for electrolyte imbalances, which can sometimes present with mood symptoms.
- Vitamin B12 and folate levels: To rule out deficiencies that can cause fatigue and mood changes.
- Toxicology screen: To rule out substance abuse as a contributing factor to mood disturbance.
- Neuroimaging: In some cases, brain imaging studies like MRI or CT scan may be indicated to rule out neurological conditions that can mimic mood disorders. [9]
Treatment
Treatment of Mood Disorders
- Pharmacotherapy: Detailed information on antidepressant medications (SSRIs, SNRIs, TCAs, MAOIs), mood stabilizers (lithium, anticonvulsants), antipsychotics, and other medications used in the treatment of mood disorders. The book covers the mechanisms of action, efficacy, side effects, and drug interactions of these medications.
- Psychotherapy: In-depth discussion of various psychotherapeutic approaches, such as cognitive-behavioral therapy (CBT), interpersonal psychotherapy (IPT), psychodynamic therapy, and family-focused therapy. The book explains the theoretical basis, techniques, and evidence base for these therapies.
- Brain Stimulation Therapies: Comprehensive overview of electroconvulsive therapy (ECT), transcranial magnetic stimulation (TMS), vagus nerve stimulation (VNS), and deep brain stimulation(DBS). The book covers the indications, procedures, efficacy, and side effects of these treatments.
- Lifestyle Interventions: Discussion of the role of lifestyle factors, such as exercise, diet, sleep, and stress management, in the treatment of mood disorders. The book provides practical tips and recommendations for incorporating these interventions into a treatment plan.
- Integrated Treatment Approaches: The book emphasizes the importance of combining pharmacotherapy, psychotherapy, and lifestyle interventions for optimal treatment outcomes. It provides guidance on how to develop personalized treatment plans that address the individual needs of each patient. [4]
Prevention
Prevention
- Risk and protective factors: It outlines the various factors that increase or decrease the likelihood of developing mood disorders in adolescents, such as genetic predisposition, family environment, stressful life events, and coping skills.
- Prevention strategies: It presents evidence-based interventions that have been shown to be effective in preventing or reducing the severity of mood disorders in adolescents. These interventions include:
- Universal prevention programs: Targeted at the general population of adolescents, regardless of their risk level.
- Selective prevention programs: Targeted at adolescents who are at higher risk due to specific risk factors (e.g., family history of mood disorders).
- Indicated prevention programs: Targeted at adolescents who are showing early signs of mood disturbance.
- Future directions: The chapter also discusses the need for further research to develop more effective prevention programs and to better understand the mechanisms underlying mood disorders in adolescents. [10]
Homeopathic Treatment
Homeopathic Treatment for various Mood Disorders:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
1. Arsenicum album :
Anxious, insecure, and perfectionist people who need this remedy may set high standards for themselves and others and become depressed if their expectations are not met. Worry about material security sometimes borders on despair. When feeling ill, these people can be demanding and dependent, even suspicious of others, fearing their condition could be serious.
2. Aurum metallicum:
Generally, This remedy can be helpful to serious people, strongly focused on work and achievement, which become depressed if they feel they have failed in some way. Additionally, Discouragement, self-reproach, humiliation, and anger can lead to "feelings of emptiness and worthlessness. All in all, The person may feel worse at night, with nightmares or insomnia.
3. Calcarea carbonica:
A dependable, industrious person who becomes overwhelmed from too much worry, work, or physical illness may benefit from this remedy. Moreover, Anxiety, fatigue, confusion, discouragement, self-pity, and a dread of disaster may develop. Lastly, A person who needs this remedy often feels chilly and sluggish and easily tires on exertion.
4. Causticum:
A person who feels depressed because of grief also loss ( either recent or over time) may benefit from this remedy. Furthermore, Frequent crying or a feeling of mental dullness and forgetfulness (with anxious checking to see if the door is locked, if the stove is off, etc.) are other indications. In detail, People who need this remedy are often deeply sympathetic toward others and, having a strong sense of justice, can be deeply discouraged or angry about the world.
5. Cimicifuga:
A person who needs this remedy can be energetic and talkative when feeling well, but upset and gloomy when depressed-with exaggerated fears (of insanity, of being attacked, of disaster). Painful menstrual periods and headaches that involve the neck are often seen when this remedy is needed.
6. Ignatia amara:
Sensitive people who suffer grief or disappointment and try to keep the hurt inside may benefit from this remedy. Wanting not to cry or appear too vulnerable to others, they may seem guarded, defensive, and moody. They may also burst out laughing, or into tears, for no apparent reason. A feeling of a lump in the throat and heaviness in the chest with frequent sighing or yawning are strong indications for Ignatia. Insomnia ( or excessive sleeping), headaches, and cramping pains in the abdomen and back are also often seen.
7. Kali phosphoricum:
If a person feels depressed after working too hard, being physically ill, or going through prolonged emotional stress or excitement, this remedy can be helpful. Exhausted, nervous, and jumpy, they may have difficulty in working or concentrating-and become discouraged and lose confidence. Headaches from mental effort, easy perspiration, and sensitivity to cold, anaemia, in- somnia, and indigestion often seen when this remedy is needed.
8. Natrum carbonicum:
Individuals who need this remedy are usually mild, gentle, and selfless- making an effort to be cheerful and helpful, and avoiding conflict whenever possible. After being hurt or disappointed, they can become depressed, but keep their feelings to themselves. Even when feeling lonely, they withdraw to rest or listen to sad music, which can isolate them even more, Nervous and physically sensitive (to sun, to weather changes, and to many food, especially milk), they may also get depress when feeling weak or ill.
9. Natrum muriaticum:
People who need this remedy seem reserved, responsible, and private yet have strong inner feelings (grief, romantic attachment, anger, or fear of misfortune) that they rarely show. Even though they want other people to feel for them, they can act affronted or angry if someone tries to console them, and need to be alone to cry. Anxiety, brooding about past grievances, migraines, back pain, and insomnia can also be experienced when the person is depressed. A craving for salt and tiredness from sun exposure are other indications for this remedy.
10. Pulsatilla:
People who need this remedy have a childlike softness and sensitivity-e-and can also be whiny, jealous, and moody. When depressed, they are sad and tearful, wanting a lot of attention and comforting. Crying, fresh air, also gentle exercise usually improve their mood. Besides this, Getting too warm or being in a . stuffy room can increase anxiety. Depression around the time of hormonal changes (puberty, either menstrual periods, or menopause) can often be helped with Pulsatilla.
11. Sepia:
People who feel weary, irritable, also indifferent to family members, and worn out by the demands of everyday life may respond to this remedy. Basically, They want to be left alone and may respond in an angry or cutting way if -anyone bothers them. They often feel better especially from crying, but would rather have others keep their distance and not try to console them or cheer them up. All in all, Menstrual problems, a sagging feeling in internal organs, sluggish digestion, and improvement from vigorous exercise are other indications for this remedy.
12. Staphysagria:
In general; Quiet, sensitive, emotional people who have difficulty standing up for themselves may benefit from this remedy. Hurt feelings, shame, resentment, also suppressed emotions can lead them to depression. If under too much pressure, they can sometimes lose their natural inhibition and fly into rages or throw things. Besides this, A person who needs this remedy may also have insomnia feeling sleepy all day, but unable to sleep at night), toothaches, headaches, stomach aches, or bladder infections that are stress-related.
Diet & Regimen
Diet & Regimen
Diet:
- Complex carbs: Whole grains, fruits, and vegetables for sustained energy and serotonin boost.
- Lean protein: Fish, poultry, beans, tofu for brain function and neurotransmitters.
- Omega-3s: Fatty fish, flaxseed, walnuts for mood improvement and reduced inflammation.
- Vitamin D: Sunlight, fatty fish, fortified foods to combat deficiency.
- B vitamins: Leafy greens, whole grains, legumes for nerve function and energy.
- Limit: Processed foods, sugary drinks, and excessive caffeine.
Regimen:
- Exercise: Aim for at least 30 minutes of moderate-intensity exercise most days.
- Sleep: 7-9 hours of quality sleep nightly with a consistent sleep schedule.
- Stress management: Practice meditation, deep breathing, or yoga.
- Socialize: Connect with loved ones and engage in enjoyable activities.
- Sunlight: Get some sun daily for circadian rhythm and vitamin D.
Do’s and Don'ts
Do’s:
- Seek professional help: If you suspect you or someone you know is experiencing symptoms of a mood disorder, seek professional help from a mental health specialist. Early diagnosis and treatment can significantly improve outcomes.
- Educate yourself: Learn about mood disorders, their symptoms, and available treatment options. This knowledge can empower you to make informed decisions about your mental health care.
- Stick to your treatment plan: Whether it involves medication, therapy, or lifestyle changes, adherence to your treatment plan is crucial for managing your mood disorder and preventing relapse.
- Practice self-care: Prioritize sleep, exercise, healthy eating, stress management, and relaxation techniques. These practices can help regulate your mood and improve overall well-being.
- Build a support system: Surround yourself with supportive friends and family who understand your condition and can offer encouragement and assistance. Consider joining a support group to connect with others who share similar experiences.
- Be patient and kind to yourself: Recovery from a mood disorder takes time and effort. Be patient with yourself and celebrate small victories along the way.
- Set realistic goals: Break down tasks into smaller, manageable steps and avoid putting too much pressure on yourself. Celebrate your achievements and learn from any setbacks.
Don’ts:
- Self-medicate: Avoid using alcohol, drugs, or other substances to cope with your mood disorder. These substances can worsen your symptoms and interfere with your treatment.
- Isolate yourself: While it’s normal to want to withdraw at times, isolating yourself can worsen your mood and make it harder to recover. Stay connected with loved ones and engage in activities you enjoy.
- Ignore your feelings: If you’re feeling overwhelmed or struggling to cope, don’t ignore your emotions. Talk to a trusted friend, family member, or mental health professional.
- Compare yourself to others: Everyone’s experience with a mood disorder is unique. Avoid comparing yourself to others and focus on your own progress and recovery.
- Give up: Recovery from a mood disorder can be challenging, but it’s important to remember that there is hope. With appropriate treatment and support, you can manage your symptoms and live a fulfilling life.
Remember, you are not alone. Millions of people worldwide experience mood disorders. With the right help and support, you can manage your condition and thrive.
Terminology
Terminology
- Mood Disorder: A broad term encompassing various mental health conditions characterized by significant and persistent disturbances in mood. This includes depressive disorders (e.g., major depressive disorder, persistent depressive disorder) and bi-polar disorders (e.g., bi-polar I, bi-polar II).
- Major Depressive Disorder (MDD): A common mood disorder characterized by persistent feelings of sadness, loss of interest, and other symptoms that interfere with daily life.
- Bi-polar Disorder: A mood disorder characterized by alternating episodes of mania (elevated or irritable mood) and depression.
- Mania: A state of abnormally elevated or irritable mood, increased energy, and often impulsive behavior.
- Hypomania: A milder form of mania that does not significantly impair functioning.
- Depression: A state of low mood and aversion to activity that can affect a person’s thoughts, behavior, feelings, and sense of well-being.
- Anhedonia: The inability to experience pleasure from activities that were once enjoyable.
- Alogia: Poverty of speech, a symptom often seen in depression.
- Avolition: Lack of motivation or goal-directed behavior.
- Psychomotor Agitation: Excessive motor activity associated with a feeling of inner tension.
- Psychomotor Retardation: Slowing of physical and emotional reactions, including speech and affect.
- Affect: The outward expression of a person’s emotional state.
- Dysthymia: A persistent depressive disorder characterized by a chronic low mood for at least two years.
- Cyclothymia: A mood disorder characterized by chronic fluctuations between hypomanic and depressive symptoms.
- Euthymia: A normal, non-depressed, reasonably positive mood.
- Cognitive Behavioral Therapy (CBT): A type of psychotherapy that helps people identify and change negative thought patterns and behaviors that contribute to mood disorders.
- Interpersonal Psychotherapy (IPT): A type of psychotherapy that focuses on improving interpersonal relationships and social skills to help manage mood disorders.
- Antidepressants: Medications used to treat depression.
- Mood Stabilizers: Medications used to manage mood swings in bipolar disorder.
Common Homeopathic Remedies for Mood Disorders:
- Ignatia: Often used for grief, loss, or emotional trauma. Individuals may experience mood swings, hypersensitivity, and a lump in the throat sensation.
- Natrum Muriaticum: Suitable for individuals who suppress emotions, experience grief, or feel worse from consolation. They may also have strong cravings for salt.
- Sepia: Often prescribed for women experiencing hormonal changes, such as during menopause or postpartum. Symptoms may include irritability, indifference, and exhaustion.
- Pulsatilla: Indicated for individuals who are emotionally sensitive, weepy, and seek reassurance. They may experience changeable moods and crave attention.
- Aurum Metallicum: Used for deep depression, feelings of worthlessness, and suicidal thoughts. Individuals may be workaholics and experience guilt and despair.
- Arsenicum Album: Helpful for anxiety, restlessness, and fear, especially related to health or finances. Individuals may be fastidious and perfectionistic.
References
References
- Homoeopathy in treatment of psychological disorders by Shilpa Harwani.
- National Mental Health Survey of India, 2015-16. Ministry of Health and Family Welfare, Government of India.
- Gururaj, G., Varghese, M., Benegal, V., & others. (2019). Prevalence and socioeconomic impact of depressive disorders in India: multisite population-based cross-sectional study.
- The American Psychiatric Association Publishing Textbook of Mood Disorders (Second Edition) Charles B. Nemeroff, Alan F. Schatzberg, Natalie Rasgon, Stephen M. Strakowski (2022, American Psychiatric Association Publishing)
- Kaplan & Sadock’s Comprehensive Textbook of Psychiatry (Tenth Edition) Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz (2017, Wolters Kluwer)
- Neurobiology of Mental Illness (Fifth Edition) Dennis S. Charney, Eric J. Nestler (2019, Oxford University Press)
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) American Psychiatric Association, 2022 (Text Revision)
- The Psychiatric Interview (Third Edition) Shawn Christopher Shea (2018. Elsevier)
- Massachusetts General Hospital Comprehensive Clinical Psychiatry (Second Edition) Theodore A. Stern, Maurizio Fava, Jerrold F. Rosenbaum, Joseph Biederman (2016, Elsevier)
- Treating and Preventing Adolescent Mental Health Disorders: What We Know and What We Don’t Know (2nd Edition) Dwight L. Evans, C. Hendricks Brown, Melanie M. Wall, Patrick H. Tolan, Kimberly E. Hoagwood (2017, Oxford University Press)
- Integrative Therapies for Depression: Reuniting the Body and Mind. by James M. Greenblatt, M.D. (2011, Taylor & Francis)
Also Search As
Also Search As
There are several ways people can search for homeopathic articles on mood disorders:
Online Databases:
- Homeopathic Library (hpathy.com): This website contains a vast collection of homeopathic articles, cases, and materia medica. You can search for specific mood disorders or browse by remedy.
- PubMed: While not exclusively homeopathic, PubMed includes some articles and studies related to homeopathy. Use search terms like "homeopathy AND mood disorder" or "homeopathy AND depression."
Homeopathic Journals and Publications:
- The Homeopathic Links: An online journal with articles on various topics, including mood disorders.
- The American Journal of Homeopathic Medicine: A peer-reviewed journal that publishes original research and case studies related to homeopathy.
Homeopathic Organizations and Websites:
- National Center for Homeopathy (NCH): This organization offers resources and information on homeopathy, including articles and research on mood disorders.
- Council for Homeopathic Certification (CHC): This website provides information on certified homeopathic practitioners and may have links to articles on mood disorders.
Books:
- Several books on homeopathic treatment of mental and emotional disorders are available. Search for titles like "Homeopathy for Emotional and Mental Disorders" or "Homeopathic Psychology" in online bookstores or libraries.
Homeopathic Practitioners:
- Consult with a qualified homeopathic practitioner. They can provide personalized recommendations and direct you to relevant resources.
There are several ways to search for information on mood disorders, depending on your needs and the type of information you are looking for:
Online Search Engines:
- Google, Bing, DuckDuckGo: Use search terms like "mood disorders," "depression," "bipolar disorder," "types of mood disorders," "symptoms of mood disorders," or "treatment for mood disorders."
- Specific websites: Reputable health organizations and medical institutions often have dedicated sections on mood disorders. Consider searching websites like the National Institute of Mental Health (NIMH), Mayo Clinic, Cleveland Clinic, or WebMD.
Academic Databases:
- PubMed: A free resource developed by the National Center for Biotechnology Information (NCBI) that provides access to millions of biomedical literature citations and abstracts.
- Google Scholar: A search engine that indexes scholarly literature across many disciplines and sources, including articles, theses, books, abstracts, and court opinions.
- ScienceDirect: A leading full-text scientific database offering journal articles and book chapters from a wide range of scientific fields.
Books and Libraries:
- Libraries: Public and university libraries often have a collection of books on mental health and mood disorders.
- Bookstores: Many bookstores have sections dedicated to health and wellness, where you can find books on mood disorders.
- Online retailers: Websites like Amazon offer a wide range of books on mood disorders, both in physical and digital formats.
Mental Health Organizations:
- National Alliance on Mental Illness (NAMI): Provides support, education, advocacy, and public awareness programs for individuals and families affected by mental illness.
- MentalHealth.gov: A U.S. government website that provides information and resources on mental health topics.
- The Jed Foundation: A nonprofit organization dedicated to preventing suicide in young adults and promoting emotional well-being.
Social Media:
- Support groups: Many online communities and forums provide support and information for people with mood disorders and their loved ones.However, be cautious about the accuracy of information shared in these groups.
- Support groups: Many online communities and forums provide support and information for people with mood disorders and their loved ones.
What is Mood Disorders?
Definition:
Mood disorders is a category of mental health problems that include all types of depression and bipolar disorder. Additionally, It is sometimes called affective disorders.
What causes Mood Disorders?
Causes:
- Chemical imbalance in the brain
- Life events
- Multifactorial inherited
- Genetic and environmental
How are mood disorders diagnosed?
Mood disorders are typically diagnosed by a mental health professional, such as a psychiatrist or psychologist, based on a comprehensive evaluation of the person’s symptoms, medical history, and mental health assessment.
What are the types of Mood Disorders?
Types:
- Major depression
- Dysthymia (in other words; dysthymic disorder)
- excited depression (bipolar disorder)
- Mood disorder due to a general medical condition
- Substance induced mood disorder
Give the symptoms of Mood Disorders?
Symptoms:
- Persistent feelings of sadness.
- Feeling either hopeless or helpless.
- Having low self-esteem.
- Feeling inadequate.
- Excessive guilt.
- Feelings of wanting to die.
- Loss of interest in usual activities or activities once enjoyed.
- Difficulty with relationships.
- Sleep disturbances
Where can I get help for mood disorders?
If you think you may be experiencing a mood disorder, it’s important to seek professional help. You can start by talking to your doctor, who may refer you to a mental health specialist. You can also reach out to mental health organizations like the National Institute of Mental Health (NIMH) or the National Alliance on Mental Illness (NAMI) for information and resources.
Can homeopathy help with mood disorders?
Yes,
Some people find homeopathy helpful for managing mood disorder symptoms. It aims to treat the whole person, considering emotional, mental, and physical aspects.
Is homeopathy a safe treatment for mood disorders?
Homeopathic remedies are generally considered safe when prescribed by a qualified practitioner. However, it’s important to inform your doctor about any homeopathic treatment you’re using.
What homeopathic remedies are used for mood disorders?
Common remedies include:
- Ignatia for grief, Natrum Muriaticum for suppressed emotions, Sepia for hormonal mood swings, Pulsatilla for weepiness, Aurum Metallicum for deep depression, and Arsenicum Album for anxiety.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Mood Disorders?
Homoeopathic Medicines for Mood Disorders
- Arsenicum album
- Aurum metallicum
- Calcarea carbonica
- Causticum
- Cimicifuga
- Ignatia
- Kali phos
