Menopause
Definition
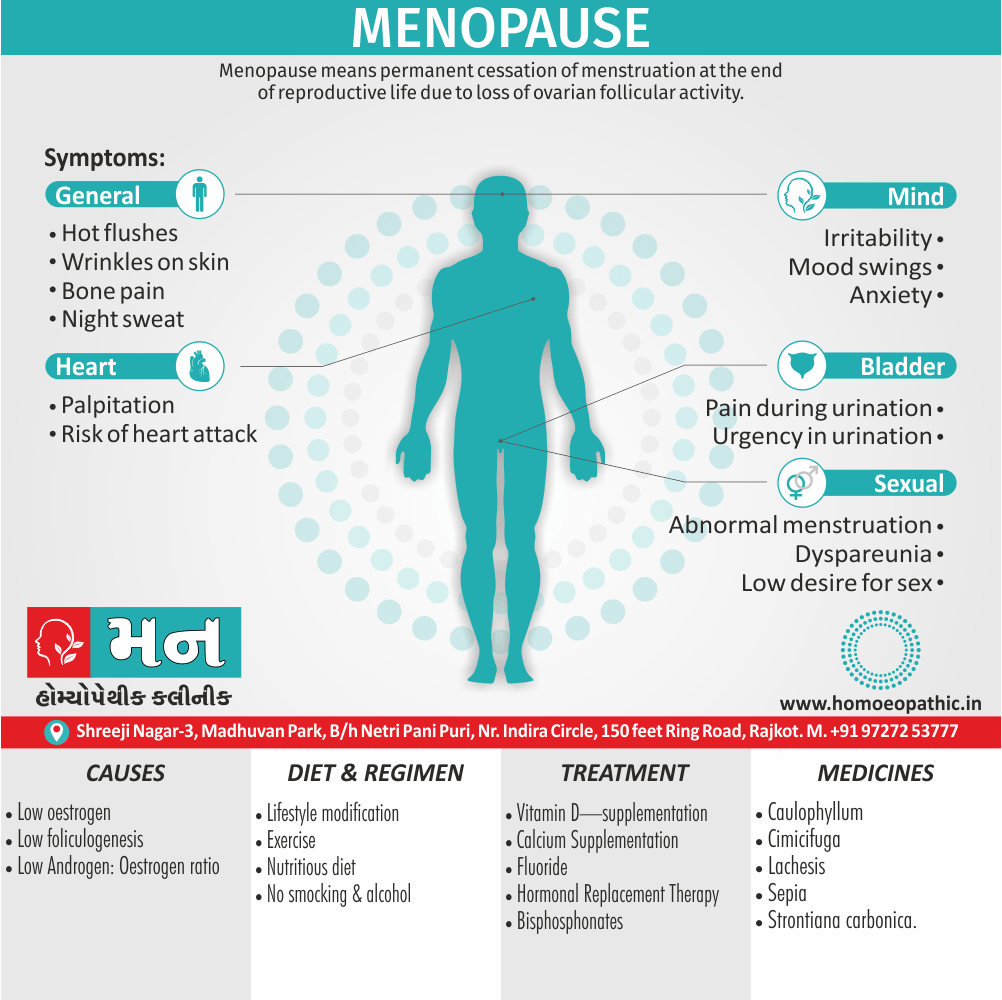
Menopause means permanent cessation of menstruation at the end of reproductive life due to loss of ovarian follicular activity. It is the point of time when Last and final menstruation occurs.[1]
There are two main synonyms for menopause, each with slightly different connotations:
- Change of life: This is a more general term that refers to the biological and social changes that women experience around menopause. It can be a more euphemistic way to talk about menopause, but it doesn’t necessarily capture the specific biological aspects.
- Climacteric: This is a medical term that refers to the transitional period in a woman’s life marked by the decline in ovarian function and the end of menstruation. It’s a more technical term than "menopause" but emphasizes the physiological changes.
Here’s a quick breakdown:
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
The clinical diagnosis is confirmed following stoppage of menstruation (amenorrhea) for twelve consecutive months without any other pathology. As such, a woman declare to have attained menopause only retrospectively. Premenopausal refers to the period prior to menopause, post menopause to the period after menopause and perimenopause to the period around menopause (40–55 years), Climacteric is the period of time during which a woman passes from the reproductive to the nonreproductive stage. This phase covers 5–10 years on either side of menopause. Perimenopause is the part of the climacteric when the menstrual cycle is likely to be irregular. Post menopause is the phase of life that comes after the menopause.[1]
Age of Menopause
Age at which menopause occurs genetically predetermine. The age of menopause is not relate to age of menarche or age at last pregnancy. It is also not relate to number of pregnancies, lactation, use of oral pill, socioeconomic condition, race, height or weight. Thinner women have early menopause. However, cigarette smoking and severe malnutrition may cause early menopause. The age of menopause ranges between 45–55 years, average being 50 years.[1]
Clinical Importance
Due to increased life expectancy, especially in affluent society, about one-third of life span will be spent during the period of estrogen deprivation stage with long-term symptomatic and metabolic complications.[1]
Endocrinology of Climacteric and Menopause
Hypothalamopituitary Gonadal Axis
Few years prior to menopause, along with depletion of the ovarian follicles, the follicles become resistant to pituitary gonadotropins. As a result, effective folliculogenesis impaire with diminished estradiol production.
This decreases the negative feedback effect on hypothalamo-pituitary axis resulting in increase in FSH. The increase in FSH also due to diminish inhibin. Inhibin, a peptide, secrete by the granulosa cells of the ovarian follicle. The increase of LH occurs subsequently. Disturbed folliculogenesis during this period may result in anovulation, oligo-ovulation, premature corpus luteum or corpus luteal insufficiency. The sustained level of estrogens may even cause endometrial hyperplasia and clinical manifestation of menstrual abnormalities prior to menopause. The mean cycle length is significantly shorter. This is due to shortening of the follicular phase of the cycle. Luteal phase length remaining constant. Ultimately, no more follicles are available and even some exist, they are resistant to gonadotropins. Estradiol production drops down to the optimal level of 20 pg/mL → no endometrial growth → absence of menstruation.
Androgens:
After menopause, the stromal cells of the ovary continue to produce androgens because of increase in LH. The main androgens are androstenedione and testosterone. Though the secretion of androgens from postmenopausal ovary are more, their peripheral levels reduce due to conversion of androgens to estrone in adipose tissue. However, the cumulative effect is a decrease in estrogenic: androgen ratio. This Results in increased facial hair growth and change in voice. As the higher weight patient converts more androgens into estrone, they are less likely to develop symptoms of oestrogen deficiency and osteoporosis. But they are Vulnerable to endometrial hyperplasia and endometrial carcinoma.[1]
Epidemiology
Epidemiology
The Indian Menopause Society (IMS) conducted a study on the age of menopause in 10 Indian cities, including over 1900 women. The mean age of menopause was found to be 46.7 years, with a range of 39-56 years.
Reference: The Indian Menopause Society (IMS). (2004). Consensus statement on menopause research. Journal of Mid-life Health, 5(2), 55-61.[3]
Causes
Causes
Natural Cause:
The primary natural cause of menopause is the depletion of ovarian follicles.
This is a gradual process that typically begins in a woman’s 40s and results in decreased production of estrogen and progesterone. As these hormone levels decline, menstruation becomes irregular and eventually ceases, marking the onset of menopause.
Artificial Causes:
Several artificial factors can induce menopause prematurely, including:
- Surgical menopause: The surgical removal of both ovaries (oophorectomy) leads to an abrupt cessation of hormone production and the immediate onset of menopause.
- Chemotherapy and radiation therapy: These cancer treatments can damage the ovaries, leading to premature menopause.
- Premature ovarian insufficiency (POI): This condition, also known as premature ovarian failure, occurs when the ovaries stop functioning normally before age 40.The cause of POI is often unknown, but it can be due to genetic factors, autoimmune disorders, or certain infections. [4]
Types
Types
Menopause can be categorized into three main types:
- Natural Menopause: This is the most common type, occurring when a woman’s ovaries naturally stop producing eggs and hormone levels decline. It typically happens between the ages of 45 and 55.
- Premature Menopause: Also known as premature ovarian insufficiency (POI), this type occurs when menopause begins before the age of 40. It can be caused by various factors, including genetics, autoimmune disorders, or medical treatments.
- Induced Menopause: This type is artificially induced by medical interventions such as surgery (removal of ovaries) or cancer treatments (chemotherapy or radiation therapy). [5]
Risk Factors
Risk factors
Several factors can influence the onset and experience of menopause:
Modifiable Risk Factors:
- Smoking: Women who smoke tend to experience menopause earlier than non-smokers.
- Body Mass Index (BMI): Both underweight and over-weight women may experience menopause earlier.
- Lack of Exercise: Physical inactivity can increase the risk of early menopause.
- Diet: A diet low in vitamin D and calcium can impact bone health during menopause.
Non-Modifiable Risk Factors:
- Age: The most significant risk factor is age. Most women experience natural menopause between 45 and 55 years old.
- Genetics: Family history of early menopause can increase the risk.
- Ethnicity: Women of certain ethnicities, such as Hispanic and African American women, may experience menopause earlier.
- Medical History: Certain medical conditions or treatments, such as autoimmune disorders or chemotherapy, can trigger early menopause. [6]
Pathogenesis
Pathogenesis of Menopause
The pathogenesis of menopause involves a complex interplay of biological processes leading to the cessation of ovarian function.
Primarily, it’s driven by the depletion of ovarian follicles, which house and nurture immature eggs. As a woman ages, the number of follicles declines, resulting in diminished production of estrogen and progesterone, the primary female sex hormones. This hormonal decline triggers a cascade of physiological changes, including irregular menstrual cycles and eventually, the cessation of menstruation, marking the onset of menopause.
Several factors contribute to this follicular depletion:
- Follicular Atresia: This is a natural process where follicles degenerate and are reabsorbed by the body. It occurs throughout a woman’s life but accelerates as she approaches menopause.
- Reduced Follicle Recruitment: The ovaries become less responsive to hormonal signals that stimulate follicle growth, leading to fewer follicles maturing each cycle.
- Decreased Ovarian Responsiveness: The remaining follicles become less sensitive to follicle-stimulating hormone (FSH) and luteinizing hormone (LH), further hindering their maturation and ovulation.
The resulting hormonal changes not only impact the reproductive system but also affect various other bodily functions. These include vasomotor symptoms (hot flashes and night sweats), sleep disturbances, mood changes, bone loss, and cardiovascular risks. [7]
Pathophysiology
Pathophysiology of Menopause
The pathophysiology of menopause is a complex interplay of hormonal, ovarian, and systemic changes.
The primary event is the depletion of ovarian follicles, leading to a decline in estrogen and progesterone production. This decline disrupts the hypothalamic-pituitary-ovarian (HPO) axis, the feedback loop that regulates reproductive function.
As estrogen levels decrease, the hypothalamus increases its production of gonadotropin-releasing hormone (GnRH), stimulating the pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). However, the ovaries become less responsive to these hormones, resulting in irregular ovulation and eventually, the cessation of menstruation.
This hormonal imbalance also affects other systems in the body, leading to various menopausal symptoms. For example, declining estrogen levels can cause:
Vasomotor symptoms
Hot flashes, night sweats, and flushing due to dysregulation of the thermoregulatory system.
Urogenital atrophy:
Vaginal dryness, itching, and pain during intercourse due to thinning and decreased lubrication of vaginal tissues.
Bone loss
Increased risk of osteoporosis due to decreased bone density.
Cardiovascular changes
Increased risk of heart disease due to changes in lipid metabolism and vascular function.
Mood changes
Irritability, depression, and anxiety due to the impact of hormones on neurotransmitters. [8]
Clinical Features
Clinical Features of Menopause
The clinical features of menopause can be broadly categorized into:
1. Vasomotor Symptoms:
- Hot flashes: Sudden feeling of intense warmth, often accompanied by sweating, flushing, and palpitations.
- Night sweats: Excessive sweating during sleep, often disrupting sleep patterns.
- Other vasomotor symptoms: Dizziness, headaches, and chills.
2. Urogenital Symptoms:
- Vaginal dryness: Thinning and drying of the vaginal tissues, leading to discomfort and pain during intercourse.
- Vaginal atrophy: Shrinkage and inflammation of the vagina.
- Urinary symptoms: Increased frequency, urgency, and incontinence.
- Increased susceptibility to urinary tract infections.
3. Psychological Symptoms:
- Mood swings: Irritability, anxiety, and depression.
- Difficulty sleeping: Insomnia or disturbed sleep patterns.
- Cognitive changes: Difficulty concentrating and memory problems.
4. Other Symptoms:
- Joint pain: Stiffness and aching in joints.
- Muscle aches and pains.
- Decreased libido.
- Skin changes: Dryness, thinning, and loss of elasticity.
- Hair changes: Thinning and hair loss.
- Weight gain.
- Changes in body shape.
- Breast tenderness. [9]
Sign & Symptoms
Sign & Symptoms
Generally, In majority, apart from cessation of menstruation, no more symptoms are evident. In some women symptoms appear. The important symptoms and the health concerns of menopause are i.e.:
- Vasomotor symptoms
- Urogenital atrophy
- Osteoporosis also fracture Osteopenia (WHO) refers to bone mineral density
- Cardiovascular disease
- Cerebrovascular disease
- Psychological changes
- Skin and Hair
- Sexual dysfunction
- Dementia and cognitive decline.[1]
Vasomotor symptoms:
The characteristic symptom of menopause is “hot flush”. Hot flush characterize by sudden feeling of heat followed by profuse sweating. There may also the symptoms of palpitation, fatigue and weakness. The physiologic changes with hot flushes are perspiration and cutaneous vasodilatation. Both these two functions are under central thermoregulatory control. Low oestrogen level is a prerequisite for hot flush. Hot flush coincides with GnRH pulse secretion with increase in serum LH level. It may last for 1–10 minutes, and may at times unbearable. Sleep may be disturbed due to night sweats. The thermoregulatory centre in association with GnRH Centre in the hypothalamus involve in the ethology of hot flush.
Gonadotropins (LH) are Thought involve.[1]
Genital and urinary system:
Steroid receptors have identify in the mucous membrane of urethra, bladder, vagina also the pelvic floor muscles. oestrogen plays an important role to maintain the epithelium of vagina, urinary bladder also the urethra. oestrogen deficiency produces atrophic epithelial changes in these organs. All in all, This may cause dyspareunia and dysuria.
Vagina:
Minimal trauma may cause vaginal bleeding. Dyspareunia, vaginal infections, dryness, pruritus and leukorrhea are also common. The urinary symptoms are: urgency, dysuria and recurrent urinary tract infection and stress incontinence.[1]
Sexual dysfunction:
Oestrogen deficiency often associate with decreased sexual desire. This may due psychological changes (depression anxiety) as well as atrophic changes of the genitourinary system.
Skin and hair:
There are thinning, loss of elasticity and wrinkling of the skin. Skin collagen content and thickness decrease by 1–2% per year. “Purse string” wrinkling around the month and “crow feet” around the eyes are the characteristics. oestrogen receptors are present in the skin and maximum are present in the facial skin. oestrogen replacement can prevent this skin loss during menopause. After menopause, there is some loss of pubic and axillary hair and slight balding. This may due to low level of oestrogen with normal level of testosterone.
Psychological changes:
There increase frequency of anxiety, headache, insomnia, irritability dysphasia and depression. They also suffer from dementia, mood swing and inability to concentrate. oestrogen increases opioid (neurotransmitter) activity in the brain and is known to important for memory.
Dementia:
oestrogen thought to protect the function of central nervous system. Dementia and mainly Alzheimer disease are more common in postmenopausal women.[1]
Osteoporosis and fracture:
Following menopause there are decline in collagenous bone matrix resulting in osteoporotic changes. Bone Mass loss and microarchitectural deterioration of bone tissue occurs primarily in trabecular bone (vertebra, distal radius) and in cortical bones. Bone loss increases to 5% per year during menopause. Osteoporosis may primary (Type 1) due to oestrogen loss, age, deficient nutrition (calcium, vit. D) or hereditary. It may secondary (Type 2) to endocrine abnormalities (parathyroid, diabetes) or medication.
Osteoporosis may lead to back pain, loss of height and kyphosis. Fracture of bones is a major health problem. Fracture may involve the vertebral body, femoral neck, or distal forearm (Colles’ fracture). Morbidity and mortality in older women following fracture is high.[1]
Detection of osteoporosis:
Computed tomography (CT) and specially the dual-energy X-ray absorptiometry (DEXA) are reliable methods to assess the bone-mineral density. Total radiation exposure is high with CT than DEXA.
Biochemical parameters to detect bone loss are measurement of urinary calcium/creatinine and hydroxyproline/creatinine ratios.
Cardiovascular and cerebrovascular effects:
Oxidation of LDL and foam cell formation cause vascular endothelial injury, cell death and smooth muscle proliferation. All these lead to vascular atherosclerotic changes, vasoconstriction and thrombus formation.
Risks of ischemic heart disease, coronary artery disease and strokes are increased.[1]
Clinical Examination
Clinical Examination of Menopause
The clinical examination of a woman experiencing menopause involves a comprehensive assessment of her overall health and specific menopausal symptoms. This typically includes:
History Taking:
- Detailed menstrual history: Age at menarche, regularity of cycles, duration of bleeding, and date of last menstrual period.
- Menopausal symptoms: Severity and frequency of hot flashes, night sweats, vaginal dryness, mood changes, sleep disturbances, and other relevant symptoms.
- Medical history: Past and current medical conditions, medications, surgeries, and family history.
- Lifestyle factors: Smoking, alcohol consumption, exercise, and diet.
Physical Examination:
- General appearance: Assess for any signs of distress, fatigue, or weight changes.
- Vital signs: Measure blood pressure, heart rate, respiratory rate, and temperature.
- Breast examination: Palpate for any lumps, masses, or tenderness.
- Pelvic examination: Assess the external genitalia, vagina, and cervix for signs of atrophy, dryness, or inflammation.
- Abdominal examination: Palpate for any masses or tenderness.
Additional Tests:
- Hormone levels: Measurement of follicle-stimulating hormone (FSH) and estradiol levels can help confirm menopause.
- Bone density scan: To assess for osteoporosis, a common complication of menopause.
- Thyroid function tests: To rule out thyroid disorders, which can have similar symptoms to menopause.
- Lipid profile: To assess cardiovascular risk, as menopause can affect cholesterol levels. [8]
Diagnosis
Diagnosis
- Cessation of menstruation for consecutive 12 months during climacteric.
- Appearance of menopausal symptoms ‘hot flush’ and ‘night sweats.
- Vaginal cytology – showing maturation index of at least 10/85/5 (Features of low estrogen).
- Serum estradiol : < 20 pg/mL.
- Serum FSH and LH: >40 mlU/mL (three values at weeks interval required).
Differential Diagnosis
Differential Diagnosis of Menopause
These include:
Thyroid Disorders: Both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid) can cause irregular periods, mood swings, fatigue, and sleep disturbances, mimicking menopausal symptoms.
Anxiety Disorders: Anxiety can manifest with symptoms like hot flashes, palpitations, and sleep disturbances, which can be mistaken for menopause.
Depression: Mood changes, fatigue, and sleep problems associated with depression can overlap with menopausal symptoms.
Sleep Disorders: Insomnia or other sleep disorders can cause fatigue, irritability, and difficulty concentrating, similar to menopausal symptoms.
Medication Side Effects: Certain medications, such as antidepressants, antipsychotics, and corticosteroids, can induce menopausal-like symptoms.
Chronic Fatigue Syndrome (CFS): CFS can cause fatigue, muscle aches, sleep problems, and cognitive difficulties, potentially mimicking menopause.
Premenstrual Dysphoric Disorder (PMDD): PMDD can cause mood swings, irritability, and physical symptoms before menstruation, which may be confused with perimenopause.
Other Hormonal Imbalances: Conditions like polycystic ovary syndrome (PCOS) or adrenal disorders can cause hormonal fluctuations that mimic menopausal symptoms. [9]
Complications
Complications of Menopause
Menopause, while a natural transition, can lead to several potential complications due to the decline in estrogen levels:
Osteoporosis: The decreased estrogen levels accelerate bone loss, increasing the risk of osteoporosis, a condition characterized by weak and brittle bones prone to fractures.
- Cardiovascular Disease: Estrogen plays a protective role in cardiovascular health. Its decline during menopause increases the risk of heart disease, stroke, and other vascular conditions.
- Urogenital Atrophy: The thinning and drying of vaginal and urinary tract tissues can lead to discomfort, pain during intercourse, and increased susceptibility to urinary tract infections.
- Sexual Dysfunction: Vaginal dryness, decreased libido, and difficulty achieving orgasm are common sexual complications of menopause.
- Mood Disorders: Hormonal fluctuations can contribute to mood swings, irritability, anxiety, and depression.
Cognitive Decline: Some women may experience memory problems and difficulty concentrating during menopause, although the link between menopause and cognitive decline is still being researched.
Weight Gain: Changes in metabolism and body composition can lead to weight gain and redistribution of fat, particularly around the abdomen. [8]
Investigations
Investigations
The investigations for menopause primarily involve assessing the hormonal status and ruling out other potential causes for the symptoms.
Hormonal Assays:
- Follicle-Stimulating Hormone (FSH): Elevated FSH levels (typically >30 IU/L) are a hallmark of menopause.
- Luteinizing Hormone (LH): LH levels may also be elevated, but the increase is less pronounced than FSH.
- Estradiol: Estradiol levels decrease significantly during menopause.
- Anti-Müllerian Hormone (AMH): AMH is produced by ovarian follicles and declines with age. Low levels can indicate reduced ovarian reserve.
Other Investigations:
- Thyroid Function Tests: To rule out thyroid disorders, which can mimic menopausal symptoms.
- Complete Blood Count (CBC): To assess for anemia or other underlying conditions.
- Lipid Profile: To evaluate cardiovascular risk factors associated with menopause.
- Bone Density Scan: To assess for osteoporosis, a common complication of menopause.
Additional Tests (if indicated):
- Pelvic Ultrasound: To assess the ovaries and uterus for any abnormalities.
- Endometrial Biopsy: To evaluate the uterine lining if there is abnormal bleeding. [10]
Treatment
Treatment
Lifestyle modification i.e.:
Physical activity (weight bearing), reducing high coffee intake, smoking and excessive alcohol. There should be adequate calcium intake (300 mL of milk), reducing medications that causes bone loss (corticosteroids)
Nutritious diet i.e.
balanced with calcium and protein is helpful [1]
Supplementary calcium i.e.
daily intake of 1–1.5 g can reduce osteoporosis and fracture
Exercise i.e.
weight bearing exercises, walking, Jogging
Vitamin D—supplementation of vitamin D3 i.e.
(1500–2000 IU/day) along with calcium can reduce osteoporosis and fractures. Exposure to sunlight enhances synthesis of cholecalciferol (vitamin D3) in the skin,
Cessation of smoking and alcohol [1]
Bisphosphonates i.e.
Bisphosphonates prevent osteoclastic bone resorption. It improves bone density and prevents fracture. It is preferred for older women. Women should be monitored with bone density measurement. Drug should be stopped when there is severe pain at any site. Commonly used drugs are etidronate and alendronate. Alendronate is more potent. Ibandronate and zoledronic acid are also effective and have less side effects. Bisphosphonates when used alone cannot prevent hot flushes, atrophic changes and cardiovascular disease. It is taken in empty stomach. Nothing should be taken by mouth for at least 30 minutes after oral dosing. Patient should remain upright for 30 minutes. Side effects include gastric and oesophageal ulceration, osteomyelitis and osteonecrosis of the jaw.
Fluoride i.e.
It prevents osteoporosis and increases bone matrix. It give at a dose of 1 mg/kg for short-term only. Calcium supplementation should continue. Long-term therapy induces side effects (brittle bones).
Calcitonin inhibits bone resorption i.e.
Simultaneous therapy with calcium and vitamin D should be given. It give either by nasal spray (200 IU daily) or by injection (SC) (50–100 IU daily). It use when oestrogen therapy contraindicate.[1]
Selective oestrogen receptor modulators i.e.
(SERMs) are tissue specific in action. Of the many SERMs, raloxifene has shown to increase bone mineral density, reduce serum LDL and to raise HDL2 level. Raloxifene inhibits the oestrogen receptors at the breast and endometrial tissues. Risks of breast cancer and endometrial cancer are therefore reduced. Raloxifene does not improve hot flushes or urogenital atrophy. Evaluation of bone density (hip) should do periodically. Risks of venous thromboembolism increase.
Clonidine, an alpha-adrenergic agonist may use to reduce the severity and duration of hot flushes. It is helpful where oestrogen contraindicate (hypertension)
Thiazides i.e.
It reduce urinary calcium excretion. It increases bone density specially when combined with oestrogen.
Paroxetine i.e.
It is a selective serotonin reuptake inhibitor, is effective to reduce hot flushes (both the frequency and severity).
Gabapentin i.e.
It is an analogy of gamma-aminobutyric acid. It is effective to control hot flushes.
Phytoestrogens i.e.
It containing isoflavones are found to lower the incidence of vasomotor symptoms, osteoporosis and cardiovascular disease. It reduces the risk of breast and endometrial cancer.
Soy protein i.e.
It is also found effective to reduce vasomotor symptoms. Soy protein acts as SERMS.[1]
Prevention
Prevention
Spontaneous menopause is unavoidable. However, artificial menopause induced by surgery (bilateral oophorectomy) or by radiation (gonadal) during reproductive period can to some extent be preventable or delayed.
Counselling: Every woman with postmenopausal symptoms should be adequately explained about the physiologic events. This will remove her fears, and minimize or dispel the symptoms of anxiety, depression and insomnia. Reassurance is essential.[1]
Homeopathic Treatment
Homeopathic Treatment
The treatment in homeopathy is based on individualization in which a doctor selects a medicine according to your/ patients constitution rather than matching only symptoms similarity, so before taking any homoeopathic medicine you have to firstly consult a homoeopathic physician for your concern problem’s, there are so many remedies are useful for this condition but some few therapeutic indications of homeopathic remedies in the cases of Menopause are as below
Menopause Homeopathic Medicines
Lachesis
Suits especially women who never get well from the change of life; "have never felt well since that time." It corresponds to many climacteric troubles, such as hemorrhoids, hemorrhages, vertigo, burning on the vertex and headaches. It is remedy for women worn out by frequent pregnancies, with sudden cessation of the menses, trembling pulse, headache, flushing of the heat and rush of blood to the head, cold feet and constriction about the heart
Amyl nitrite.
Flushes of heat at change of life. The 30th potency acts well here.
Strontiana carbonica.
Flushes of heat with head symptoms relieved by wrapping head up warmly.
Sanguinaria.
Flushes at climax’s; headache with profuse menses.
Caladium.
Pruritus at menopause.
Aconite.
Derangements of circulation at menopause. Hughes also praises Glonoine for these conditions. Veratrum viride. Perhaps no remedy controls the flushes of heat, so annoying to women at the change of life, as well as Veratrum viride.[2]
Cimicifuga [Cimic]
is very often the remedy for the suffering incident to the change of life. There is sinking at the stomach, pain at the vertex and irritability of disposition. The patient is restless and unhappy, feels sad and grieved. Bayes prefers the 6th and 12th potencies to the lower dilutions. It is but just to state that many have been disappointed in the use of this remedy. Caulophyllum 3X. Dr. Ludlam praises this remedy for nervous conditions following the climax’s, when there is "great nervous tension and unrest with a propensity to work and worry over little things." Sepia. Congestion at the climax’s, in characteristic Sepia constitutions, are quickly benefited by the remedy. [2]
Bellis perennis [Bell]
Our English confreres use this remedy quite extensively in what is termed a "fagged womb." The patients are very tired, want to lie down, have a backache. There is no real disease, but a marked tiredness all the time. Carduus is of supreme importance for liver troubles at the climax’s Ustilago. Often rivals Lachesis in controlling the flooding during the climaxes. Vertigo is characteristic.[2]
Diet & Regimen
Diet & Regimen
General Dietary and Lifestyle Recommendations for Menopause:
- Eat a balanced diet: Focus on whole foods, including fruits, vegetables, whole grains, lean protein, and healthy fats.
- Get enough calcium and vitamin D: These nutrients are essential for bone health, which is particularly important during menopause.
- Limit processed foods, sugar, and unhealthy fats: These can contribute to weight gain, inflammation, and other health problems.
- Exercise regularly: Aim for at least 150 minutes of moderate-intensity exercise or 75 minutes of vigorous-intensity exercise per week.
- Manage stress: Stress can worsen menopause symptoms, so find healthy ways to cope, such as yoga, meditation, or spending time in nature.
- Get enough sleep: Aim for 7-8 hours of sleep per night to support overall health and well-being. [11,12,13]
Do’s and Don'ts
Do’s & Don’ts
menopause do’s and don’ts
Do’s:
Maintain a Balanced Diet:
- Prioritize fruits, vegetables, and whole grains for essential nutrients and fiber.
- Choose lean protein sources like fish, poultry, beans, and lentils.
- Incorporate healthy fats from avocados, nuts, seeds, and olive oil.
- Limit processed foods, sugary drinks, and unhealthy fats.
Stay Active:
- Engage in regular physical activity to help manage weight, improve mood, and boost energy levels.
- Aim for at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity exercise per week.
- Include strength training exercises to maintain muscle mass and bone density.
Prioritize Sleep:
- Aim for 7-8 hours of quality sleep each night.
- Establish a consistent sleep routine and create a relaxing bedtime environment
Manage Stress:
- Practice relaxation techniques like yoga, meditation, deep breathing, or mindfulness.
- Engage in hobbies and activities you enjoy.
- Seek support from friends, family, or a therapist if needed.
Stay Hydrated:
- Drink plenty of water throughout the day to stay hydrated and support overall health.
- You can also consume herbal teas and other non-caffeinated beverages.
Regular Check-ups:
- Schedule regular checkups with your doctor to monitor your health and discuss any concerns you may have.
DON’Ts:
Smoke:
- Smoking increases the risk of heart disease, osteoporosis, and other health problems.
- It can also worsen menopause symptoms like hot flashes and night sweats.
Excessive Alcohol Consumption:
- Limit alcohol intake as it can disrupt sleep, contribute to weight gain, and increase the risk of certain health conditions.
Neglect Calcium and Vitamin D:
- Adequate calcium and vitamin D intake is essential for bone health, especially during menopause.
- Talk to your doctor about supplements if needed.
Ignore Hot Flash Triggers:
- Identify and avoid triggers like spicy foods, caffeine, alcohol, and hot beverages that can worsen hot flashes.
Skip Regular Exercise:
- Staying active is crucial for managing menopause symptoms and maintaining overall health.
- Find activities you enjoy and make them a regular part of your routine.
Self-Medicate:
- Consult your doctor before taking any medications or supplements for menopause symptoms.
- They can assess your individual needs and recommend the best course of action.
Terminology
Terminology
Stages of Menopause:
- Perimenopause: The transitional period leading up to menopause, marked by hormonal fluctuations and irregular periods. It can last for several years.
- Menopause: The permanent cessation of menstruation, confirmed after 12 consecutive months without a period.
- Postmenopause: The time after menopause when hormone levels stabilize and symptoms may lessen.
Symptoms of Menopause:
- Hot Flashes: Sudden feelings of intense heat, often accompanied by sweating and flushing of the skin.
- Night Sweats: Hot flashes that occur during sleep, often causing disruptions.
- Vaginal Dryness: Thinning and drying of the vaginal tissues due to decreased estrogen levels.
- Mood Swings: Emotional fluctuations, including irritability, anxiety, and depression.
- Sleep Disturbances: Difficulty falling asleep or staying asleep, often due to night sweats or hormonal changes.
Other Relevant Terms:
- Hormone Replacement Therapy (HRT): Treatment using estrogen and/or progesterone to relieve menopause symptoms and reduce the risk of certain health problems.
- Osteoporosis: A condition characterized by decreased bone density and increased risk of fractures, often associated with menopause.
- Vasomotor Symptoms: Hot flashes and night sweats, caused by changes in blood vessels due to hormonal fluctuations.
- Genitourinary Syndrome of Menopause (GSM): A collection of symptoms related to decreased estrogen levels, including vaginal dryness, urinary urgency, and painful intercourse.
- Surgical Menopause: Menopause that occurs after surgical removal of the ovaries.
Common Homeopathic Remedies for Menopause:
- Sepia: Often recommended for hot flashes, irritability, fatigue, and mood swings. It may also help with vaginal dryness and decreased libido.
- Lachesis: Suitable for hot flashes that worsen with heat or tight clothing, along with mood swings, palpitations, and other hormonal symptoms.
- Pulsatilla: Beneficial for women experiencing mood swings, tearfulness, and changeable symptoms. It may also help with menstrual irregularities.
- Sulphur: Often prescribed for intense hot flashes, night sweats, and skin issues during menopause. Symptoms worsen with warmth and improve with fresh air.
- Ignatia: Helpful for emotional ups and downs, anxiety, and depression triggered by grief or stress. It may also alleviate headaches and muscle spasms.
Other Remedies:
Several other homeopathic remedies may be considered depending on individual symptoms and overall constitution. These include:
- Belladonna: For sudden, intense hot flashes with a red face and throbbing headaches.
- Calcarea carbonica: For women who feel overwhelmed and chilly, with weight gain and fatigue.
- Folliculinum: Made from estrogen, it may help with hot flashes, vaginal dryness, and mood swings.
- Sanguinaria: For hot flashes that start in the face and spread downwards, often accompanied by burning sensations.
References
References
- DC Dutta text book of gynaecology
- Therapeutics from Zomeo Ultimate LAN
- The Indian Menopause Society (IMS). (2004). Consensus statement on menopause research. Journal of Mid-life Health, 5(2), 55-61.
- Speroff’s Clinical Gynecologic Endocrinology and Infertility (9th Edition). Hugh S. Taylor, Lubna Pal, Emre Seli (2019) Wolters Kluwer.
- Discover Your Menopause Type by Joseph Collins (2003)
- Menopause Practice: A Clinician’s Guide (5th Edition) by Wulf H. Utian, MD, PhD, and Rebecca H. Thurston, PhD (2010)
- Yen & Jaffe’s Reproductive Endocrinology (8th Edition) by Jerome F. Strauss III, Robert L. Barbieri (2019, Elsevier)
- Menopause (4th Edition) by Rogerio A. Lobo (2017, Elsevier)
- Menopause Practice: A Clinician’s Guide (5th Edition) by Wulf H. Utian, MD, PhD, and Rebecca H. Thurston, PhD (2010, Cambridge University Press)
- Management of the Menopause (3rd Edition) by John Studd, Nick Panay, Wulf H. Utian (2009)
- The Menopause Manifesto: Own Your Health with Facts and Feminism by Dr. Jen Gunter (2021)
- The North American Menopause Society (NAMS) Guide to Menopause by The North American Menopause Society (Second Edition,2016)
- Menopause Confidential: A Doctor Reveals the Secrets to Thriving Through Midlife by Dr. Tara Allmen (2016)
Also Search As
Also Search As
There are several ways to search for homeopathic articles on menopause:
Online Search Engines:
- Use specific keywords: Combine terms like "homeopathy," "menopause," "remedies," and specific symptoms you’re interested in (e.g., "hot flashes," "mood swings").
- Try different search engines: Google, DuckDuckGo, Bing, and others may yield different results.
- Check the sources: Look for reputable websites, blogs, and journals specializing in homeopathy or women’s health.
Homeopathic Organizations and Websites:
- The North American Society of Homeopaths (NASH): Offers a directory of homeopathic practitioners and resources.
- The National Center for Homeopathy (NCH): Provides information on homeopathy, research, and educational materials.
- Council for Homeopathic Certification (CHC): Certifies professional homeopaths and offers resources for the public
- Local homeopathic clinics and practitioners: Many have websites with information on menopause and homeopathic approaches.
Online Homeopathic Libraries and Databases:
- HomBRex: A free online database with information on homeopathic remedies and clinical cases.
- Synergy Homeopathic: Offers a comprehensive online library with articles, cases, and materia medica.
- Complete Dynamics: Provides a vast collection of homeopathic books, journals, and software.
Academic Journals and Publications:
- The Journal of the American Institute of Homeopathy
- Homeopathy
- The International Journal of High Dilution Research
- Explore university libraries or databases like PubMed for homeopathic research articles.
Social Media and Forums:
- Homeopathic groups and forums on Facebook, Reddit, or other platforms can be a source of information and discussion. However, be critical of the information you find and verify it with reliable sources.
There are numerous ways to search for information about menopause, each offering different types of resources and perspectives:
Online Search Engines:
- General search engines (Google, Bing, DuckDuckGo): Use keywords like "menopause," "menopause symptoms," "menopause treatment," etc.
- Specialized search engines (health websites, medical journals): These can provide more targeted and in-depth information.
Medical Websites and Organizations:
- Reputable health organizations (Mayo Clinic, Cleveland Clinic, National Institutes of Health): Offer reliable, evidence-based information.
- Menopause-specific websites (The North American Menopause Society): Provide comprehensive information and resources.
Books and Publications:
- Medical textbooks: Offer in-depth, scientific explanations.
- Self-help books: Provide practical advice and personal stories.
- Magazines and articles: Often feature personal experiences and the latest research.
Healthcare Professionals:
- Your doctor or gynecologist: Can offer personalized advice and treatment options.
- Menopause specialists: Have expertise in managing menopause symptoms and complications.
Support Groups and Online Forums:
- Connect with other women going through menopause to share experiences and advice.
- Many organizations and websites offer online forums and support groups.
Social Media:
- Follow reputable healthcare organizations and experts for reliable information.
- Join online communities and discussions to connect with others experiencing menopause.
Frequently Asked Questions (FAQ)
What is Menopause?
Menopause means permanent cessation of menstruation at the end of reproductive life due to loss of ovarian follicular activity. It is the point of time when Last and final menstruation occurs.
What is the age of Menopause?
The age of menopause ranges between 45–55 years, average being 50 years.
How does menopause affect my health?
Menopause can increase the risk of certain health conditions like osteoporosis and heart disease.
It’s important to maintain a healthy lifestyle and talk to your doctor about preventative measures.
What are the symptoms of Menopause?
- Vasomotor symptoms
- Urogenital atrophy
- Osteoporosis and fracture
- Osteopenia
- Cardiovascular disease
- Cerebrovascular disease
- Psychological changes
- Skin and Hair
- Sexual dysfunction
- Dementia and cognitive decline
Are there any treatments for menopause symptoms?
Yes, several treatments can help manage symptoms.
These include hormone therapy, non-hormonal medications, lifestyle changes, and alternative therapies.
What are some natural ways to manage menopause symptoms?
Natural approaches include dietary changes, exercise, stress management techniques, and herbal supplements. Discuss these options with your doctor to see if they’re right for you.
Can homeopathy help with menopause symptoms?
Yes, homeopathy offers a holistic approach to managing menopause symptoms like hot flashes, night sweats, mood swings, and sleep disturbances.
How does homeopathic treatment for menopause work?
Homeopathic remedies stimulate the body’s self-healing abilities to restore balance and alleviate symptoms naturally.
How long does it take to see results with homeopathic treatment for menopause?
The response time varies depending on individual factors, but many women experience relief within a few weeks or months of starting treatment.
