Gangrene
Definition
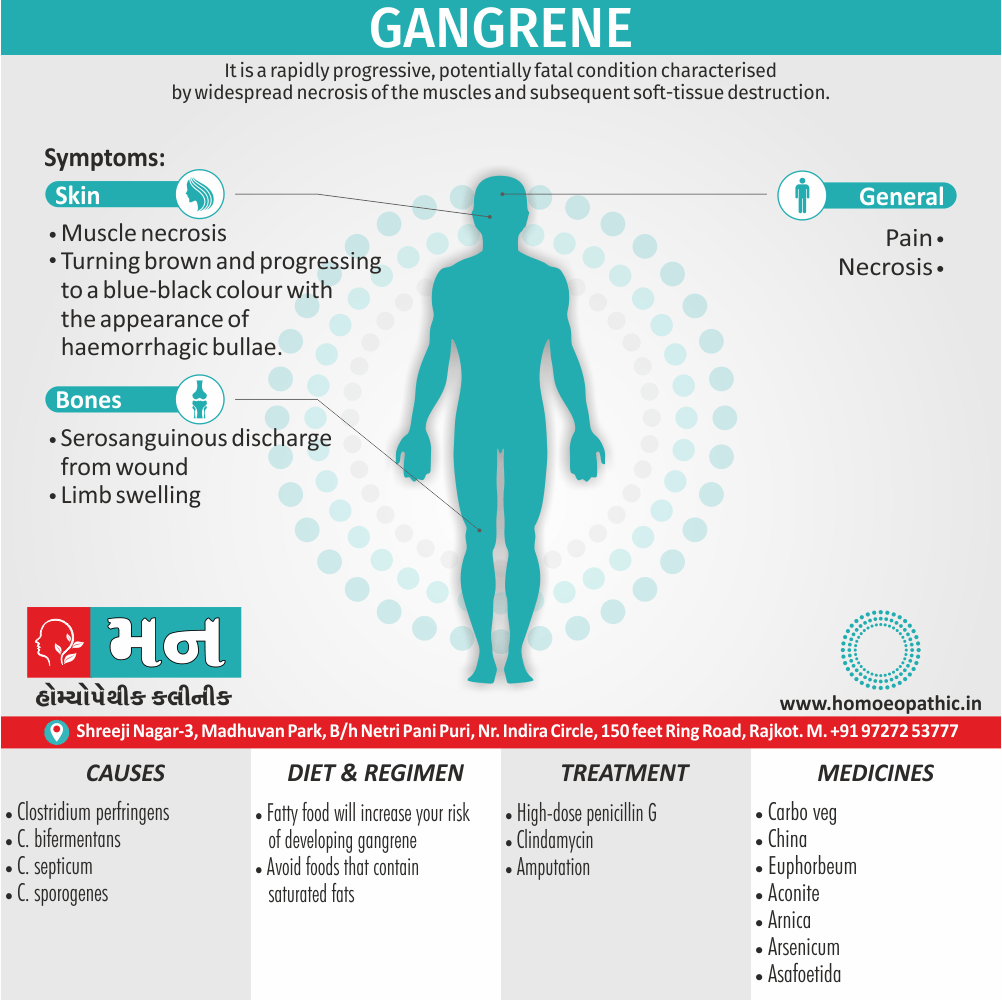
Gangrene is a rapidly progressive, potentially fatal condition characterized by widespread necrosis of the muscles and subsequent soft-tissue destruction. [1]
Here are some synonyms for gangrene:
- Necrosis: This is a general term for the death of living tissue. It is a specific type of necrosis that occurs when there is a lack of blood flow to an area of tissue.
- Mortification: This term is less commonly used than necrosis and gangrene. It refers to the death and decomposition of tissue, often accompanied by a darkening of the skin.
- Sphacelus: This term refers to a specific type of gangrene that is dry and shrunken, with a blackish-brown color.
- Putrefaction: This term refers to the decomposition of organic matter, often accompanied by a foul odor. While gangrene can involve putrefaction, not all putrefaction is gangrene.
It’s important to note that It is a serious medical condition that requires prompt treatment. If you suspect that you or someone you know may have gangrene, it is important to seek medical attention immediately.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
This is a dreaded consequence of inadequately treated missile wounds, crushing injuries and high-voltage electrical injuries.
Non-clostridia gas-producing organisms such as coliforms have also been isolated in 60–85% of cases of gas gangrene. [1]
Epidemiology
Epidemiology
There are limited studies focusing specifically on the epidemiology of gangrene in the Indian population. However, some research has touched upon the prevalence and characteristics of this condition in India:
Assessing the Prevalence Rate of Gangrene Among Patients With Peripheral Vascular Disease in a Tertiary Care Hospital in Central India (2024):
This study found a 35% prevalence of gangrene among patients with peripheral vascular disease (PVD) in a tertiary care hospital in Central India. (Bhargava et al., 2024) [4]
(PDF) Fournier’s gangrene: Prospective study of 34 patients in South Indian population and treatment strategies (2018):
While not an epidemiological study, this research provides insights into Fournier’s gangrene, a specific type of gangrene, in a South Indian population, highlighting its association with HIV and the importance of aggressive treatment. (ResearchGate, 2018) [5]
Important Considerations:
- The prevalence and incidence of gangrene can be difficult to establish due to underreporting and misdiagnosis.
- Research often focuses on specific types of gangrene or specific populations, making it difficult to generalize findings to the broader Indian population.
- More comprehensive epidemiological studies on gangrene in India are neededto fully understand its prevalence, risk factors, and outcomes.
Please note: These references provide some information, but a comprehensive epidemiological study on It in the Indian population across various regions and demographics would be needed for a complete understanding.
Causes
Causes
- The common causative organism is Clostridium perfringens, a spore-forming, Gram-positive saprophyte that flourishes in anaerobic conditions.
- Other organisms implicated in gas gangrene include bifermentans, C. septicum and C. sporogenes.
- They are present in the soil and have also been isolated from the human gastrointestinal tract and female genital tract.
- Clostridium perfringens produces many exotoxins but their exact role is unclear.
- Clostridium perfringens produces many exotoxins but their exact role is unclear.
- Alpha-toxin, the most important, is a lecithinase, which destroys red and white blood cells, platelets, fibroblasts and muscle cells.
- The phi-toxin produces myocardial suppression whereas the kappa-toxin is responsible for the destruction of connective tissue and blood vessels.
Contamination of wound
- Wounds become contaminated with clostridial spores and the devitalized tissue, foreign bodies and premature wound closure provide the anaerobic conditions necessary for spore germination.
- The usual incubation period is < 24 hours but it can range from 1 hour to 6 weeks. A vicious cycle of tissue destruction is initiated by rapidly multiplying bacteria and locally and systemically acting exotoxins.
- Locally, this results in spreading necrosis of muscle and thrombosis of blood vessels while progressive oedema further compromises the blood supply. The typical feature of this condition is the production of gas that spreads along the muscle planes.
- Systemically, the exotoxins cause severe hemolysis and, combined with the local effects, this leads to rapid progression of the disease, hypotension, shock, renal failure and acute respiratory distress syndrome (ARDS). [1]
Examples of causes include:
- Pathogens: Viruses, bacteria, fungi, parasites (infectious diseases)
- Genetic mutations: Inherited or spontaneous changes in genes (genetic diseases)
- Environmental factors: Toxins, radiation, nutritional deficiencies
- Lifestyle choices: Smoking, unhealthy diet, lack of exercise (contributing factors)
Types
Types
Gas gangrene:
- Gas gangrene typically affects deep muscle tissue. If you have gas gangrene, the surface of your skin may look normal at first.
- As the condition worsens, your skin may become pale and then turn gray or purplish red.
Dry gangrene:
- Cause: Primarily caused by ischemia (reduced blood flow) due to conditions like peripheral arterial disease (PAD) or atherosclerosis.
- Characteristics:
- Affected area becomes dry, shrunken, and dark (often black).
- Clear line of demarcation between dead and healthy tissue.
- Minimal pain and no associated infection.
Wet gangrene:
- Cause: Occurs when necrotic tissue becomes infected with bacteria, often following dry gangrene or in cases of severe injury or burns.
- Characteristics:
- Affected area is moist, swollen, and foul-smelling due to bacterial decomposition.
- No clear line of demarcation between dead and healthy tissue.
- Severe pain and systemic symptoms like fever and malaise.
Internal gangrene:
- Cause: Occurs when blood flow to an internal organ is interrupted, leading to tissue necrosis.
- Characteristics:
- Can affect organs like the intestines, appendix, or gallbladder.
- Symptoms vary depending on the affected organ but may include abdominal pain, fever, nausea, and vomiting.
Fournier’s gangrene:
- Cause: A specific type of necrotizing fasciitis (a rapidly spreading soft tissue infection) that affects the genitals and perineum.
- Characteristics:
- Rapid onset of pain, swelling, erythema, and crepitus in the genital area.
- High mortality rate if not treated aggressively. [2]
Risk Factors
Risk Factors
Following are the major risk factors:
Peripheral Arterial Disease (PAD):
- PAD is a condition characterized by narrowed arteries, reducing blood flow to the extremities. This reduced blood flow increases the risk of developing It, especially in the toes and feet.
Diabetes Mellitus:
- Elevated blood sugar levels in diabetes can damage blood vessels and nerves, impairing blood flow and sensation. This combination of factors makes individuals with diabetes more susceptible to developing gangrene.
Smoking:
- Smoking significantly increases the risk of gangrene due to its detrimental effects on blood vessels. Smoking causes vasoconstriction (narrowing of blood vessels), which reduces blood flow and can lead to tissue death.
Trauma:
- Severe injuries or trauma can damage blood vessels and disrupt blood flow to tissues, increasing the risk of gangrene.
Infection:
- Infections, particularly those that spread to deep tissues, can cause inflammation and damage to blood vessels, leading to gangrene.
Immunosuppression:
- Individuals with weakened immune systems, such as those undergoing chemotherapy or with certain medical conditions, are more susceptible to infections that can lead to It.
Intravenous Drug Use:
- Injecting illicit drugs can introduce bacteria into the bloodstream, which can then infect and damage tissues, leading to gangrene. [6]
Please note that this is not an exhaustive list of risk factors. Other factors, such as frostbite, Raynaud’s disease, and certain medical procedures, can also increase the risk of gangrene.
Pathogenesis
Pathogenesis
The pathogenesis of gangrene involves the following key steps:
Ischemia:
The primary event in Its development is ischemia, which is the insufficient blood supply to a tissue or organ. Ischemia can result from various factors, including:
- Obstruction of arterial blood flow (e.g., atherosclerosis, thrombosis, embolism)
- Reduced cardiac output (e.g., heart failure)
- Vasoconstriction (e.g., due to cold exposure, Raynaud’s disease)
- External pressure on blood vessels (e.g., tight bandages, casts)
Cell Injury and Necrosis:
- Prolonged ischemia leads to cellular injury and eventual necrosis (cell death) due to the lack of oxygen and nutrients. The extent and severity of necrosis depend on the duration and severity of ischemia, as well as the tissue’s vulnerability to hypoxia.
Development:
The necrotic tissue undergoes further changes depending on the presence or absence of infection:
- Dry: In dry gangrene, the affected area becomes dry, shrunken, and dark (often black) due to the desiccation (drying out) of the tissue. There is usually a clear line of demarcation between the dead and healthy tissue. Dry gangrene typically occurs in extremities with poor blood supply and is not usually associated with infection.
- Wet: In wet gangrene, the necrotic tissue becomes moist and swollen due to the invasion of bacteria. The area is often foul-smelling due to the decomposition of tissue by bacteria. Wet gangrene can spread rapidly and is a life-threatening condition.
- Gas: Gas gangrene is a severe form of wet gangrene caused by specific bacteria (e.g., Clostridium perfringens) that produce gas within the tissues. The affected area becomes crepitant (crackling sound on palpation) due to the presence of gas bubbles. Gas gangrene is a medical emergency and can be fatal if not treated promptly.
Additional Notes:
The pathogenesis of gangrene can vary depending on the underlying cause and the type of gangrene.
The presence of infection in wet and gas gangrene accelerates tissue damage and can lead to systemic complications, such as sepsis.
Early recognition and treatment of gangrene are crucial to prevent the spread of necrosis and associated complications. [7]
Pathophysiology
Pathophysiology
Ischemia:
The initial event in gangrene development is ischemia, which refers to inadequate blood supply to a specific tissue or organ. This can occur due to various reasons:
- Occlusion of blood vessels: Atherosclerosis, thrombosis, or embolism can block blood flow.
- Vasoconstriction: Conditions like Raynaud’s phenomenon or frostbite can cause extreme narrowing of blood vessels.
- External compression: Tight bandages, casts, or tumors can compress blood vessels and hinder blood flow.
Hypoxia and Cellular Injury:
Ischemia leads to hypoxia (lack of oxygen) and nutrient deprivation in the affected tissue. This results in cellular injury and dysfunction. If the ischemia persists, cells eventually undergo necrosis (cell death).
Development:
The type of gangrene that develops depends on the presence or absence of infection:
- Dry: In the absence of infection, the necrotic tissue becomes dry, shrunken, and dark (often black) due to the desiccation (drying out) of the tissue. There is usually a clear line of demarcation between the dead and healthy tissue.
- Wet: When the necrotic tissue becomes infected by bacteria, it results in wet gangrene. The tissue appears moist, swollen, and foul-smelling due to bacterial decomposition. Wet gangrene can spread rapidly and is often life-threatening.
- Gas: Gas gangrene is a severe form of wet gangrene caused by specific gas-producing bacteria (e.g., Clostridium perfringens). The affected tissue becomes crepitant (crackling sound on palpation) due to the presence of gas bubbles. Gas gangrene is a medical emergency.
Systemic Complications:
If left untreated, gangrene can lead to systemic complications:
- Sepsis: Bacteria from the infected tissue can enter the bloodstream, causing a life-threatening systemic inflammatory response called sepsis.
- Toxemia: Toxins produced by bacteria can also enter the bloodstream and cause systemic toxicity.[8]
It’s important to note that the pathophysiology of gangrene can vary depending on the underlying cause, the type of gangrene, and individual patient factors.
Clinical Features
Clinical Feature
Dry Gangrene:
- Appearance: Skin becomes dry, shrunken, and changes color, progressing from blue or purple to black.
- Sensation: Affected area may be numb or have decreased sensation.
- Pain: Pain is usually minimal, but there may be an aching or burning sensation.
- Spread: Progresses slowly, usually limited to the extremities.
- Line of Demarcation: A clear line separates the dead tissue from healthy tissue.
Wet Gangrene:
- Appearance: Skin becomes moist, swollen, and discolored (often black).
- Sensation: Loss of sensation in the affected area.
- Pain: Severe pain and tenderness.
- Spread: Rapid progression, with the potential to spread to other body parts.
- Discharge: Foul-smelling discharge or pus may be present.
Gas Gangrene:
- Appearance: Skin becomes discolored, with a bronze or reddish hue, and may have blisters filled with foul-smelling fluid.
- Sensation: Loss of sensation in the affected area.
- Pain: Severe pain and tenderness.
- Spread: Rapid progression, with the potential to be fatal if not treated promptly.
- Crepitus: Crackling sensation under the skin due to gas production by bacteria.
Additional Features:
- Systemic Symptoms: Fever, chills, malaise, and tachycardia may be present, particularly in wet and gas gangrene.
- Underlying Disease: Signs and symptoms of the underlying cause (e.g., diabetes, peripheral arterial disease, trauma) may also be present. [9]
Important Note: Gangrene is a medical emergency, especially wet and gas gangrene. If you suspect gangrene, seek immediate medical attention.
Sign & Symptoms
Sign And Symptoms
- The earliest symptom is acute onset of pain that increases in severity as the myo-necrosis progresses.
- The limb swells up.
- The wound exudes a serosanguinous discharge.
- The skin is involved secondary to underlying muscle necrosis, turning brown and progressing to a blue-black colour with the appearance of hemorrhagic bullae.
- The characteristic sickly-sweet odour and soft tissue crepitus caused by gas production appear with established infection but the absence of either does not exclude the diagnosis.
- These local signs are accompanied by pyrexia, tachycardia disproportionate to body temperature, tachypnoea and alteration in mental status. [1]
Clinical Examination
Clinical Examination
Inspection:
- Color: Assess the color of the affected area. Dry gangrene typically appears black, brown, or blue, while wet gangrene may be black, brown, green, or yellow. Gas gangrene may exhibit a bronze or reddish hue with blisters containing foul-smelling fluid.
- Texture: Observe the texture of the skin. Dry gangrene appears dry and leathery, while wet gangrene appears moist and swollen.
- Line of Demarcation: Look for a clear line separating the dead tissue from healthy tissue, which is usually present in dry gangrene but may be absent or less distinct in wet gangrene.
- Blisters: Note the presence of blisters, which are more common in gas gangrene.
- Discharge: Look for foul-smelling discharge or pus, which is characteristic of wet gangrene.
Palpation:
- Temperature: Assess the temperature of the affected area. Dry gangrene usually feels cold, while wet gangrene may be warm or cool.
- Crepitus: Palpate for crepitus (crackling sensation under the skin), which indicates the presence of gas in gas gangrene.
- Tenderness: Palpate for tenderness, which is typically present in wet and gas gangrene but may be absent in dry gangrene.
Auscultation:
- Blood Flow: Use a Doppler ultrasound to assess blood flow in the affected area, particularly in dry gangrene where blood flow is significantly reduced or absent.
Neurological Examination:
- Sensation: Assess sensation in the affected area using light touch, pinprick, and temperature. Loss of sensation is common in gangrene.
Systemic Examination:
- Vital Signs: Assess vital signs, including blood pressure, heart rate, respiratory rate, and temperature. Fever, tachycardia, and hypotension may indicate systemic complications, such as sepsis.
- Other Systems: Assess other organ systems for signs of underlying conditions that may have contributed to gangrene development (e.g., peripheral vascular disease, diabetes).
- Additional Considerations:
- Imaging: Radiographs, computed tomography (CT), or magnetic resonance imaging (MRI) may be used to assess the extent of tissue involvement and identify underlying causes.
- Laboratory Tests: Blood tests, wound cultures, and tissue biopsies may be performed to confirm the diagnosis, identify the causative organism (in wet and gas gangrene), and assess the patient’s overall health status.[10]
Important Note: Gangrene is a medical emergency. If you suspect gangrene, immediate medical attention is crucial. Early diagnosis and treatment can significantly improve outcomes and prevent life-threatening complications.
Diagnosis
Diagnosis
- The diagnosis make on the basis of history and clinical features: a peripheral blood smear may suggest hemolysis; additionally a Gram stain of the exudate reveals large Gram-positive bacilli without neutrophils; and the biochemical profile may show metabolic acidosis and renal failure.
- Radiography can visualize gas in the soft tissues and computerized tomography (in other words, CT) scans are useful in patients with chest and abdominal involvement. [1]
Differential Diagnosis
Differential Diagnosis
Necrotizing Fasciitis:
- A rapidly progressing bacterial infection of the fascia (connective tissue) that can mimic the appearance of wet gangrene. It presents with severe pain, erythema, edema, and systemic toxicity.
Pyoderma Gangrenosum:
- A rare inflammatory skin condition characterized by painful ulcers that can resemble wet gangrene. It is often associated with underlying systemic diseases like inflammatory bowel disease or arthritis.
Deep Vein Thrombosis (DVT):
- DVT can cause limb ischemia and tissue necrosis, which may resemble dry gangrene. However, DVT typically presents with pain, swelling, and warmth in the affected limb, unlike the cold and insensate nature of dry gangrene.
Venous Stasis Ulcers:
- These chronic ulcers occur due to impaired venous return and can develop necrosis and a dark appearance. However, they are usually located on the lower legs and have a different clinical course than gangrene.
Calciphylaxis:
- This rare condition occurs in patients with end-stage renal disease and is characterized by skin necrosis due to calcium deposits in small blood vessels. It can resemble dry gangrene but is often associated with other signs of renal failure.
Warfarin Necrosis:
- This uncommon complication of warfarin therapy occurs due to rapid depletion of protein C, leading to skin necrosis. It can mimic dry gangrene but usually occurs within the first few days of warfarin initiation.
Atheroembolism:
- Embolization of cholesterol crystals from atherosclerotic plaques can cause digital ischemia and necrosis, resembling dry gangrene. However, it typically affects multiple digits and is associated with a history of vascular disease.
Important Considerations:
- History: A detailed history is crucial to distinguish between these conditions. Consider the patient’s underlying medical conditions, medications, and any recent trauma or infections.
- Physical Examination: A thorough physical examination should focus on the appearance, temperature, and sensation of the affected area, as well as signs of systemic illness.
- Laboratory Tests: Blood tests, wound cultures, and imaging studies can help confirm the diagnosis and identify the underlying cause.
It’s important to note: Gangrene is a medical emergency, especially wet and gas gangrene. Early recognition and prompt treatment are crucial to prevent complications and improve outcomes. [11]
Complications
Complications
Local Complications:
Infection and Sepsis: Gangrene, particularly wet gangrene, is often associated with bacterial infection.
Contractures: After healing from gangrene or amputation, scar tissue formation can lead to contractures, which are limitations in joint movement.
Systemic Complications:
Septic Shock: In severe cases, sepsis can progress to septic shock, a life-threatening condition characterized by dangerously low blood pressure and organ failure.
Multiple Organ Dysfunction Syndrome (MODS): MODS is a serious complication of sepsis and shock, where multiple organ systems (e.g., lungs, kidneys, liver) begin to fail.
Death: If left untreated, gangrene can be fatal due to the spread of infection, sepsis, and multi-organ failure.
Other Complications:
Chronic Pain: Even after successful treatment, some patients may experience chronic pain in the affected area due to nerve damage or phantom limb pain (in the case of amputation).
Psychological Distress: Gangrene and its complications, such as amputation, can have a significant psychological impact, leading to depression, anxiety, and post-traumatic stress disorder (PTSD). [12]
Important Note: The risk of complications increases with the severity and extent of gangrene, as well as the presence of underlying medical conditions (e.g., diabetes, peripheral vascular disease). Early recognition and prompt treatment of gangrene are crucial to minimize complications and improve outcomes.
Investigations
Investigations
Laboratory Tests:
- Complete Blood Count (CBC): Elevated white blood cell count may indicate infection.
- Blood Cultures: To identify the causative organism in cases of wet or gas gangrene.
- Metabolic Panel: To assess electrolyte levels, kidney function, and blood glucose levels, which can be affected in patients with gangrene.
- C-reactive Protein (CRP): Elevated levels indicate inflammation and may be useful in monitoring the response to treatment.
- Erythrocyte Sedimentation Rate (ESR): Elevated levels suggest inflammation and can be used to monitor disease activity.
Imaging Studies:
- Plain Radiographs: X-rays may show gas in the tissues in cases of gas gangrene or bone involvement.
- Computed Tomography (CT) Scan: CT scans can help assess the extent of tissue involvement and identify underlying causes like arterial occlusion.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of soft tissues and can help differentiate between viable and non-viable tissue.
- Angiography: This imaging test involves injecting a contrast dye into the blood vessels to visualize the blood flow and identify any blockages.
Other Investigations:
- Doppler Ultrasound: Can be used to assess blood flow in the affected area and detect any arterial or venous insufficiency.
- Tissue Biopsy: Biopsy of the affected tissue can confirm the diagnosis and identify the causative organism in cases of infection.
- Wound Cultures: Swabs of the wound can be taken to identify the bacteria causing the infection in wet gangrene.
Additional Considerations:
- The choice of investigations may vary depending on the suspected type and cause of gangrene.
- The clinical presentation and initial assessment of the patient will guide the selection of appropriate tests.
- Early diagnosis and prompt treatment are essential to prevent complications and improve outcomes in patients with gangrene. [13]
Treatment
Treatment
- High-dose penicillin G also clindamycin.
- Third-generation cephalosporins intravenously.
- The mainstay of management is early surgical excision of the necrotic tissue.
- The muscle planes open through generous longitudinal incisions and all devitalized tissue remove, going beyond the area of induration.
- Abdominal involvement may necessitate excision of the wall musculature.
- Excision should continue daily until the process of necrosis has stopped spreading.
- In established gas gangrene with systemic toxicity, amputation of the involved extremity is life saving and should not delay.
- The role of HBO is not as clear as in necrotizing fasciitis but it recommend in severe cases if the facilities are available. [1]
Prevention
Prevention of Gangrene
Manage underlying conditions:
- Diabetes: Control blood sugar levels meticulously.
- Peripheral artery disease (PAD): Quit smoking, manage blood pressure and cholesterol.
- Other conditions: Address any condition affecting blood circulation or immune function.
Wound care:
- Prompt treatment: Clean and disinfect any wounds immediately, no matter how small.
- Medical attention: Seek professional care for deep or infected wounds.
Foot care (especially for diabetics):
- Daily inspection: Check for cuts, sores, blisters, or any signs of infection.
- Proper hygiene: Wash and dry feet thoroughly.
- Protective footwear: Wear well-fitting shoes and avoid going barefoot.
Avoid frostbite:
- Proper clothing: Dress warmly in cold weather, covering exposed skin.
- Warm-up breaks: Take frequent breaks in warm areas during prolonged exposure to cold.
Healthy lifestyle:
- Balanced diet: Eat a nutritious diet to support overall health.
- Regular exercise: Improve circulation and overall fitness.
- Avoid smoking: Smoking significantly increases the risk of gangrene.
Reference:
- Book: "Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases"
- Edition: 9th Edition
- Writers: John E. Bennett, Raphael Dolin, Martin J. Blaser
- Year of Publication: 2020
- Publication: Elsevier
Note: This information is intended for general knowledge and informational purposes only, and does not constitute medical advice. It is essential to consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
Homeopathic Treatment
Homoeopathic Treatment of Gangrene
Homeopathic Treatment
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
1.Aconite:
- Deathly paleness of face also shuddering.
- The part first swells and then assumes a blackish color.
- Sleeplessness also restlessness.
- Chilliness from least uncovering; additionally, sweat cool in palms of hands; coldness of feet up to malleoli, with sweat on toes and soles of feet.
2.Arnica:
- In general, Hard, hot and shining swelling of parts affected; gangrene follows contused wounds.
- Thirst before fever; pain in periosteum of all the bones.
- Besides this, Pain in cartilage of ears, as if contused; swelling of nose, with feeling as if from ulceration of nostrils; tendency to boils also carbuncles
3.Arsenic Alb:
- Ulcers extremely painful or entirely insensible, with elevated edges.
- Secreting a bad, watery foetid ichors; hard, shining, burning swelling with bluish- black, burning vesicles, filled with acrid ichor.
- Aggravation especially from warmth, from cold; extreme restlessness.
- Moreover, Gangrene accompanied by foetid diarrhoea.
- Great weakness and emaciation; numbness, stiffness and insensibility of the feet.
- Lastly, General coldness with parchment-like dryness of the skin, followed by heat.
4.Asafoetida:
- Dark-red and hot swellings; bright-red appearance of the wounds.
- Which are sensitive to touch; coldness also dryness of skin with rapid pulse.
5.Aurum:
- Gangrenous diseases with edematous swelling of the parts; very sensitive to cold.
- Aggravate especially at night, disturbing sleep; low- spirited, with suicidal ideas.
6.Belladonna:
- Generally, Fiery redness of swelling, even Erysipelatous.
- Dry, hot skin, thirst also headache, Erysipelatous indurated swellings which mortify.
- Accompanied by glandular swellings; Besides this, secretions of bloody ichor.
7.Bromium:
- Hospital gangrene, death of the edges of the wound; cancerous ulcer in face.
- In detail, stony-hard swelling of glands, especially on lower jaw and throat.
- decayed teeth also gums; foul breath; much prostration and emaciation.
- Lastly, psoric constitution
8.Carbo veg:
- Humid gangrene in cachectic persons whose vital powers are exhausted.
- great foulness of the secretions; great prostration; sepsis; indifference; fainting after sleep, while yet in bed, morning; no restlessness.
9.China:
- In general, After profuse and frequently repeated hemorrhage.
- With coldness of the extremities or of the whole body, with pale also clammy face.
- Moreover, The parts around the wound become soft, blue and swollen.
- Bedsores in people who are much debilitated from excessive discharges.
10.Ephorbium:
- Gangrene following either gastritis or enteritis, temperature continually falling;
- inflammation also swelling, followed by cold gangrene; torpor; insensibility of parts affected;
- Lastly, chilliness and shuddering over whole body; gangrene senilis. [3]
Diet & Regimen
Diet And Regimen
- Eating an unhealthy diet high in fat will make any existing atherosclerosis worse and increase your risk of developing gangrene.
- Continuing to eat high-fat foods will cause more fatty plaques to build-up in your arteries. Additionally, This is because fatty foods contain cholesterol.
- There are 2 types of fat – saturated and unsaturated. Avoid foods that contain saturated fats because they increase levels of "bad cholesterol" in your blood.
Foods high in saturated fat include:
- Meat pies
- Sausages and fatty cuts of meat
- Butter & Ghee
- Cream
- Hard cheese
- Cakes and biscuits
- Food containing coconut or palm oil. [2]
Do’s and Don'ts
Do’s:
- Seek immediate medical attention: Gangrene is a medical emergency, and early intervention is crucial for the best possible outcome.
- Keep the affected area clean and dry: This helps prevent further infection and promotes healing.
- Elevate the affected limb: This can help reduce swelling and improve blood flow.
- Follow your doctor’s instructions carefully: This may include taking antibiotics, undergoing surgery, or other treatments.
- Manage underlying conditions: If you have conditions like diabetes or peripheral artery disease, managing them effectively can help prevent gangrene from recurring. [10]
Don’ts:
- Not ignore the symptoms: Pain, discoloration, numbness, or foul odor are signs that should not be ignored.
- Don’t attempt to treat gangrene at home: Self-treatment can be dangerous and may worsen the condition.
- Not apply heat to the affected area: Heat can increase the risk of infection and tissue damage.
- Don’t smoke: Smoking impairs blood flow and can worsen gangrene.
- Don’t delay seeking medical attention: Prompt treatment is essential to prevent complications and improve the chances of a full recovery.[10]
Important Note: This information is not a substitute for professional medical advice. Always consult with a healthcare provider for diagnosis and treatment.
Terminology
Terminology
- Gangrene: The death of body tissue due to a lack of blood flow or a serious bacterial infection.
- Ischemia: Inadequate blood supply to an organ or part of the body, often a precursor to gangrene.
- Necrosis: The death of cells or tissues within a living organism.
- Dry Gangrene: A form of gangrene where the tissue becomes dry and shrinks, usually due to a lack of blood supply.
- Wet Gangrene: A form of gangrene where the tissue is infected with bacteria, causing swelling and a foul odor.
- Gas Gangrene: A dangerous form of gangrene caused by bacteria that produce gas within the tissue.
- Debridement: The surgical removal of dead or damaged tissue.
- Amputation: The surgical removal of a limb or part of a limb.
- Sepsis: A life-threatening condition that arises when the body’s response to infection injures its own tissues and organs.www.rarediseasesjournal.com
Additional terms that may appear in gangrene-related articles:
- Peripheral Arterial Disease (PAD): A circulatory condition in which narrowed blood vessels reduce blood flow to the limbs, a major risk factor for gangrene.
- Diabetes Mellitus: A chronic condition characterized by high blood sugar levels, which can damage nerves and blood vessels, increasing the risk of gangrene.
- Frostbite: Injury to body tissues caused by exposure to extreme cold, which can lead to gangrene.
- Revascularization: A surgical procedure to restore blood flow to a blocked artery.
- Hyperbaric Oxygen Therapy (HBOT): A treatment that involves breathing pure oxygen in a pressurized chamber, sometimes used to treat certain types of gangrene.
Understanding these terms can help you better comprehend articles on gangrene and make informed decisions about your health or the health of someone you care for.
In homeopathic articles about gangrene, you might find these common terminologies, along with their meanings:
- Gangrene: The death and decay of body tissue, often caused by a lack of blood flow or a serious bacterial infection.
- Miasm: A predisposition to chronic disease, which is a central concept in homeopathic theory. There are three main miasms: psora (related to suppressed skin conditions), sycosis (related to overgrowth and excess), and syphilis (related to destructive processes). Understanding the miasm is considered important for selecting the appropriate homeopathic remedy.
- Remedy: A homeopathic medicine prepared from natural substances, used to treat specific symptoms and underlying imbalances.
- Proving: A process in homeopathy where healthy individuals take a substance and record their symptoms, which are then used to determine the substance’s therapeutic properties.
Repertory:
- A reference book used by homeopaths to find remedies that match a patient’s symptoms.
- Materia Medica: A comprehensive reference book that describes the properties and uses of homeopathic remedies.
- Potency: The strength or dilution of a homeopathic remedy. Higher potencies are considered more dilute and are thought to act on deeper levels.
- Aggravation: A temporary worsening of symptoms after taking a remedy, which is sometimes seen as a sign that the remedy is working.
- Constitutional Remedy: A remedy that matches the patient’s overall physical and mental characteristics, not just their specific symptoms.
Here are some additional terms you might find in homeopathic articles on gangrene:
- Vital Force: The energy or life force that animates the body and is considered essential for health in homeopathy.
- Law of Similars: The principle that a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
- Succussion: A specific method of shaking homeopathic remedies during preparation, believed to enhance their therapeutic properties.
Understanding these terms will help you navigate homeopathic articles on gangrene and have informed discussions with homeopathic practitioners.
References
Reference
- Bailey_and_Love_s_Short_Practice_of_Surgery
- https://www.nhs.uk/conditions/gangrene/prevention/]
- Homoeopathic Therpeutics by Lilienthal.
- Assessing the Prevalence Rate of Gangrene Among Patients With Peripheral Vascular Disease in a Tertiary Care Hospital in Central India (2024)
- (PDF) Fournier’s gangrene: Prospective study of 34 patients in South Indian population and treatment strategies (2018)
- Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice, 21st Edition
- Robbins and Cotran Pathologic Basis of Disease, 10th Edition
- Rubin, R., & Strayer, D. S. (Eds.). (2021). Rubin’s Pathology: Clinicopathologic Foundations of Medicine (8th ed.). Wolters Kluwer.
- Harrison’s Principles of Internal Medicine, 21st Edition
- Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9th Edition
- Fitzpatrick’s Dermatology in General Medicine, 9th Edition
- Schwartz’s Principles of Surgery, 12th Edition
- Current Surgical Diagnosis & Treatment, 16th Edition
- Rutherford’s Vascular Surgery and Endovascular Therapy, 10th Edition
Also Search As
Also Searched As
Online Databases:
- The Homoeopathic Journal: This peer-reviewed journal often publishes case reports and studies related to homeopathic treatment of various conditions, including gangrene.
- Indian Journal of Research in Homoeopathy (IJRH): This is another reputable journal that features research articles and case studies on homeopathic interventions.
- ResearchGate: This platform allows researchers to share their work, and you may find case reports or studies on gangrene treatment with homeopathy.
Homeopathic Websites and Blogs:
- HomoeoCARE: This website features case studies and articles on homeopathic treatment approaches, including successful cases of gangrene.
- National Center for Homeopathy (NCH): The NCH website may have resources, articles, or links to research on homeopathy for various conditions.
Search Engines:
- Using keywords like "homeopathic treatment of gangrene," "homeopathy for gangrene case studies," or "gangrene cured by homeopathy" on search engines like Google or DuckDuckGo can yield relevant results.
Libraries:
- University or medical libraries may have homeopathic journals and books that discuss gangrene and its treatment options.
Homeopathic Practitioners:
- Consulting a qualified homeopathic practitioner can provide personalized information and guidance on homeopathic approaches to gangrene.
Important Considerations:
- While homeopathic case reports and studies can be informative, it’s crucial to remember that gangrene is a serious medical condition requiring prompt conventional medical attention.
- Homeopathy should not be considered a replacement for conventional treatment but can be explored as a complementary therapy under the guidance of a qualified healthcare professional.
- Always consult with a doctor or healthcare provider before starting any new treatment, including homeopathic remedies.
By utilizing these resources, individuals can gather information on homeopathic approaches to gangrene and make informed decisions about their healthcare in consultation with a qualified practitioner.
Online Search Engines:
- Use search engines like Google, Bing, or DuckDuckGo to search for "gangrene." You can also use more specific search terms like "causes of gangrene," "symptoms of gangrene," or "treatment of gangrene."
- Look for reputable sources like medical websites (e.g., Mayo Clinic, Cleveland Clinic, WebMD), government health agencies (e.g., CDC, NIH), and academic institutions.
Medical Websites and Encyclopedias:
- Consult online medical encyclopedias like MedlinePlus, Merck Manual, or the Encyclopedia of Surgery.
- Look for articles and resources on specific types of gangrene (e.g., dry gangrene, wet gangrene, gas gangrene).
Medical Journals and Databases:
- If you are a healthcare professional or researcher, you can access medical journals and databases like PubMed, Cochrane Library, or EMBASE to search for scientific articles and research studies on gangrene.
Books and Textbooks:
- Consult medical textbooks like "Harrison’s Principles of Internal Medicine," "Schwartz’s Principles of Surgery," or "Tintinalli’s Emergency Medicine" for in-depth information on the pathophysiology, diagnosis, and treatment of gangrene.
Consult a Healthcare Professional:
- If you have any concerns about gangrene or suspect you may have it, consult a doctor or healthcare professional for diagnosis and treatment.
Additional Tips:
- Use keywords related to the specific aspect of gangrene you are interested in (e.g., "risk factors," "complications," "prevention").
- Use filters to narrow down your search results by date, source, or type of information (e.g., news, images, videos).
- Look for credible sources with up-to-date information and references to support their claims.
- Consult a medical professional for personalized advice and diagnosis.
By utilizing these resources, you can gather comprehensive information on gangrene from various sources and perspectives.
Frequently Asked Questions (FAQ)
What is gangrene?
Gangrene is the death of body tissue due to a lack of blood flow or a serious bacterial infection.
It can affect any part of the body but is most common in the extremities, like the toes, feet, fingers, and hands.
How is gangrene diagnosed?
Gangrene is typically diagnosed through a physical examination, medical history review, and additional tests like blood tests, imaging scans, or tissue biopsies.
Can homeopathy treat gangrene?
Yes,
Homeopathy can be considered a complementary approach to gangrene treatment, working alongside conventional medical care. It aims to support the body’s natural healing processes and address the underlying causes of the condition.
Is homeopathy safe for gangrene?
Homeopathic remedies are generally considered safe when used under the guidance of a qualified practitioner. However, gangrene is a serious condition and should always be treated with conventional medical care alongside any complementary therapies.
What are the causes of gangrene?
Gangrene can be caused by various factors, including:
Reduced blood flow (ischemia) due to peripheral artery disease, diabetes, or blood clots
Severe infections, especially those caused by certain types of bacteria * Physical trauma, such as frostbite or burns
Can homeopathy prevent gangrene?
Homeopathy may help prevent gangrene by addressing underlying risk factors and supporting overall health. However, conventional preventive measures like managing diabetes, maintaining good hygiene, and seeking prompt medical attention for wounds are crucial.
What are the symptoms of gangrene?
Symptoms of gangrene can vary depending on the type and location, but common signs include:
- Changes in skin color (e.g., blue, purple, black)
- Numbness or loss of sensation in the affected area Pain, swelling, or a foul odor
- Blisters or sores
What are the treatment options for gangrene?
Treatment for gangrene depends on the type, cause, and severity.It may include:
- Antibiotics to treat any underlying infection
- Surgery to remove dead tissue (debridement) Revascularization procedures to restore blood flow Hyperbaric oxygen therapy
- In severe cases, amputation may be necessary.
How does homeopathy work in cases of gangrene?
Homeopathy works on the principle of "like cures like,"
where a substance that can cause symptoms in a healthy person can cure similar symptoms in a sick person.
Homeopathic remedies are selected based on the individual’s unique symptoms and constitution, aiming to stimulate the body’s healing response.
