Botulism
Definition
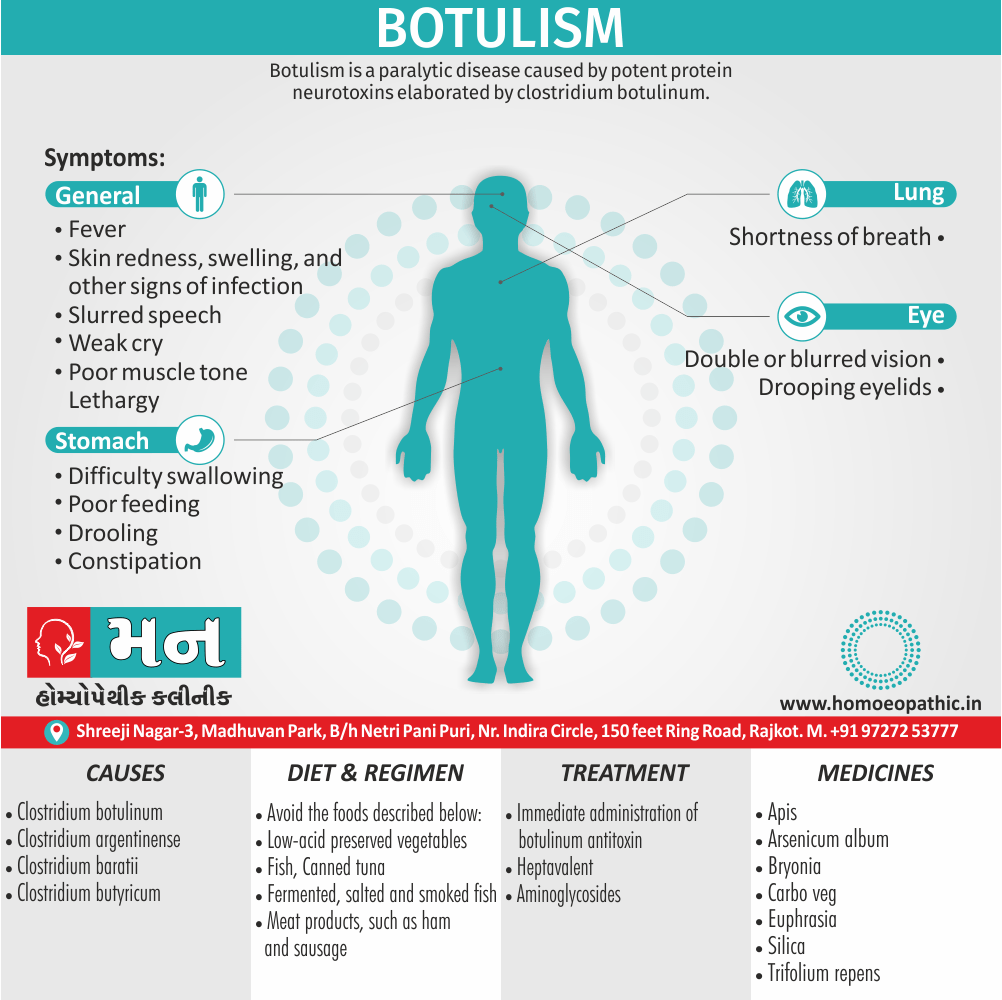
Botulism is a paralytic disease cause by potent protein neurotoxins elaborated by clostridium botulinum. [1]
Botulism doesn’t have true synonyms in the medical field, as it’s a specific illness caused by a particular toxin. However, there are some related terms you can use depending on the context:
- Clostridial foodborne botulism: This is a more specific term that clarifies the source of the botulism toxin (Clostridium bacteria) and the common transmission route (contaminated food).
- Infant botulism: This specifies the type of botulism that affects infants, caused by ingesting spores that germinate in their intestines.
- Wound botulism: This refers to botulism caused by the toxin entering the body through a wound.
- Inhalational botulism (rare): This is the rarest form, caused by inhaling botulinum toxin spores.
Informal Terms (use with caution):
- Food poisoning (ambiguous): This is a general term for various illnesses caused by contaminated food, not specific to botulism.
Important Considerations:
- In a medical setting, always use "botulism" or a more specific type (e.g., infant botulism) for clarity and accuracy.
- When discussing foodborne illness in general, "food poisoning" might be used, but it’s important to emphasize the need for proper diagnosis if botulism is suspected.
Additional Options:
- You could describe the symptoms of botulism, such as "paralysis caused by botulinum toxin." However, this wouldn’t be a direct synonym for the illness itself.
Remember:
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
Botulism, recognized at least since the eighteenth century, is a neuroparalytic disease cause by botulinum toxin, one of the most toxic substances known. While initially thought to cause only by the ingestion of botulinum toxin in contaminated food (food-borne botulism), three additional forms cause by in situ toxin production after germination of spores in either a wound or the intestine are now recognized worldwide: wound botulism, infant botulism, and adult intestinal colonization botulism.
In addition to occurring in these recognized natural forms of the disease, botulism symptoms have report in patients receiving injections of botulinum toxin for cosmetic or therapeutic purposes (iatrogenic botulism). Moreover, botulism was reported after inhalation of botulinum toxin in a laboratory setting.
Spread of Botulism
All forms of botulism manifest as a relatively distinct clinical syndrome of symmetric cranial-nerve palsies followed by descending bilateral flaccid paralysis of voluntary muscles, which may progress to respiratory compromise and death. The mainstays of therapy are meticulous intensive care and treatment with antitoxin as soon as botulism is suspected and before other illnesses have been ruled out.[1]
Botulism occurs worldwide, but the number of cases reported varies among countries and regions.
The variation may be due not only to actual differences in incidence but also to
(1) availability of resources to identify botulism, a rare disease
(2) differences in reporting requirements
(3) limited external access to data collections
There is no universal surveillance system to capture worldwide botulism incidence. However, 30 countries currently participate in voluntary reporting of botulism cases to the European Union through an established surveillance system that includes standardized case definitions similar to those used in the United States and Canada. Other countries (e.g., Argentina, China, Thailand, Japan) maintain independent botulism surveillance. [1]
Epidemiology
Epidemiology of Botulism
There is limited published data specifically on the Indian epidemiology of botulism. However, some studies and case reports mention botulism cases in India. One such reference is:
- "Botulism in India: A Review" (2016) by S. K. Sharma, et al.
This review article summarizes available information on botulism cases in India, including clinical presentations, causative agents, and risk factors. However, it does not provide a comprehensive epidemiological analysis due to the lack of systematic surveillance data. [5]
It’s important to note that this is a review article summarizing existing information up to 2016, and newer data may be available.
For the most up-to-date information on the Indian epidemiology of botulism, consulting recent publications in relevant medical journals or contacting public health authorities in India would be recommended.
Causes
Causes
Seven serologically distinct confirmed serotypes of botulinum toxin (A through G) have confirm. Botulinum toxin produce by four recognized species of clostridia: Clostridium botulinum, Clostridium argentinense, Clostridium baratii, and Clostridium butyricum. Certain strains may produce more than one serotype.
All are anaerobic gram positive organisms that form subterminal spores; C. botulinum and C. argentinense spores have recover from the environment. The spores survive environmental conditions and ordinary cooking procedures. Toxin production, however, requires a rare confluence of product storage conditions: an anaerobic environment, a pH of >4.6, low salt and sugar concentrations, and temperatures of >4°C. Although commonly ingested, spores do not normally germinate and produce toxin in the adult human intestine.[1]
Food-borne botulism
Food-borne botulism cause by consumption of foods contaminated with botulinum toxin; no confirmed host-specific factors involved in the disease. Wound botulism cause by contamination of wounds with C. botulinum spores, subsequent spore germination, and toxin production in the anaerobic milieu of an abscess or a wound.
Infant botulism
Infant botulism results from absorption of toxin produced in situ by toxigenic clostridia colonizing the intestine of children ≤1 year of age. Colonization thought to occur because the normal bowel microbiota not yet fully establish; this theory support by studies in animals. Adult intestinal colonization botulism, a very rare form that poorly understood, has a pathology similar to that of infant botulism but occurs in adults; typically, patients have some anatomic or functional bowel abnormality or have recently used antibiotics that may help toxigenic clostridia compete more successfully against the normal bowel microbiota.
Antitoxin treatment
Despite antitoxin treatment, relapse due to intermittent intraluminal production of toxin may observe in patients with adult intestinal colonization botulism.[1] Regardless of how exposure occurs, botulinum neurotoxin enters the vascular system and transport to peripheral cholinergic nerve terminals, including neuromuscular junctions, postganglionic parasympathetic nerve endings, and peripheral ganglia.
Botulinum toxin is a zinc-endopeptidase protein of ~150 kDa, consisting of a 100-kDa heavy chain and a 50-kDa light chain.
Steps in neurotoxin activity include
(1) Heavy-chain binding to nerve terminals
(2) Internalization in endocytic vesicles
(3) Translocation of the light chain to cytosol
(4) Light chain serotype-specific cleavage of one of several proteins involved in the release of the neurotransmitter acetylcholine.
Inhibition of acetylcholine release by any of the seven toxin serotypes results in characteristic flaccid paralysis. Recovery follows sprouting of new nerve terminals.
Botulinum toxin serotypes
All botulinum toxin serotypes have demonstrated to cause botulism in nonhuman primates. Human cases associated with serotypes A, B, E, and F are reported each year. Serotype A produces the most severe syndrome, with the greatest proportion of patients requiring mechanical ventilation. Serotype B appears to cause milder disease than type A in both food-borne and infant botulism.
Other serotype
Besides this, Serotype E, most often associated with foods of aquatic origin, produces a syndrome of variable severity. The rare cases of illness caused by toxin serotype F, whether in infants or adults, characterize by rapid progression to quadriplegia and respiratory failure but also by relatively rapid recovery.
Recent studies have shown that at least some serotypes can be differentiated into subtypes through neurotoxin gene sequencing; however, the impact of these subtype differences on clinical illness is not yet known. [1]
Types
Types
Food borne botulism: –
From 1899 to 2011, 1225 food-borne botulism events (single cases or outbreaks) reported in the United States; from 1990 to 2000, a median of 23 cases were reported annually. Most such events (~80%) involve vegetables or fish/ aquatic animals, usually home-preserved (canned, jarred). Native communities in both the United States (Alaska) and Canada have a high incidence of food-borne botulism due to traditional food preparation practices; 85% of all cases in Canada occur in Native communities. Outbreaks typically involve two or three cases; however, one restaurant-associated outbreak in 1977 affected 59 persons.
Wound botulism: –
This form of disease first recognized in 1951 as a result of a review of the clinical records on an accidental injury in 1943. Between 1943 and 2011, 491 cases of wound botulism were reported in the United States; 97% of cases reported after 1990 were associated with injection drug use. The typical patient a 30- to 50-year-old resident of the western United States with a long history of black-tar heroin injection. In the early 2000s, wound botulism associated with drug use emerged in Europe, and at least two case clusters have reported.[1]
Infant botulism: –
More than 3900 infant botulism cases have reported worldwide (84% in the United States alone) since this form of the disease first recognized in 1976; ~80–100 cases (commonly caused by serotypes A and B) reported annually in the United States.[1]
Adult intestinal colonization botulism.: –
This form of botulism difficult to confirm because it is poorly understand and because no clear guidelines are available to help differentiate it from other adult botulism cases. Often these cases cause by C. baratii type F, but the involvement of both C. botulinum type A and C. butyricum type E has report.[1]
Iatrogenic botulism: –
Paralysis of variable severity has followed injection of licensed botulinum toxin products for treatment of conditions involving hypertonicity of large muscle groups. The U.S. Food and Drug Administration received 658 reports of adverse events related to botulinum toxin use—some very serious—between 1997 and 2006. Although some patients had symptoms consistent with botulism, no cases laboratory confirmed. Injection of approved doses of licensed products for cosmetic purposes has not associated with botulism. However, four cases of laboratory-confirmed botulism resulted from illegal injection of research-grade toxin for cosmetic purposes in a U.S. medical facility in 2004[1]
Inhalational botulism: –
Inhalational botulism does not occur naturally. One report from Germany has described botulism resulting from possible inhalational exposure to botulinum toxin in a laboratory incident.[1]
Intentional botulism: –
Botulinum toxin has been “weaponized” by governments and terrorist organizations. An attack might use aerosolization of toxin or contamination of foods or beverages ranging in scope from small-scale tampering to contamination of a widely distributed food item. An unnatural event may be suggested by unusual relationships between patients (e.g., a visit to the same building), atypical exposure vehicles, or atypical toxin serotypes.[1]
Risk Factors
Risk factors :
Botulism risk factors can be characterized based on each type of botulism as follows:
Infant botulism
Infants are especially vulnerable to botulism. Risk factors for infant botulism include:
- Living in rural areas
- Consuming corn or corn-containing products
- Penetrating trauma
- Being in contact with soil
- Honey intake
- Slow intestinal movement
Foodborne botulism
Using home canning methods increase risk for contracting botulism.
- Canned food such as:
- Fish
- Vegetables
- Beets
- Corn
- Spinach
- String beans
- Chili peppers
- Asparagus
- Honey
- Processed cheese
- Ingestion of foods that are not freshly prepared
Canned foods provide an environment with optimal pH for clostridium botulinum to survive. Additionally, the anaerobic environment in canned products allows the bacteria to thrive.
Wound botulism
It is a rare type of the disease yet, it is important to know the risk factors in order to completely prevent it. Wound botulism risk factors include the following:
- Intravenous drug abuse
- Penetrating trauma with an infected object. (4)
Pathogenesis
Pathogenesis of Botulism
Toxin Production: Clostridium botulinum or related species (e.g., C. baratii, C. butyricum) produce botulinum neurotoxin (BoNT) under anaerobic conditions. BoNT is one of the most potent toxins known.
Toxin Acquisition: BoNT can be acquired through various routes:
- Ingestion: of preformed toxin in contaminated food (foodborne botulism).
- Wound Contamination: with spores that germinate and produce toxin in vivo (wound botulism).
- Intestinal Colonization: in infants, with subsequent toxin production (infant botulism).
- Inhalation: of aerosolized toxin (a potential bioterrorism threat).
Toxin Action: BoNT binds irreversibly to presynaptic nerve terminals at the neuromuscular junction (NMJ) and autonomic ganglia. It then enters the nerve terminal and cleaves specific SNARE proteins essential for acetylcholine (ACh) release.
Neuroparalysis: The blockade of ACh release results in flaccid paralysis, affecting both voluntary and involuntary muscles. The cranial nerves are usually affected first, followed by descending, symmetrical paralysis of the limbs and trunk. Autonomic dysfunction may manifest as constipation, urinary retention, and dry mouth.
Recovery: Recovery occurs as new nerve terminals sprout and restore neurotransmission. This process can take weeks to months, depending on the severity of intoxication and the availability of antitoxin therapy. [6]
Pathophysiology
Pathophysiology :
- Botulism is most commonly caused by neurotoxins produced by C. botulinum, but C. baratii produces similar neurotoxins (5, 6). These toxins have been designated by letters, and human botulism has been caused by toxins A, B, E, and F.
- The neurotoxins which cause botulism are the most potent toxins currently known and cause paralysis through the inhibition of acetylcholine release in human nerve endings.
Origin of Symptoms
- Symptoms may begin as a headache and vomiting and progress to proximal and then distal paralysis (6).
- Eventually respiratory failure may occur due to paralysis and the morality rate for botulism is currently only 3 to 5 percent, in part due to mechanical respiration technology
Clostridium Botulinum
- Clostridium botulinum is an obligate anaerobe that forms spores. The natural habitat for the Clostridium botulinum spores is the soil. The species of Clostridium botulinum is made up of 4 genetically diverse groups that do not have much in common other than the fact that they all produce the botulinum toxin.
- The botulinum toxin itself exists as 7 different antigenic types and these 7 antigenic types have been assigned a series of letters: A, B, C, D, E, F, G.
- These toxins have a specific definition, and they are defined by their inability to cross neutralize the other types.
- The botulinum molecule itself is composed of a heavy chain as well as a light chain polypeptide. It is referred to as a dichain polypeptide.
- The light chain of the toxin contains an endopeptidase that blocks acetylcholine-containing vesicles from being able to fuse with the membrane at the end of the motor neuron.
- If acetylcholine is not present, it will result in flaccid muscle paralysis.
- Many people may not realize it, but the commercial therapeutic procedure termed "Botox" actually contains the botulinum toxin.
- However, there is a very small amount of it present, otherwise it would present an extensive danger.
- A vial of type A preparation, which is currently licensed in the US, contains only about 0.005% of the lethal oral dose and 0.3% of the lethal inhalation
Classification
Clostridium botulinum is divided into 4 groups:
- Group I – can produce toxins specifically A, B, or F proteolytic
- Group II – can produce toxins specifically B, E, or F, nonproteolytic
- Group III – can produce toxins C or D
- Group IV – can produce toxin G but toxin G has not been shown to cause neuroparalytic illness.
- Honey, corn syrup, and other sweeteners are potentially dangerous for infants. This is partly because the digestive juices of an infant are less acidic than older children and adults, and may be less likely to destroy ingested spores.
- In addition, young infants do not yet have sufficient numbers of resident microbiota in their intestines to competitively exclude C. botulinum. Unopposed in the small intestine, the warm body temperature combined with an anaerobic environment creates a medium for botulinum spores to germinate, divide and produce toxin.
- Thus, C. botulinum is able to colonize the gut of an infant with relative ease, whereas older children and adults are not typically susceptible to ingested spores. C. botulinum spores are widely present in the environment, including honey.
- For this reason, it is advised that neither honey, nor any other sweetener, be given to children until after 12 months. Nevertheless, the majority of infants with botulism have no history of ingestion of honey, and the exact source of the offending spores is unclear about 85% of the time.
- Spores present in the soil are a leading candidate for most cases, and often a history of construction near the home of an affected infant may be obtained.(4)
Clinical Features
Clinical Features of Botulism
The clinical presentation of botulism typically involves:
Incubation Period: Varies depending on the type and amount of toxin exposure.
Early Symptoms (often the first to appear):
- Neurological:
- Blurred or double vision (diplopia)
- Drooping eyelids (ptosis)
- Difficulty swallowing (dysphagia)
- Slurred speech (dysarthria)
- Dry mouth (xerostomia)
- Gastrointestinal (less common, more frequent in foodborne botulism):
- Nausea
- Vomiting
- Abdominal pain
- Diarrhea
- Neurological:
Progressive Paralysis:
- Descending, symmetrical, flaccid paralysis, typically starting with cranial nerves and progressing to the limbs and trunk.
- Respiratory muscle weakness, leading to respiratory failure in severe cases.
- Autonomic dysfunction:
- Constipation
- Urinary retention
- Fixed/dilated pupils
- Decreased salivation and lacrimation
Other Findings:
- Absence of fever (afebrile)
- Normal sensation (intact)
- Normal mental status (unless hypoxic)
Specific features may vary depending on the type of botulism:
Infant botulism:
- Constipation (often the first sign)
- Weak cry
- Poor feeding
- Hypotonia ("floppy baby")
Wound botulism:
- May have signs of infection at the wound site (e.g., pain, erythema, purulence) (6)
Sign & Symptoms
Sign & Symptoms
No matter how you get botulism, the symptoms are usually the same. The most defining symptom is weakness that starts on both sides of your face, goes down to your neck, and then to the rest of your body.
Other early symptoms e.g.:
- Either Double or blurred vision
- Drooping eyelids
- Difficulty swallowing
- Slurred speech
- Shortness of breath
Other symptoms that can follow include vomiting, belly pain, and diarrhea. Later, you may have a very hard time urinating and have severe constipation. Symptoms do not include a fever.[1]
If you don’t get treatment, your symptoms could progress to paralysis of your arms and legs and the muscles used for breathing.[1]
Infants with botulism have symptoms that i.e.:
- Lethargy
- Poor muscle tone starting in the head and neck and moving down
- Poor feeding
- Drooling
- Weak cry
Symptoms of wound botulism
Symptoms of wound botulism are similar to general botulism but may take about 2 weeks to appear. They also can i.e.:
- Fever
- Skin redness, swelling, also other signs of infection
Symptoms of inhalation botulism
Symptoms of inhalation botulism are the same as those for general botulism but usually happen more quickly. Respiratory failure can occur.
Symptoms of adult intestinal toxemia
Symptoms of adult intestinal toxemiaare similar to infant botulism. They are the same as general botulism but may also include i.e.:
- Firstly, Constipation
- Secondly, Poor feeding
- Lastly, Lack of energy (lethargy)
Symptoms of iatrogenic botulism
Symptoms of iatrogenic botulism are the same as those seen in general botulism. Along with muscle weakness, you could have i.e.:
- Eye muscle weakness
- A hard time speaking
- A paralyzed face
- A thick, weak tongue
- Reduced gag reflex [1]
Cranial nerve deficits i.e.
- Diplopia, Dysarthria
- Dysphonia, Ptosis
- Ophthalmoplegia
- Facial paralysis
- Impaired gag reflex
- Pupillary reflexes may be depressed, also fixed or dilated pupils
- Autonomic symptoms such as dizziness, dry mouth, and very dry, occasionally sore throat are common.
- Constipation
- Respiratory failure may occur due to either paralysis of the diaphragm and accessory breathing muscles or pharyngeal collapse secondary to cranial nerve paralysis.
- Weakness descends, often rapidly, from the head to involve the neck, arms, thorax, and legs; occasionally, weakness is asymmetric.
- Deep tendon reflexes may be normal or may progressively disappear.
Other symptoms
- Paresthesias, while rare, have been reported and may represent secondary nerve compression from immobility due to paralysis.
- Absence of cranial nerve palsies or their onset after the appearance of other true neurologic symptoms makes botulism highly unlikely.
- Nausea, vomiting, and abdominal pain may precede or follow the onset of paralysis in food-borne botulism.
- Infants with botulism typically present with reduced ability to suck and swallow, constipation, weakened voice, ptosis, sluggish pupils, hypotonia, and floppy neck; as in adults, illness can progress to generalized flaccidity and respiratory compromise.[1]
Clinical Examination
Clinical examination :
Appearance of the patient– Patients of botulism may appear lethargic and dizzy, Infants appear pale with less crying and unable to eat
Vital signs- Botulism patients have normal vital signs., Unstable blood pressure and heart rate
Skin-In wound botulism, the following may be observed:
- Wounds
- Bruises
- Subcutaneous abscesses
- Pale skin with bruises and signs of penetrating trauma in infant.
HEENT-Absent or decreased gag reflex
- Tongue hypotonia
- Weakness of the eye muscles
- Nystagmus
- Ptosis
Abdomen: Paralytic ileus: Decreased or absent bowel sounds (Foodborne botulism)
Lungs: Bradypnea due to respiratory muscle paralysis
CVS-Normal heart sounds, No murmurs, gallops or rubs
Neuromscular:
- Absent or decreased deep tendon reflexes
- Motor deficit
- Facial nerve impairment
- Speech impairment
Extremities: Weakness of lower and upper extremities (4)
Diagnosis
Diagnosis
Botulism is diagnosed primarily on clinical grounds, with laboratory confirmation by specific tests that identify botulinum toxin in clinical and food samples. In the setting of an outbreak with multiple patients presenting to the same treatment facility, the diagnosis is apparent as long as physicians recognize that cases within a cluster may have varied signs and symptoms.
The temporal occurrence of two or more cases with symptoms compatible with botulism is essentially pathognomonic because other illnesses that resemble botulism do not usually occur in clusters. In lone (sporadic) cases, the diagnosis is often missed. The rarity of this disease prevents many physicians from gaining experience with its clinical diagnosis, and some patients present with signs and symptoms that do not fit the classic pattern. Assessing clinical characteristics of other paralytic illnesses in single cases is sometimes critical to rule in or rule out the diagnosis of botulism. [1]
In adults
a food history and the names of contacts who may have shared foods should be obtained before illness progresses to respiratory failure; specific questions should include information about the consumption of home-preserved and/or foreign foods and of products requiring refrigeration that have been left at room temperature in sealed plastic containers or bags. A history of recent consumption of home-canned food substantially enhances the probability of food-borne botulism.
Ascertainment of the patient’s behavioral history related to injection drug use is critical to the diagnosis of wound botulism unless an accidental wound is evident. A history of recent abdominal surgery or antibiotic use may 989 be important in the diagnosis of adult intestinal colonization botulism. [1]
Differential Diagnosis
Differential Diagnosis
The illnesses most commonly considered in the differential diagnosis of adult botulism cases include Guillain Barré syndrome (GBS), myasthenia gravis, stroke syndromes, Eaton Lambert syndrome, and tick paralysis. Less likely possibilities are poisoning by tetrodotoxin, shellfish, or a host of rarer agents and antimicrobial drug–associated paralysis. A thorough history and a meticulous physical examination can effectively eliminate most alternative diagnoses, but a workup for other diagnoses should not delay treatment with botulinum antitoxin. [1]
GBS
GBS, a rare autoimmune demyelinating polyneuropathy that often follows an acute infection, presents most often as an ascending paralysis. Case clusters are rare. Occasional GBS cases present as the Miller Fisher variant, whose characteristic triad of ophthalmoplegia, ataxia, and areflexia easily mistake for the early descending paralysis of botulism.
Pathogenesis
Protein levels in cerebrospinal fluid (CSF) elevate in GBS; because this increase may delay until several days after symptom onset, an early lumbar puncture with a negative result may need to repeat. In contrast, CSF findings generally normal in botulism, although marginally elevate CSF protein concentrations have reported. In experienced hands, electromyography may differentiate GBS from botulism.
edrophonium (Tensilon) test
The edrophonium (Tensilon) test is sometimes of value in distinguishing botulism from myasthenia gravis. In most cerebrovascular accidents, physical examination reveals asymmetry of paralysis and upper motor neuron signs. Brain imaging can reveal the rare basilar stroke that produces symmetric bulbar palsies. Eaton-Lambert syndrome usually manifests as proximal limb weakness in a patient already debilitated by cancer.
Tick paralysis
Tick paralysis is a rare flaccid condition closely resembling botulism and caused by neurotoxins of certain ticks. [1]
Complications
Complications of Botulism
The potential complications of botulism include:
Respiratory Failure:
- The most serious and life-threatening complication.
- Occurs due to paralysis of respiratory muscles, leading to inadequate ventilation.
- Requires prompt intervention with mechanical ventilation.
Aspiration Pneumonia:
- Risk increased due to impaired swallowing and gag reflex.
- Occurs when food, saliva, or gastric contents enter the lungs.
- Can lead to secondary infections and further respiratory compromise.
Prolonged Hospitalization and Rehabilitation:
- Severe cases may require prolonged intensive care and rehabilitation.
- Recovery from neurological deficits can take weeks to months.
- Physical therapy and occupational therapy may be needed to regain muscle strength and function.
Secondary Infections:
- Risk increased due to prolonged immobility and potential for aspiration.
- Urinary tract infections, pressure ulcers, and bloodstream infections can occur.
Psychological Impact:
- The experience of acute paralysis and potential for prolonged recovery can cause significant psychological distress.
- Anxiety, depression, and post-traumatic stress disorder (PTSD) may occur.
Long-Term Sequelae:
- Some patients may experience long-term fatigue, weakness, and exercise intolerance.
- Cognitive impairment and autonomic dysfunction can also persist in some cases. [6]
Investigations
Investigation
Botulism is confirmed in the laboratory by demonstration of toxin in clinical specimens (e.g., serum, stool, gastric aspirate, and sterile-water enema samples) or in samples of ingested foods.
Isolation of toxigenic clostridia from stool also provides evidence of botulism.
Wound cultures yielding the organism are highly suggestive in symptomatic cases.
mouse bioassay
The universally accepted method for confirmation of botulism is the mouse bioassay, which is available only in specialized laboratories.
Specific guidance about what specimens to collect should be obtained from the testing laboratory because the requirements vary with the form of botulism suspected.
Hospitalization
Clinical specimens collected early in the hospital admission process should be submitted for testing; toxin results may be negative if specimens are collected >7 days after symptom onset. Because of the extreme potency of botulinum toxin, a test may yield a negative result even when a patient has botulism; thus, a negative result does not exclude this diagnosis.
Nerve conduction studies
Nerve conduction studies showing reduced amplitude of motor potentials—with or without potentiation by rapid repetitive stimulation in weak muscles—and needle electromyography showing small-motor-unit action potentials are consistent with botulism; these results and those that make alternative diagnoses more likely may be useful. Standard blood work and radiologic studies are not useful in diagnosing botulism.[1]
Treatment
Treatment
The cornerstones of treatment for botulism are meticulous intensive care and immediate administration of botulinum antitoxin. Because antitoxin most beneficial early in the course of clinical illness. It should administer as soon as botulism suspect and before the time-consuming workup for other illnesses is complete.
Hosptalization
Persons of all ages in whom botulism suspect should hospitalize immediately so that respiratory failure—the usual cause of death—can detect and managed promptly.
Vital capacity should monitor frequently and mechanical ventilation provided as needed.
Botulinum antitoxin can limit the progression of illness because it neutralizes toxin molecules in the circulation that have not yet bound to nerve endings.
However, antitoxin does not reverse existing paralysis, which may take weeks to improve.
Vaccination
In the United States, there two license antitoxin products: Botulism Antitoxin Heptavalent an equine-derived heptavalent product enzymatically de-speciated for treatment of all forms of adult botulism and infant cases not involving serotypes A and B; and Botulism Immune Globulin Intravenous, a human derived product for treating infant botulism caused by serotype A and/or B only.
Antitoxin is also available in some other countries. Aminoglycosides and other medications that block the neuromuscular junction may potentiate botulism and should avoid. [1]
In wound botulism, suspect wounds and abscesses should cleaned, debrided, and drained promptly.
Medications
The role of penicillin and metronidazole in treatment and decolonization is unclear.
It has hypothesize that antimicrobial agents may increase circulating botulinum toxin from lysis of bacterial cells. Person-to-person transmission of botulism does not occur.
Universal precautions the only infection-control measures require during inpatient care. [1]
Prevention
Prevention
No prophylaxis or licensed vaccine is available against botulism. Home canning instructions and equipment have changed over the years. Up-to-date canning instructions from reliable sources should follow to ensure food safety. Processed food should store properly and heated thoroughly prior to consumption.
Because of the possible presence of spores, honey should not give to infants (≤12 months of age). Injection of illicit drugs should avoid. All wounds should be meticulously cleaned to eliminate possible contamination with bacterial spores.
Role of clinician
Clinicians should educate individuals or family members of at-risk individuals, including infants, illegal drug users, and preparers of home-preserved foods.[1]
Homeopathic Treatment
Homeopathic Treatment :
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Botulism:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Medicines:
Arsenicum album:
With nausea and vomiting. Burning in the stomach. Additionally, Restlessness. Despairing. Intense thirst – drinks little but often. Craves ice water which vomit (Phos.). Violent abdominal pains. Rolls about in anguish. Worse after (1) spoiled food, especially meat and watery fruit.
Carbo veg:
Patient is lifeless. Cold body and breath (but hot head). Weak pulse, quick breathing -needs air (to be fanned). Skin blue. Flatulent. Loud belching. Burning in stomach. Vomiting of blood.
Apis:
Confluent eruption, with pronounced oedema of the skin; oedematous swelling of the throat; cerebral complications.
Bryonia:
Cases calling for Bryonia characterize by a predominance of catarrhal symptoms from the very beginning with tendency to extend the finer bronchial tubes. Additionally, involve the pulmonary parenchyma. The rash slow in coming out, but, when once establish, it is usually abundant and characteristic. The accompanying symptoms are dry, painful cough. Furthermore, great lassitude and irritability anorexia, with thirst for large quantities of water; constipation, etc. Bryonia look upon somewhat as a specific to bring out the rash. On the other hand, any well-selected remedy will accomplish the same result.
Euphrasia:
Profuse corroding discharge from the eyes, with profuse, bland, nasal discharge.
Trifolium repens:
This remedy, the white clover, in the 3rd potency, is a remedy for the slobbering, drooling, or slavering of infants, or others- so they say.
Silicea:
In brief, Blindness-Momentary attacks of sudden blindness.
Diet & Regimen
Diet & Regimen
Must avoid this type of food:
- The botulism toxin has found in a variety of foods, including low-acid preserved vegetables. For example; green beans, spinach, mushrooms and beets; fish, including canned tuna, fermented, salted and smoked fish. Besides this; meat products, such as ham and sausage [2]
Do’s and Don'ts
The Do’s & Dont’ts
Do’s:
Food Safety:
- Wash hands thoroughly before handling food.
- Cook food thoroughly, especially meat and poultry.
- Store food properly at safe temperatures.
- Avoid eating food from bulging or damaged cans.
- Boil home-canned foods for 10 minutes before consuming.
Infant Care:
Wound Care:
- Clean wounds properly and seek medical attention for infected wounds.
- Be aware that wound botulism can occur even without visible signs of infection.
Medical Attention:
- Seek immediate medical attention if you suspect botulism.
- Inform healthcare providers of any recent food consumption or wound injuries.
Don’ts:
Food Handling:
- Do not taste or consume food that looks or smells spoiled.
- Do not eat food from cans with bulging lids or leaks.
- Do not store garlic or herb-infused oils at room temperature.
Infant Feeding:
- Do not feed honey to infants under 12 months of age.
Wound Care:
- Do not ignore wounds, even if they seem minor.
- Do not delay seeking medical care for infected wounds.
General:
- Do not panic. Botulism is rare but treatable with prompt medical attention.
- Do not self-treat. Seek professional medical advice for diagnosis and treatment.
Terminology
Terminology
Here’s a breakdown of the medical terminologies used in the homeopathic article, along with their meanings in the context of botulism:
Clinical Terminology
- Neuroparalytic: A condition where the nervous system is damaged, leading to paralysis (loss of muscle function).
- Neurotoxins: Poisons that specifically target and damage the nervous system.
- In situ: In its original place or position (e.g., toxin produced within the body).
- Anaerobic: An environment lacking oxygen.
- Abscess: A swollen area within body tissue, containing pus.
- Microbiota: The community of microorganisms (bacteria, fungi, etc.) that live in a particular environment, like the gut.
- Antibiotics: Medications that kill or inhibit the growth of bacteria.
- Pathognomonic: A sign or symptom that is uniquely characteristic of a particular disease.
- Sporadic: Occurring occasionally or in isolated instances.
- Quadriplegia: Paralysis of all four limbs.
- Ascending Paralysis: Paralysis that starts in the lower extremities and moves upward.
- Demyelinating Polyneuropathy: A disorder where the protective covering (myelin) of nerves is damaged.
- Ataxia: Loss of coordination of muscle movements.
- Areflexia: Absence of reflexes.
- CSF: Cerebrospinal fluid, a clear fluid that surrounds the brain and spinal cord.
- Electromyography: A diagnostic test that assesses the health of muscles and the nerves controlling them.
- Edrophonium Test: A test used to diagnose myasthenia gravis, a neuromuscular disorder.
- Bulbar Palsies: Weakness or paralysis of muscles supplied by cranial nerves (those that control the face, throat, etc.).
- Debrided: The removal of damaged tissue or foreign objects from a wound.
- Lysis: The breakdown or destruction of cells.
Homeopathic Terminology
- Miasmatic Tendency: In homeopathy, a predisposition to certain types of illnesses.
- Catarrhal Symptoms: Inflammation of mucous membranes, producing increased mucus.
- Potency: In homeopathy, the number of times a substance has been diluted and shaken.
- Constitutional Indications: The overall physical and mental characteristics of a patient used to guide homeopathic treatment.
References
Reference
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- https://www.webmd.com/food-recipes/food-poisoning/what-is-botulism
- A Complete Repertory of The Tissue Remedies of Schussler by S. F. Shannon
- Botulism in India: A Review (2016) by S. K. Sharma, et al.
- Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases (9th edition, 2020) by John E. Bennett, Raphael Dolin, and Martin J. Blaser (published by Elsevier).
Also Search As
Botulism Also Search As
Broad Terms:
- Botulism Symptoms and Treatment
- Clostridium Botulinum Infection
- Food Poisoning Paralysis
- Homeopathic Remedies for Foodborne Illness
Specific Terms:
- Infant Botulism Risk Factors
- Wound Botulism Diagnosis
- Neurotoxin Mechanism of Action
- Homeopathic Treatment for Neurological Conditions
- Food Preservation Safety Guidelines
Related Conditions:
People could find this article by searching for:
Specific Keywords:
Keyword Phrases:
Questions:
To further optimize the article’s visibility, you could:
- Include relevant tags: Add tags like "botulism," "homeopathy," "food poisoning," "neurotoxin," etc., to the article.
- Share on social media: Promote the article on relevant social media platforms with the appropriate hashtags.
- Link from other articles: If you have other articles related to botulism or homeopathy, link to this article for further reading.
- Submit to relevant websites: Consider submitting the article to websites or forums that focus on homeopathy or food safety.
Given that this article appears to be on a website, there are a few ways people could find it:
1. Through the Website’s Search Function:
- Most websites have a search bar. Users could type keywords like "botulism," "homeopathy," or "food poisoning" into the site’s search to potentially find this article.
2. Through External Search Engines (Google, Bing, etc.):
- Specific Keywords: Searching for precise terms like "botulism homeopathic treatment" or "clostridium botulinum homeopathy" could lead directly to the article.
- Keyword Phrases: Broader phrases like "homeopathic remedies for food poisoning" or "natural treatments for botulism" might also surface the article in search results.
- Questions: Typing a question like "Can homeopathy help with botulism?" could lead search engines to suggest this article as a potential answer.
3. Through Links from Other Websites or Articles:
- If other websites or articles reference this content, they might include a hyperlink directly to it.
- Backlinks can be a powerful way to drive traffic to specific articles.
4. Through Social Media Shares:
- If the website or others share the article on social media platforms, users who follow those accounts or search relevant hashtags could discover it.
Tips for Improving Searchability:
- Optimize the Article Title: Make sure the article title clearly reflects the content and includes relevant keywords.
- Use Meta Descriptions: These are short summaries that appear in search engine results. A well-crafted meta description can entice users to click on the article.
- Internal Linking: Link to this article from other relevant pages on the website to create a web of interconnected content.
Frequently Asked Questions (FAQ)
What is botulism and how is it caused?
Botulism is a rare but serious illness caused by a neurotoxin produced by the bacterium Clostridium botulinum. It can be acquired through contaminated food, infected wounds, or in infants, through intestinal colonization
What are the symptoms of Botulism?
- Double or blurred vision
- Drooping eyelids
- Difficulty swallowing
- Slurred speech
- Shortness of breath
- Vomiting, belly pain, diarrhea
How can I prevent botulism?
Preventing botulism involves safe food handling practices, especially with home-canned foods, avoiding honey for infants under one year old, and prompt wound care to prevent infection.
What are the causes of Botulism?
- Clostridium botulinum
- Clostridium argentinense
- Clostridium baratii
- Clostridium butyricum
How is botulism diagnosed and treated?
Diagnosis involves a combination of clinical examination, patient history, and laboratory tests to detect the botulinum toxin. Treatment primarily focuses on prompt administration of antitoxin and supportive care.
Can homeopathic remedies help with botulism?
While homeopathy is sometimes used as a complementary therapy, it’s crucial to seek immediate medical attention for botulism as it can be life-threatening. Conventional medical treatment, including antitoxin, is essential.
What is the conventional treatment for botulism?
Conventional treatment involves immediate administration of botulinum antitoxin to neutralize the toxin, along with supportive care in a hospital setting, which may include mechanical ventilation if breathing is impaired.
Can homeopathic remedies be used for botulism?
Homeopathy can be considered a complementary approach, but it should not replace conventional medical treatment for botulism. If you suspect botulism, seek immediate medical attention. Homeopathic remedies like Arsenicum album or Carbo veg may help address specific symptoms under the guidance of a qualified homeopath.
