Piles or Haemorrhoid
Definition
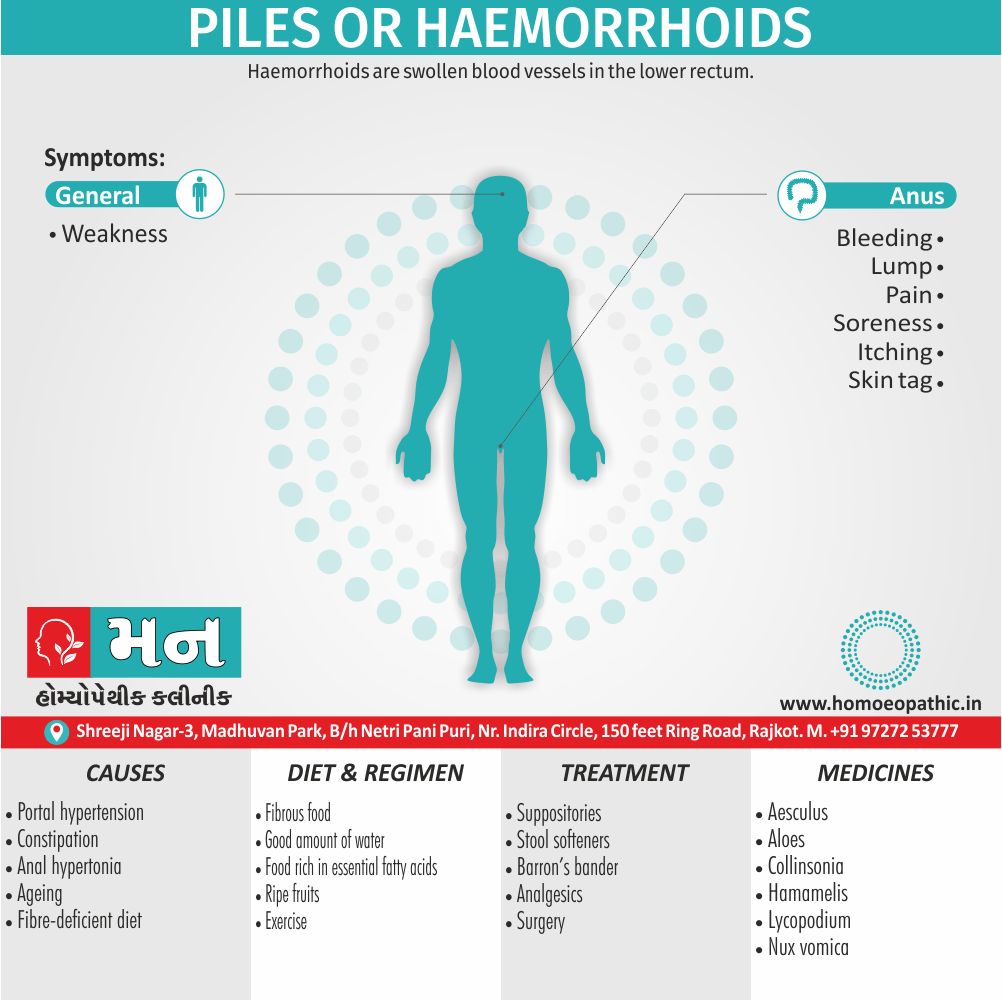
Piles or Haemorrhoid are swollen blood vessels in the lower rectum. Hemorrhoids, also spelled hemorrhoids, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool control. They become a disease when swollen or inflamed; the unqualified term "hemorrhoid" is often used to refer to the disease.
Here are some synonyms for Piles:
Piles as a hemorrhoid condition:
- Hemorrhoids (the most common and medical term)
- Varicose veins of the anus and rectum
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Piles or Haemorrhoid
Symptomatic hemorrhoids affect >1 million individuals in the Western world per year.
The Prevalence of hemorrhoidal disease is not selective for age or sex. However, Age known to be a risk factor. The prevalence of hemorrhoidal disease less in underdevelope countries.
The typical low-fiber, high-fat Western Diet associate with constipation and straining and the development of symptomatic hemorrhoids.
Epidemiology
Epidemiology
The prevalence of hemorrhoids in India is significant, affecting a substantial portion of the population. While estimates vary, studies suggest that roughly 10-12% of Indians experience hemorrhoids at some point in their lives. Certain factors contribute to this prevalence:
- Dietary Habits: Low fiber intake, common in many Indian diets, can lead to constipation and straining, increasing the risk of hemorrhoids.
- Sedentary Lifestyles: Lack of physical activity, especially prevalent in urban areas, contributes to constipation and weakens pelvic floor muscles.
- Delayed Bowel Movements: The cultural tendency to postpone bowel movements can lead to straining and increased pressure on the anal veins.
Specific studies highlight the epidemiological picture:
- A study published in the International Journal of Surgery (2016) found a prevalence of 10.1% in a semi-urban population.[5]
- Another study published in Surgical Review (2020) examined hospital admissions and reported a male predominance (69% male, 31% female) and a higher prevalence in the 20-40 age group.[6]
- A survey published in Colorectal Disease (2021) found an overall prevalence of 11%, with higher rates in urban areas and increasing risk with age.[7]
These figures underscore the widespread nature of hemorrhoids in India and highlight the need for increased awareness and preventive measures.
Key Points:
- Prevalence: 10-12% of the Indian population is affected by hemorrhoids.
- Risk Factors: Low-fiber diets, sedentary lifestyles, delayed bowel movements.
- Demographics: Higher prevalence in urban areas, men, and increasing age.
Causes
Causes of Piles or Haemorrhoid
Portal hypertension and varicose veins
- Misconceptions concerning the vascular anatomy of the anal canal led to theories of development of primary internal haemorrhoids that lasted for several centuries.
- Man’s upright posture, lack of valves in the portal venous system and raised abdominal pressure were thought to contribute to the development of anal varicosities.
- If raised portal venous pressure were indeed the cause, one would expect a high incidence in subjects suffering from portal hypertension.
- However, although such patients have a higher incidence of anorectal varices, these are a separate anatomical and clinical entity from Haemorrhoid, which are seen no more frequently than in those without cirrhosis, portal hypertension and esophageal varices.
- Other vascular causes Historically, some considered Haemorrhoid to be hemangiomatous or to result from changes in the erectile tissue that forms part of the continence mechanism, such as hyperplasia of the ‘corpus cavernous recti’.
Infection
- Repeated infection of the anal lining, secondary to trauma at defaecation, has been postulated as a cause of weakening and erosion of the walls of the veins of the submucosa.
- This hypothesis is difficult to accept, as one of the truly incredible properties of the anal canal is its resistance to infection, as well as the ability of its mucosa to heal after surgical intervention despite the torrent of micro-organisms passing over it.[3]
Diet and stool consistency
- Much emphasis has been placed on the role of constipation in the development of Haemorrhoid and, indeed, much of the management of sufferers involves attempts to ‘normalize’ bowel habits.
- A fibre-deficient diet results in a prolonged gut transit time, which is associated with the passage of smaller, harder stools that require more straining to expel.
- The presence of a hard Faecal mass in the Rectum could obstruct venous return, resulting in engorgement of the anal veins with the act of straining at stool or sitting for prolonged periods on the lavatory with a relaxed perineum, causing a disturbance of vascular flow.
- However, the epidemiological pattern of constipation is different from that of Haemorrhoidal disease and, indeed, an association has been demonstrated between haemorrhoids and diarrhoeal disorders.
Anal hypertonia
- The association between raised anal canal resting pressure and haemorrhoids is well known, but whether anal hypertonia causes symptoms attributable to haemorrhoids or whether anal cushion hypertrophy causes anal hypertonia is a subject of debate.
- The fact that surgical hemorrhoidectomy restores resting pressures to the normal range is not absolute evidence that the pile masses themselves are the cause of the hypertonia.
- It should be remembered, however, that there are a significant proportion of patients who suffer Haemorrhoidal symptoms in whom the anal canal is relatively patulous, and there is mucosal prolapse, which is associated with perineal descent and pudendal neuropathy.
Ageing
- In contrast to the anal cushion of early life, with age, the supporting structures show a higher proportion of collagen than muscle fibres and are fragmented and disorganised.
- Presumably, these changes arise over time with continued use of the anal canal for defaecation.
- However, similar changes are noted histologically in surgically excised haemorrhoids in younger patients.
- Current view Shearing forces acting on the anus lead to caudal displacement of the anal cushions and mucosal trauma. With time, fragmentation of the supporting structures leads to loss of elasticity of the cushions such that they no longer retract following defaecation.[1][3]
Types
Classification of Piles or Haemorrhoid
Hemorrhoids are commonly classified as
[1] External
- External Hemorrhoids originate below the dentate line and are covered with squamous epithelium and are associated with an internal component.
- External hemorrhoids are painful when thrombosed.
[2] Internal
- Internal hemorrhoids originate above the dentate line and are Covered with mucosa and transitional zone epithelium and represent majority of hemorrhoids.
- The standard classification of hemorrhoidal disease is based on the progression of the disease from their normal internal location to the prolapsing external position.[3]
Risk Factors
Risk Factors of Piles
- Chronic Constipation or Diarrhea: Straining during bowel movements or frequent loose stools can put pressure on the veins in the anal canal, leading to hemorrhoids.
- Pregnancy: The growing uterus and hormonal changes can increase pressure on the veins in the pelvic area, contributing to hemorrhoids.
- Low-Fiber Diet: A diet low in fiber can cause constipation, which is a risk factor for hemorrhoids.
- Heavy Lifting: Lifting heavy objects can put pressure on the veins in the pelvic and anal area, increasing the risk of developing hemorrhoids.
- Aging: As we get older, the tissues that support the veins in the anal canal can weaken, making hemorrhoids more likely.
- Sitting for Long Periods: Prolonged sitting, especially on the toilet, can increase pressure on the veins in the anal canal.
- Family History: If your family members have had hemorrhoids, you may be at an increased risk of developing them.[8]
Pathogenesis
Pathogenesis of Hemorrhoids (Piles)
The development of hemorrhoids is a multifactorial process involving several contributing factors:
Increased Intra-abdominal Pressure:
- Straining during defecation due to constipation is a major contributing factor.
- Chronic diarrhea, pregnancy, obesity, and heavy lifting can also increase intra-abdominal pressure.
- This elevated pressure transmits to the veins in the anal canal, leading to their engorgement and dilatation.
Weakening of Supporting Structures:
- The connective tissue and muscle fibers that support the anal cushions can weaken with age or due to chronic straining.
- This weakening allows the anal cushions to slide downwards, further contributing to venous engorgement.
Vascular Factors:
- The veins in the anal canal have a tendency to dilate and become tortuous.
- Increased blood flow to the area due to hormonal changes (e.g., during pregnancy) or inflammation can exacerbate this.
- The formation of arteriovenous shunts (abnormal connections between arteries and veins) may also play a role in some cases.
Dietary and Lifestyle Factors:
- A low-fiber diet can lead to constipation and straining, increasing the risk of hemorrhoids.
- Sedentary lifestyle and prolonged sitting can also contribute to venous stasis and engorgement.
Note: The pathogenesis of hemorrhoids is a complex process, and ongoing research continues to explore the underlying mechanisms involved.[9]
Pathophysiology
Anatomy and Pathophysiology of Piles or Haemorrhoid
Hemorrhoidal cushions are a normal part of the anal canal. The vascular structures contained within this tissue aid in continence by preventing damage to the sphincter muscle.
Three main hemorrhoidal complexes traverse the anal canal—the left lateral, the right anterior, and the right posterior. Engorgement and straining lead to prolapse of this tissue into the anal canal.
Over time, the anatomic support system of the hemorrhoidal complex weakens, exposing this tissue to the outside of the anal canal where it is susceptible to injury. [3]
Clinical Features
Clinical Features
Bleeding:
- The most common symptom.
- Typically bright red blood on toilet paper, in the toilet bowl, or dripping after defecation.
- Can range from mild spotting to significant blood loss.
Prolapse:
- Sensation of a lump or protrusion from the anus.
- May occur during defecation and reduce spontaneously or require manual reduction.
- Can cause discomfort, pain, and mucus discharge.
Pain:
- Usually associated with thrombosed external hemorrhoids or incarcerated prolapsed hemorrhoids.
- Described as a sharp, severe pain or a constant ache.
Pruritus (Itching) and Irritation:
- Due to mucus discharge or skin irritation from prolapse.
- Can lead to scratching and further discomfort.
Soiling:
- Leakage of mucus or stool due to incomplete closure of the anal canal from prolapsed hemorrhoids.
Thrombosis:
- Formation of a blood clot within an external hemorrhoid.
- Presents as a painful, bluish lump at the anal verge.
Additional Considerations:
- Symptoms can vary in severity and may be intermittent.
- Internal hemorrhoids are often asymptomatic unless they prolapse or bleed.
- External hemorrhoids are typically more painful,especially when thrombosed.
- Chronic hemorrhoids can lead to skin tags and anal fissures.
Sign & Symptoms
Sign & Symptoms of Piles or Haemorrhoid
External Hemorrhoids
- If not thrombosed, external hemorrhoid may cause few problems.
- However, when thrombosed, hemorrhoids may be very painful.
- Nevertheless, this pain typically resolves in two to three days.
- The swelling may, however, take a few weeks to disappear. A skin tag may remain after healing.
- If hemorrhoids are large and cause issues with hygiene, they may produce irritation of the surrounding skin, and thus itchiness around the anus. [1][3]
Internal Hemorrhoids
- Internal hemorrhoids usually present with painless, bright red rectal bleeding during or following a bowel movement.
- The blood typically covers the stool is on the toilet paper, or drips into the toilet bowl. The stool itself is usually normally colored.
- Other symptoms may include mucous discharge, a perianal mass if they prolapse through the anus, itchiness, and fecal incontinence.
- Internal hemorrhoids are usually painful only if they become thrombosed or necrotic.
- Bleeding, As the name Haemorrhoid implies, is the principal and earliest symptom. The nature of the bleeding is characteristically separate from the motion and seen either on the paper on wiping or as a fresh splash in the pan.
- Very rarely, the bleeding may sufficient to cause anemia.
- Pain is not commonly associated with the bleeding and its presence should make the clinician alert to the possibility of another diagnosis; however, pain may result from congestion of pile masses below a hypertonic sphincter.
Internal Hemorroids
- Piles associated with bleeding Alone call first-degree haemorrhoids.
- Patients may complain of true ‘piles’, lumps that appear at the anal orifice during defaecation and which return spontaneously afterwards (second-degree haemorrhoids), piles that have to replace manually (third-degree haemorrhoids). Or piles that lie permanently outside (fourth-degree haemorrhoids).
- By this stage there is often a significant cutaneous Component to the pile masses, which arise through repeated congestion and Oedema.
- In addition to the main symptoms of pain and prolapse, patients may complain of anal irritation, which may occur as a result of mucus secretion from the caudally displaced rectal mucosa, minor leakage through a now imperfect anal seal or difficulties in cleaning after defaecation because of the irregularity of the anal verge.[1][3]
Clinical Examination
Clinical Examination
Inspection:
Perianal Region:
- Look for skin tags, excoriation, inflammation, fistulae, fissures, and external hemorrhoids.
- Note any prolapse or evidence of thrombosis.
Position:
- Ask the patient to bear down or strain.
- Observe for prolapse of internal hemorrhoids.
Digital Rectal Examination (DRE):
Lubricated Glove:
- Perform a gentle DRE with a well-lubricated gloved finger.
Internal Hemorrhoids:
- Assess for the presence, size, and degree of prolapse of internal hemorrhoids.
Sphincter Tone:
- Evaluate anal sphincter tone.
Other Pathology:
- Rule out other anorectal pathology like tumors, polyps, or strictures.
Proctoscopy/Anoscopy:
Visualization:
- If indicated, perform proctoscopy or anoscopy for direct visualization of the anal canal and lower rectum.
- Look for internal hemorrhoids and any other mucosal abnormalities.[3]
Diagnosis
Diagnosis of Piles or Haemorrhoid
- Your doctor might be able to see external haemorrhoids. Diagnosing internal haemorrhoids might include examination of your anal canal and rectum.
- Digital examination- Your doctor inserts a gloved, lubricated finger into your rectum. They feels for anything unusual, such as growths.
- Visual inspection- Because internal haemorrhoids are often too soft to be felt during a rectal exam, your doctor might examine the lower portion of your colon and rectum with an anoscope, proctoscope or sigmoidoscope.[4]
Differential Diagnosis
Differential Diagnoses of Piles (Hemorrhoids)
- Anal Fissure: A tear in the lining of the anus, often causing pain during bowel movements and bleeding.
- Anal Fistula: An abnormal tunnel connecting the anal canal to the skin near the anus, usually resulting from an infection.
- Rectal Prolapse: The protrusion of the rectum through the anus.
- Rectal Cancer: A malignant growth in the rectum.
- Condyloma Acuminata (Anal Warts): Warts caused by the human papillomavirus (HPV) in the anal area.
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis can cause inflammation in the intestines, leading to bleeding and other symptoms.
- Sexually Transmitted Infections (STIs): Certain STIs can cause lesions or sores in the anal area, sometimes mimicking hemorrhoid symptoms.[8]
Note: It’s always recommended to consult a healthcare professional for any concerns related to piles or other anorectal conditions. They can conduct a thorough examination and provide accurate diagnosis and treatment.
Complications
Complications of Piles:
- Bleeding: This is the most common complication, and it can range from mild spotting to heavy bleeding.
- Thrombosis: A blood clot can form in a hemorrhoid, causing severe pain and swelling.
- Strangulation: A hemorrhoid can become trapped outside the anus, cutting off its blood supply. This is a medical emergency.
- Infection: Hemorrhoids can become infected, leading to abscess formation.
- Anemia: Chronic blood loss from hemorrhoids can lead to iron-deficiency anemia.
- Fecal incontinence: In rare cases, severe hemorrhoids can damage the anal sphincter muscles, leading to fecal incontinence.[8]
Investigations
Investigations for Piles (Hemorrhoids)
Digital Rectal Examination (DRE)
This is the initial step in evaluating a patient with suspected piles. It helps assess the presence, size, and location of hemorrhoids, as well as any other anorectal pathology.[9]
Anoscopy
This involves using a short, lighted tube to visualize the lower rectum and anal canal, allowing for a closer examination of internal hemorrhoids.[8]
Proctoscopy/Sigmoidoscopy
These procedures allow visualization of a larger portion of the rectum and lower colon, aiding in the diagnosis of internal hemorrhoids and excluding other conditions like colorectal cancer, especially in patients over 50 years old or with red flag symptoms.[3]
Colonoscopy
This may be recommended in specific cases, such as patients with a family history of colorectal cancer or those with symptoms suggestive of other colonic pathology.[10]
Additional Investigations (if indicated)
Laboratory Tests:
- Complete blood count (to check for anemia due to bleeding)
- Stool occult blood test (to detect hidden blood in the stool)
Imaging Studies:
- Anorectal ultrasound or MRI (rarely needed, but may be helpful in complex cases or to evaluate for other conditions)
Important Considerations:
Tailor investigations based on:
- Patient’s symptoms
- Age
- Risk factors
- Clinical findings
Always consider alternative diagnoses: Other anorectal conditions can mimic piles, and appropriate investigations should be used to rule these out.
Treatment
Treatment of Piles or Haemorrhoid
Medications i.e.
- If your hemorrhoids produce only mild discomfort, your doctor might suggest over-the-counter creams, ointments, suppositories or pads.
- These products contain ingredients such as witch hazel, or hydrocortisone and lidocaine, which can temporarily relieve pain and itching.
- Don’t use an over-the-counter steroid cream for more than a week unless directed by your doctor because it can thin your skin.
- Use topical treatments- Apply an over-the-counter Haemorrhoid cream or suppository containing hydrocortisone, or use pads containing witch hazel or a numbing agent.
- Soak regularly in a warm bath or sitz bath- Soak your anal area in plain warm water for 10 to 15 minutes two to three times a day. A sitz bath fits over the toilet.
- Take oral pain relievers- You can use acetaminophen (Tylenol, others), aspirin or ibuprofen (Advil, Motrin IB, others) temporarily to help relieve your discomfort.
External hemorrhoid thrombectomy i.e.
- If a painful blood clot (thrombosis) has formed within an external hemorrhoid, your doctor can remove the hemorrhoid, which can provide prompt relief.
- This procedure, done under local anesthesia, is most effective if done within 72 hours of developing a clot.
Minimally invasive procedures i.e.
Min For persistent bleeding or painful haemorrhoids, your doctor might recommend one of the other minimally invasive procedures available. These treatments can be done in your doctor’s office or other outpatient setting and don’t usually require anesthesia.
- Rubber band ligation
- Injection (sclerotherapy
- Coagulation (infrared, laser or two minds Surgical procedures.
Surgical procedures i.e.
Only a small percentage of people with haemorrhoids require surgery. However, if other procedures haven’t been successful or you have large haemorrhoids, your doctor might recommend one of the following:
- Haemorrhoid removal (hemorrhoidectomy)
- Haemorrhoid stapling.[4]
Prevention
Prevention
Key Prevention Strategies:
- Dietary Fiber:
- Aim for 25-35 grams of fiber daily from fruits, vegetables, and whole grains.
- Fiber softens stools and promotes regular bowel movements, reducing straining.
- Hydration:
- Drink 6-8 glasses of water and other liquids daily to keep stools soft.
- Avoid excessive alcohol and caffeine, which can contribute to dehydration.
- Regular Exercise:
- Aim for at least 30 minutes of moderate-intensity exercise most days.
- Exercise helps maintain bowel regularity and prevents constipation.
- Healthy Bowel Habits:
- Don’t delay bowel movements when the urge arises.
- Avoid straining or holding your breath during bowel movements.
- Weight Management:
- Maintain a healthy weight to reduce pressure on the veins in the pelvic and rectal area.
- Avoid Prolonged Sitting:
- Take breaks to move around and avoid sitting for extended periods, especially on the toilet. [11]
- Dietary Fiber:
Homeopathic Treatment
Homeopathic Treatment of Piles or Haemorrhoid
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Piles or Haemorrhoid:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Homoeopathic Approach:
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines are selected after a full individualizing examination and case-analysis, which includes the medical history of the patient, physical and mental constitution, family history, presenting symptoms, underlying pathology, possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) is also often taken into account for the treatment of chronic conditions. A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’.
The disease diagnosis is important but in homeopathy, the cause of disease is not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness are also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology is not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can be greatly improved with homeopathic medicines.
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications are also taken into account for selecting a remedy.
Medicines:
Aesculus [Aesc]
- This remedy is especially suitable to the form of hemorrhoids arising from portal congestion, abdominal plethora. They may or may not bleed, but there is a feeling in the rectum as of splinters or sticks.
- This remedy actually produced many liver symptoms and hemorrhoids in the provers. Other indicating symptoms are aching in the lumbar region, protruding purple piles with severe pains in the sacrum and small of the back and fullness in the region of the liver
- Dryness, burning and itching are good indications. Hughes prefers Nux vomica and Sulphur in hemorrhoids dependent on congestion of the portal system. Pulsatilla is one of the best remedies in hemorrhoids after Aesculus.
- Passive congestion and dyspeptic troubles are the keynotes; blind hemorrhoids. Hemorrhoids that bleed easily. It acts best in the higher potencies. Hemorrhoids from chronic constipation may cure with Aesculus. [2]
Aloes [Aloe]
- This is also a most useful hemorrhoidal remedy. It indicate where the piles protrude like a bunch of grapes, bleeding often and profusely, and greatly relieve by the application of cold water. There a very mark burning in the anus the bowels feel as if scraped.
- There is a tendency to diarrhoea, with the well-known uncertain feeling in the lower bowel. This tendency to diarrhoea will distinguish from Collinsonia, which has the tendency to constipation.
- Ratanhia has burning in the anus, and protrusion of varices after a hard stool. The characteristics of this remedy are burning and fissure of the anus, great painfulness and sensitiveness of rectum Capsicum.
- Bleeding piles with burning pain, itching, smarting and stinging in anus during stool are characteristic of Capsicum.[2]
Collinsonia [Coll]
- But says that no remedy can equal Collinsonia in obstinate cases of hemorrhoids, which bleed almost incessantly, he recommends the tincture.
- It is of special use in females with inertia of the rectum and a congestive tendency to the pelvic organs. It suits pregnant women who suffer from piles, and pruritus may be a marked symptom.
- The indicating symptoms are chiefly a sensation of sticks in the rectum, with constipation from inertia of the lower bowel.
- It is especially applicable to heart pains resulting from a suppression of a habitual hemorrhoidal flow. It is somewhat similar to Nux, but is a far more useful remedy. Ignatia. Hemorrhoids characterized by sharp, stitching pains, shooting up the rectum.
Hamamelis [Ham]
- Hughes esteems this remedy as one of the best in hemorrhoids, and clinical testimony is decidedly with him. It has bleeding hemorrhoids, and the flow of blood is quite copious, and the great characterizing indication is excessive soreness.
- Hughes recommends the second dilution, and experience shows that an external application either hot or cold of Hamamelis extract will promptly reduce the inflammation and soreness.
- Sulphur has constipation and itching about the anus, worse at night, which may consider as keynotes for its use.
Lycopodium [Lyc]
- A very useful remedy for piles which do not mature, but remain as hard bluish lumps, and also for bleeding piles containing large quantities of blood. Sepia.
- Hemorrhoids from irrational portal circulation; bleeding hemorrhoids with fullness in the rectum; oozing of moisture with great soreness.
Nux vomica [Nux-v]
- If the hemorrhoids large and blind, with a burning, stinging and constricted feeling in the rectum and a bruised pain in the small of the back, and especially if excited by sedentary habits or abuse of stimulants, the Nux may prescribe with confidence.
- Itching hemorrhoids keeping the sufferer awake at night, relieved by cold water, or bleeding piles with constant urging to stool, and a feeling as if the bowel would not empty itself, are further indications. Arsenicum. Indicated in bluish piles with burning pain, prostration and debility. Muriatic acid.
- Great sensitiveness of the anus, cannot make use of the softest toilet paper; the piles are so sore and sensitive that the slightest touch is unbreakable. Hemorrhoids in the old age people. Graphitis. Hemorrhoids which burn and sting, anus sore, worse sitting.
- The rectum seems to have lost its contractile power, and the varices protrude.
Sulphur [Sulph]
- This remedy corresponds to ailments producing hemorrhoids and to the troubles resulting from piles which have stopped bleeding, and as a result fullness in the head and uneasiness in the liver; constipation is present; a desire for stool and itching of the anus.
- Piles burn and fill up the rectum.
- Inflamed and very painful piles, scanty evacuation of faces in small, hard bits, like sheep’s dung, with pressing; frequent or copious urination. [2]
Diet & Regimen
Diet & Regimen of Piles or Haemorrhoid
Deep-fried and processed food items
- Avoid processed foods such as frozen meals, fast food and deep-fried food items, they are heavy and difficult to digest.
- They contain fewer nutrients, plenty of salt and unhealthy fats.
- All these contribute to poor digestion and constipation.
Spicy food
- Avoid spicy food.
Alcohol
- Do cut out on your alcohol intake.
- Alcohol not only disrupts the digestive balance by depleting few nutrients but also have a dehydrating effect on the gut.
Dairy products
- Dairy products many times leads to gas formation, cramps in the stomach, and constipation.
- Milk, cheese, and other dairy are more bothersome during an outbreak or flare-up of the disease.
- So, keep a track of your daily consumption of dairy products!
Unripe fruits
- Fruits serve as a savior when it comes to improving symptoms of piles.
- However, please check that you are consuming ripe fruit.
- Unripe fruits, like unripe bananas, may contain some constipating or irritating compounds which can increase the pain and suffering.
- Include ripe fruits as part of your midmeal routine.
Refined grains
- Refined grains like white rice, white bread and bagels, tempting cookies or cakes you buy at the stores have lost their bran component and are very low in fiber.
- Prefer whole grain over the refined forms.
High salted foods
- The high salt content in them can cause water retention and ultimately affect the blood vessels.
Iron supplements and some other medicines
- You may have been taking iron supplements before suffering from piles. But iron is a known constipating supplement.
- Also, some commonly used medicines come with unwanted effect of constipation.
- Never stop or alter doses abruptly. It is better to consult your doctor and let him decide the best regimen to address all your health concerns.
Excessive fiber
- Do not take fiber supplements despite every other person telling you to eat lots of fibers to relieve constipation.
- Fibers have bulk-forming action on stools, rather than sweeping action. So, they are useful in other types of constipation but not in piles.
- Regular optimal fiber intake is fine to keep your gut healthy.
Do’s and Don'ts
The Do’s & Don’ts:
Do’s
Increase Fiber Intake:
- Eat plenty of fruits, vegetables, and whole grains.
- Fiber helps soften stools and makes them easier to pass, reducing straining.
Stay Hydrated:
- Drink plenty of water throughout the day.
- Adequate hydration helps keep stools soft and prevents constipation.
Exercise Regularly:
- Aim for at least 30 minutes of moderate-intensity exercise most days.
- Exercise helps improve bowel function and prevents constipation.
Maintain Healthy Bowel Habits:
- Go to the bathroom as soon as you feel the urge.
- Avoid straining or holding your breath during bowel movements.
Maintain a Healthy Weight:
- Excess weight can put pressure on the veins in the pelvic and rectal area, increasing the risk of piles.
Practice Good Hygiene:
- Gently clean the anal area after bowel movements with moist wipes or toilet paper.
- Avoid harsh soaps or scrubbing.
Take Warm Baths:
Soaking in a warm bath for 10-15 minutes can help soothe discomfort and reduce inflammation.
Don’ts
Avoid Straining:
- Straining during bowel movements puts pressure on the veins in the rectal area, worsening piles.
Don’t Delay Bowel Movements:
- Ignoring the urge to go can lead to constipation and straining.
Avoid Prolonged Sitting:
- Sitting for long periods, especially on hard surfaces, can increase pressure on the rectal area.
Don’t Lift Heavy Objects:
- Heavy lifting can strain the muscles in the pelvic and rectal area.
Avoid Spicy and Processed Foods:
- Spicy and processed foods can irritate the digestive system and worsen pile symptoms.
Limit Alcohol and Caffeine:
- Alcohol and caffeine can dehydrate the body and contribute to constipation.
Don’t Use Harsh Soaps or Perfumed Products:
- These can irritate the sensitive skin around the anus.
Terminology
Terminology
Piles (Hemorrhoids):
- Meaning: Swollen and inflamed veins in the rectum and anus.
- Usage: "Piles, also known as hemorrhoids, are a common condition that affects millions of people worldwide."
Internal Hemorrhoids:
- Meaning: Hemorrhoids located inside the rectum. They are usually painless but may bleed.
- Usage: "Internal hemorrhoids are not usually visible or felt and rarely cause discomfort."
External Hemorrhoids:
- Meaning: Hemorrhoids located under the skin around the anus. They can be itchy, painful, and may bleed.
- Usage: "External hemorrhoids are usually painful and may cause bleeding during bowel movements."
Thrombosed Hemorrhoid:
- Meaning: A blood clot has formed within an external hemorrhoid, causing severe pain and swelling.
- Usage: "Thrombosed hemorrhoids are a medical emergency and require prompt treatment to relieve pain and prevent complications."
Prolapsed Hemorrhoid:
- Meaning: An internal hemorrhoid that has protruded outside the anus.
- Usage: "Prolapsed hemorrhoids can be uncomfortable and may require manual reduction or surgical intervention."
Bleeding:
- Meaning: Blood in the stool or on toilet paper after a bowel movement.
- Usage: "Bleeding is a common symptom of hemorrhoids and should be evaluated by a doctor."
Itching:
- Meaning: An uncomfortable sensation around the anus.
- Usage: "Itching is a common symptom of hemorrhoids, especially external hemorrhoids."
Pain:
- Meaning: Discomfort or soreness in the anal area.
- Usage: "Pain is a common symptom of hemorrhoids, particularly thrombosed or prolapsed hemorrhoids."
- Meaning: Infrequent or difficult bowel movements.
- Usage: "Constipation is a major risk factor for developing hemorrhoids as it leads to straining during bowel movements."
Straining:
- Meaning: Excessive force exerted during bowel movements.
- Usage: "Straining during bowel movements increases pressure on the veins in the rectum and anus, contributing to hemorrhoid development."
Fiber:
- Meaning: Indigestible plant material that helps soften stools and promote regular bowel movements.
- Usage: "Increasing fiber intake is an important preventive measure and treatment for hemorrhoids."
Sitz bath:
- Meaning: Soaking the anal area in warm water to relieve discomfort and promote healing.
- Usage: "Sitz baths are recommended for soothing hemorrhoid symptoms and promoting hygiene."
Banding:
- Meaning: A minimally invasive procedure that involves placing a rubber band around the base of a hemorrhoid to cut off its blood supply, causing it to shrink and fall off.
- Usage: "Banding is an effective treatment for internal hemorrhoids that cause bleeding or prolapse."
Sclerotherapy:
- Meaning: Injecting a chemical solution into a hemorrhoid to shrink it.
- Usage: "Sclerotherapy is another minimally invasive option for treating hemorrhoids."
These are just some of the common terminologies about piles. Understanding these terms can help you better comprehend information about this condition and make informed decisions about its prevention and treatment.
References
References use for Article Piles or Haemorrhoid
- Harrisons_Principles_of_Internal_Medicine_19th_Edition-_2_Volume_Set
- Therapeutics from Zomeo Ultimate LAN
- Bailey_and_Love_s_Short_Practice_of_Surgery
- https://www.mayoclinic.org/diseases-conditions/hemorrhoids/diagnosis-treatment/drc-20360280.
- International Journal of Surgery (2016).
- Surgical Review (2020).
- Colorectal Disease (2021).
- Sleisenger and Fordtran’s Gastrointestinal and Liver Disease, 11th Edition, Mark Feldman, Lawrence S. Friedman, Lawrence J. Brandt, 2021 Elsevier.
- Schwartz’s Principles of Surgery, 11th Edition, F. Charles Brunicardi, et al., 2018, McGraw Hill Professional.
- Sabiston Textbook of Surgery, 20th Edition, C Townsend, 2016, Elsevier.
- Mayo Clinic on Digestive Health (3rd Edition), Sahil Khanna (Editor), et al., 2019, Mayo Clinic Press.
Also Search As
Piles Also Search As
1. Online Search Engines:
Use search terms like:
- "homeopathy for piles"
- "homeopathic treatment for hemorrhoids"
- "homeopathic remedies for piles"
- "best homeopathic medicine for piles"
Specify the type of piles or symptoms if needed:
- "homeopathy for bleeding piles"
- "homeopathy for painful piles"
- "homeopathy for prolapsed hemorrhoids"
2. Homeopathic Websites and Blogs:
- Visit websites of reputable homeopathic organizations or practitioners.
- Look for their blogs or articles section.
- Search within those sites using similar keywords as mentioned above.
3. Online Homeopathic Forums and Communities:
- Join online forums or communities dedicated to homeopathy.
- Search within those forums or ask questions directly to the community.
4. Homeopathic Books and Journals:
- Visit libraries or bookstores with sections on alternative medicine or homeopathy.
- Browse through books and journals related to homeopathic treatment of piles.
5. Consult a Homeopathic Practitioner:
- The most reliable way to get personalized information is to consult a qualified homeopathic practitioner.
- They can recommend specific articles or resources based on your individual case and symptoms.
Tips:
- Look for articles from credible sources like homeopathic organizations, practitioners, or peer-reviewed journals.
- Pay attention to the author’s credentials and experience.
- Consider the date of publication to ensure the information is up-to-date.
- If you have specific questions or concerns, consult a qualified homeopathic practitioner for personalized advice.
Frequently Asked Questions (FAQ)
What is Piles?
Definition
Piles or Haemorrhoid are swollen blood vessels in the lower rectum. Hemorrhoids, also spelled hemorrhoids, are vascular structures in the anal canal.
What causes Piles?
Causes
- Portal hypertension and varicose veins
- Infection
- Diet and stool consistency
- Anal hypertonia
- Ageing
How are piles treated?
Treatment options depend on the severity of the piles.
- Mild cases: Lifestyle changes like increasing fiber intake, drinking more water, and exercising regularly may be sufficient.
- Moderate cases: Over-the-counter medications, creams, or suppositories can help relieve symptoms.
- Severe cases: Medical procedures like rubber band ligation, sclerotherapy, or surgery may be necessary.
How are piles diagnosed?
A doctor can usually diagnose piles through a physical examination and a digital rectal exam. In some cases, they may recommend additional tests like a colonoscopy or sigmoidoscopy.
Can homeopathy cure piles?
Homeopathy aims to stimulate the body’s healing response to address the underlying causes of piles, potentially leading to long-term relief.
What are the symptoms of Piles?
- Painful
- Pain typically resolves in two to three days
- Swelling
- Mucous discharge
- Perianal mass if they prolapse through the anus
- Itchiness
- Fecal incontinence
Homeopathic Medicines used by Homeopathic Doctors in treatment of Piles?
Homoeopathic Medicines For Piles
- Aesculus
- Aloes
- Collinsonia
- Hamamelis
- Lycopodium
- Nux vomica
