Post Traumatic Stress Disorder
Definition
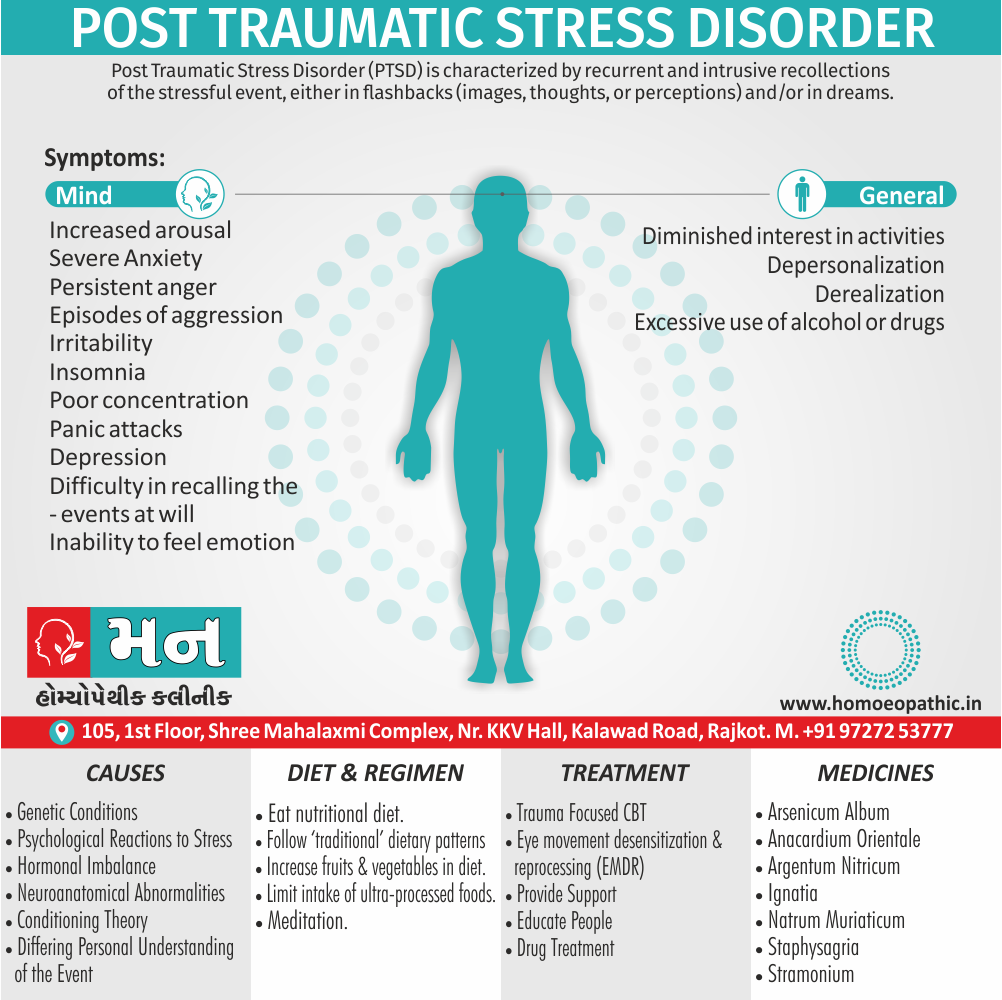
Post Traumatic Stress Disorder (PTSD) is characterised by recurrent and intrusive recollections of the stressful event, either in flashbacks (images, thoughts, or perceptions) and/or in dreams. [2]
There are a few options for synonyms of Post Traumatic Stress Disorder (PTSD), but it’s important to consider the context when choosing one:
Similar conditions:
- Battle fatigue: This term is historically used for PTSD in combat veterans.
- Delayed stress disorder: This emphasizes the delayed onset of symptoms after the trauma.
- Shell shock: This is an older term, primarily used for WWI soldiers experiencing PTSD.
Informal terms:
- Trauma: This is a general term for the event itself, not the mental health condition.
Acronyms:
- PTSD: This is the most common and accepted abbreviation.
- PTSS: Less common than PTSD, but still acceptable.
Important points:
- While some synonyms capture specific aspects of PTSD, they may not fully encompass the entire disorder.
- In most contexts, "PTSD" itself is the most accurate and respectful term.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Post-Traumatic Stress Disorder
According to ICD-10, this disorder arises as a delayed and/protracted response to an exceptionally stressful or catastrophic life event or situation, which is likely to cause pervasive distress in ‘almost any person’ (e.g. disasters, war, rape or torture, serious accident).
The symptoms of Post Traumatic Stress Disorder (PTSD) may develop, after a period of latency, within six months after the stress or may be delayed beyond this period.
There is an associated sense of re-experiencing of the stressful event. There is mark avoidance of the events or situations that arouse recollections of the stressful event, along with marked symptoms of anxiety and increased arousal. [2]
A variety of terms have used to describe what we now call PTSD, including railway spine, stress syndrome, shell shock, battle fatigue, and traumatic war neurosis.
It is now recognized that PTSD is a relatively common disorder, with US citizens having a lifetime risk of developing the condition of 8 percent.
Effective treatments are available for PTSD, so it is an important condition to screen high-risk patients for, especially those who are being treated for physical injuries/diseases relating to the trauma. [1]
Epidemiology
Epidemiology of Post-Traumatic Stress Disorder
Indian epidemiology then other
The US National Comorbidity Study found that 50 to 60 percent of individuals experience at least one traumatic event (fitting DSM-IV criteria) in their lifetime.
The most commonly experienced traumatic events are sudden death of a loved one, witnessing someone being killed or severely injured, accidents, and being involved in a fire.
However, most of those affected by traumatic events do not develop PTSD.
After a traumatic event of any type, the risk of developing PTSD is 8 percent for men and 20 percent for women.
The prevalence and incidence of PTSD vary markedly depending upon the geographical area studied.
Socioeconomic conditions, natural disasters, wars, and violence are not equally distributed across the world, and most of the current epidemiological figures relate to economically more developed countries.
In the USA, 7.8 percent of the population will suffer PTSD at some point in their lives, but the risk is twice as great for women (10 percent) as for men (5 percent). [1]
Causes
Causes of Post-Traumatic Stress Disorder
The necessary cause of post-traumatic stress disorder is an exceptionally stressful event in which the person was involved directly or as a witness.
Post Traumatic Stress Disorder (PTSD) is more common among those involved most directly in the stressful events, but the variation in response is not accounted for solely by the degree of personal involvement.
Predisposing factors:
1. Genetics i.e.:
Twin studies have shown a higher concordance of PTSD amongst monozygotic than dizygotic twins.
2. Physiological reactions to stress i.e.:
Patients with PTSD appear to have greater physiological reactions to stressors than people without PTSD who experienced the same traumatic event.
When stressed, patients show enhanced secretion of epinephrine and corticotropin secreting hormone, although levels of cortisol are lower than usual.
It seems that whilst the HPA axis is strongly stimulated, some abnormality occurs which enhances negative feedback. This may be an adaptation to reset the system in order to be able to respond quickly and strongly to new stressors.
Neurotransmitters also seem to be deregulated; the adrenergic activity of the sympathetic nervous system is increased, whilst levels and activity of serotonin (5HT) are decreased.
The fact that yohimbine (an alpha-receptor antagonist) provokes flashbacks whilst SSRIs decrease symptoms gives weight to this theory.
3. Neuroanatomical abnormalities i.e.:
MRI studies have shown that adults with PTSD have a smaller hippocampus than the general population.
Functional MRI has demonstrated that people with PTSD tend to show a heightened response to stress in the amygdala, hippocampus, and medial prefrontal cortex.
Maintaining factors:
1. Conditioning theory i.e.:
- This theory suggests that the continued symptoms of PTSD are due to classical conditioning.
- When a traumatic event occurs (an unconditioned stimulus), people respond with fear (unconditioned response).
- As reminders of the trauma occur (conditioned stimulus), people then respond with fear reactions (conditioned response).
- Frequently, the variety of stimuli widens, thereby increasing the symptom load.
- Avoidance of stimuli reinforces the conditioning, as it leads to reduced discomfort in the absence of a stimulus.
2. Differing personal understanding of the event i.e.:
- People have widely different views as to why the same event occurred, or what the future holds because of it.
- Some individuals will shake off a traumatic experience as a one of terrible event and move on. They tend to recover quickly.
- Patients with PTSD tend to have much more negative cognitions, often generalizing beyond the original event.
- Common examples are that the person starts to believe they were responsible for the accident that happened, or that nowhere is safe after being sexually assaulted.
- These negative cognitions reinforce themselves, similarly to those in patients with depression.
3. Stimuli triggering memories of the event i.e.:
- In a similar vein to the above, those patients who repeatedly come into contact with memories of the traumatic event tend to have symptoms for longer than those who do not.
- A good example of this is someone whose route to work passes the spot where a terrible car accident occurred.
4. Behaviours that maintain symptoms i.e.:
- Avoidance tends to stop people integrating the facts of the stressful experience into their memory, so that they continue to be fearful of the symptoms and what happened.
- Safety behaviours (e.g. constantly checking the gas hob is off after a fire) prevent a return to normality, and cause an increase in PTSD symptoms.
- Maladaptive coping strategies tend to increase the feelings of numbness and separation from the event, and do not help the person to acknowledge what has happened and continue with their life. [1]
Types
Types of Post-Traumatic Stress Disorder
PTSD can manifest in different ways, and recognizing the specific type can aid in understanding and seeking appropriate treatment. Here are some recognized types of PTSD:
Acute PTSD:
This type occurs within the first three months after a traumatic event. Symptoms may include re-experiencing the trauma, avoidance, and hyperarousal.
Chronic PTSD:
When symptoms persist beyond three months, it’s classified as chronic PTSD. This type may require long-term treatment and management.
Delayed-onset PTSD:
In some cases, symptoms may not appear until months or even years after the traumatic event. This can make diagnosis and treatment more challenging.
Complex PTSD:
This type often arises from prolonged or repeated trauma, such as childhood abuse or combat experiences. Symptoms can include difficulties regulating emotions, disturbed relationships, and negative self-perception.
This seminal work explores the impact of trauma on individuals and communities, offering insights into the complexities of PTSD and its various manifestations. It’s a valuable resource for anyone seeking a deeper understanding of this condition.
Remember: If you or someone you know is struggling with symptoms of PTSD, it’s crucial to seek professional help. A qualified mental health professional can provide an accurate diagnosis and guide you towards appropriate treatment options.[4]
Risk Factors
Risk Factors
Biological:
- Females
- Age: Children and Older adults are particularly vulnerable
- Ethnic marginalized groups
- Family or personal psychiatric disorder
- Low intelligence
Psychological:
- Childhood abuse
- Low self-esteem
- Exposure to previous trauma
Social:
- Lack of social support
- Difficult economic or legal circumstances [1]
Pathogenesis
Pathogenesis of Post-Traumatic Stress Disorder
PTSD is a complex disorder arising from exposure to traumatic events. Its pathogenesis involves a dynamic interplay of psychological, neurobiological, and environmental factors. While the exact mechanisms remain an area of ongoing research, here’s a breakdown of key elements:
Psychological Factors:
Fear Conditioning:
Traumatic experiences trigger intense fear responses. These responses can become conditioned, leading to heightened anxiety and avoidance even in safe situations.
Cognitive Appraisal:
How individuals perceive and interpret the traumatic event influences their vulnerability to PTSD. Negative appraisals, such as feeling helpless or blaming oneself, increase the risk.
Neurobiological Factors:
Stress Response:
The brain’s stress response systems, including the amygdala and hypothalamic-pituitary-adrenal (HPA) axis, become dysregulated in PTSD. This results in exaggerated fear responses and difficulty returning to baseline after stress.
Brain Structures:
Studies have shown alterations in brain regions like the hippocampus (memory) and prefrontal cortex (emotional regulation) in individuals with PTSD.
Environmental Factors:
Trauma Severity:
The severity and nature of the traumatic event play a role. Experiences involving intentional harm, such as assault or combat, carry a higher risk of PTSD.
Social Support:
Strong social support systems can buffer the impact of trauma and reduce the likelihood of developing PTSD.
This insightful book The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma delves into the complexities of trauma and its impact on the mind and body. It explores the neurobiological underpinnings of PTSD and offers a comprehensive understanding of its pathogenesis.
Remember:
- PTSD is a treatable condition. If you or someone you know is experiencing symptoms, seek professional help.
- Early intervention can significantly improve outcomes.[5]
Pathophysiology
Pathophysiology
The pathophysiology of PTSD involves a complex interplay of neurobiological and psychological processes that are triggered by exposure to a traumatic event. While research is ongoing, here’s a breakdown of key elements:
Neurobiological Factors:
Hyperarousal:
The autonomic nervous system becomes dysregulated, leading to heightened anxiety, hypervigilance, and exaggerated startle responses.Amygdala Hyperactivity:
The amygdala, responsible for fear and emotional processing, becomes hyperactive, leading to increased fear responses and difficulty extinguishing fear memories.Hippocampal Dysfunction:
The hippocampus, involved in memory formation and retrieval, may shrink, leading to difficulties consolidating memories and distinguishing between past and present threats.HPA Axis Dysregulation:
The hypothalamic-pituitary-adrenal (HPA) axis, responsible for stress response, becomes dysregulated, resulting in abnormal cortisol levels and impaired stress response.Neurotransmitter Imbalance:
Imbalances in neurotransmitters such as norepinephrine, serotonin, and dopamine contribute to mood dysregulation, anxiety, and hyperarousal.
Psychological Factors:
Fear Conditioning:
Traumatic experiences create strong associations between neutral stimuli and fear responses, leading to conditioned fear and avoidance behaviors.Cognitive Appraisals:
Negative interpretations of the traumatic event and its aftermath, such as self-blame or perceived helplessness, can increase the risk of PTSD.Memory Fragmentation:
Traumatic memories may become fragmented and disorganized, contributing to flashbacks and intrusive thoughts.Emotional Dysregulation:
Difficulty managing emotions, including anger, sadness, and guilt, is common in PTSD.
This book Why Zebras Don’t Get Ulcers: The Acclaimed Guide to Stress, Stress-Related Diseases, and Coping provides a comprehensive overview of the physiological and psychological effects of stress, including insights into the pathophysiology of PTSD.
Remember:
- PTSD is a treatable condition. If you or someone you know is experiencing symptoms, seek professional help.
- Early intervention can significantly improve outcomes.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Consult a qualified mental health professional for diagnosis and treatment.[6]
Clinical Features
Clinical Features
PTSD manifests with a constellation of symptoms that disrupt various aspects of a person’s life. These clinical features are typically grouped into four main categories:
1. Intrusion Symptoms:
- Flashbacks: Vivid, distressing re-experiences of the traumatic event, often accompanied by physical sensations and emotions.
- Nightmares: Disturbing dreams related to the trauma.
- Intrusive Thoughts: Unwanted and distressing memories, images, or thoughts about the traumatic event.
2. Avoidance Symptoms:
- Avoidance of Thoughts or Feelings: Deliberate attempts to avoid thinking about or discussing the trauma.
- Avoidance of People, Places, or Activities: Avoiding situations or stimuli that trigger memories of the trauma.
3. Negative Alterations in Cognition and Mood:
- Negative Beliefs About Oneself or the World: Feeling hopeless, helpless, or worthless.
- Persistent Negative Emotional State: Feeling numb, detached, or unable to experience positive emotions.
- Difficulty Remembering Key Aspects of the Trauma: Memory gaps or distorted memories of the event.
4. Alterations in Arousal and Reactivity:
- Irritability or Angry Outbursts: Feeling easily agitated or prone to anger.
- Reckless or Self-Destructive Behavior: Engaging in risky behaviors or substance abuse.
- Hypervigilance: Feeling constantly on edge or alert to potential threats.
- Difficulty Concentrating: Trouble focusing or completing tasks.
- Sleep Disturbances: Difficulty falling or staying asleep, or experiencing restless sleep.
The DSM-5 provides the official criteria for diagnosing mental disorders, including PTSD. It outlines the specific clinical features required for a diagnosis and helps mental health professionals assess and treat individuals with PTSD.
Remember:
- PTSD symptoms can vary in intensity and duration.
- If you or someone you know is experiencing these symptoms, seek professional help. Early intervention can lead to better outcomes.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Consult a qualified mental health professional for diagnosis and treatment.[7]
Sign & Symptoms
Sign & Symptoms of Post-Traumatic Stress Disorder
1. Increased arousal:
- Such as severe anxiety, irritability, insomnia, and poor concentration.
- There may be panic attacks and, occasionally, episodes of aggression.
- Anxiety increases further during flashbacks or reminders of the traumatic event.
2. Avoidance & ‘Dissociative’ symptoms:
- Such as difficulty in recalling the events at will, detachment, an inability to feel emotion (‘numbness’), and a diminished interest in activities.
- There is avoidance of reminders of the events and sometimes there is depersonalization and derealization.
3. Intrusions:
In this memories of the traumatic events appear suddenly as repeated intense imagery (‘flashbacks’), vivid memories, intrusive repetitive thoughts, or distressing dreams.
4. Depressive symptoms:
They are common, and survivors of a major disaster often feel guilt.
5. Maladaptive coping responses:
This include persistent anger (especially among those who believe they are innocent victims of others’ misbehaviour), excessive use of alcohol or drugs, and episodes of deliberate self-harm, some of which end in suicide.
Avoidance of reminders of the stressful events.
Maladaptive coping strategies. [1]
Post-traumatic stress disorder is diagnosed when symptoms last for 4 weeks or longer.
Clinical Examination
Clinical Examination
Accurate diagnosis of PTSD involves a comprehensive assessment conducted by a qualified mental health professional. This assessment typically includes the following components:
1. Detailed Clinical Interview:
- Thorough History: Gathering information about the individual’s trauma history, including the nature of the traumatic event(s), its severity, and its impact on their life.
- Symptom Assessment: Careful exploration of the individual’s current symptoms, using standardized questionnaires or structured interviews to identify and evaluate the presence and severity of PTSD symptoms.
- Mental Status Examination: Evaluating the individual’s overall mental state, including their mood, thought processes, and cognitive functioning.
- Comorbidity Assessment: Screening for other co-occurring mental health conditions, such as depression, anxiety disorders, or substance use disorders, which are often present alongside PTSD.
2. Physical Examination:
- While not always necessary, a physical examination may be conducted to rule out any medical conditions that could contribute to the individual’s symptoms or complicate treatment.
3. Psychological Testing:
- In some cases, psychological tests may be used to further assess cognitive functioning, emotional regulation, or personality traits that may be relevant to PTSD.
This comprehensive textbook Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry provides a detailed overview of psychiatric disorders, including PTSD. It covers diagnostic criteria, clinical features, and assessment procedures relevant to PTSD.
Remember:
- Accurate diagnosis is essential for effective treatment of PTSD.
- If you suspect you or someone you know may have PTSD, seeking professional help is crucial.
- Early intervention can significantly improve outcomes.
Disclaimer: This information is for education purpose cannot provide medical advice. Please consult with a qualified mental health professional for diagnosis and treatment of PTSD or any other mental health condition.[8]
Diagnosis
Diagnosis
Accurate diagnosis of PTSD is crucial for ensuring appropriate treatment and support. The diagnostic process typically involves the following steps:
Comprehensive Clinical Assessment:
A qualified mental health professional will conduct a thorough assessment, which may include:
- Detailed Interview: Gathering information about the individual’s trauma history, current symptoms, and impact on their life.
- Symptom Checklist: Using standardized questionnaires or structured interviews to assess the presence and severity of PTSD symptoms.
- Mental Status Examination: Evaluating the individual’s overall mental state, including mood, thought processes, and cognitive function.
- Comorbidity Assessment: Screening for co-occurring mental health conditions that may complicate the presentation or treatment of PTSD.
Diagnostic Criteria:
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) provides the official criteria for diagnosing PTSD. These criteria include:
- Exposure to a traumatic event: Experiencing, witnessing, or learning about an actual or threatened death, serious injury, or sexual violence.
- Presence of intrusion symptoms: Re-experiencing the trauma through flashbacks, nightmares, or intrusive thoughts.
- Persistent avoidance: Avoiding reminders of the trauma, including thoughts, feelings, people, places, or activities.
- Negative alterations in cognition and mood: Experiencing negative beliefs about oneself or the world, persistent negative emotional state, or difficulty remembering aspects of the trauma.
- Alterations in arousal and reactivity: Experiencing hypervigilance, irritability, angry outbursts, reckless behavior, difficulty concentrating, or sleep disturbances.
- Duration of symptoms: Symptoms must persist for more than one month.
- Significant distress or impairment: The symptoms must cause significant distress or impairment in social, occupational, or other important areas of functioning.
The DSM-5 is the authoritative reference for diagnosing mental disorders, including PTSD. It provides clear diagnostic criteria and guidelines for mental health professionals.
Remember:
- Accurate diagnosis of PTSD requires a comprehensive assessment by a qualified mental health professional.
- Self-diagnosis is strongly discouraged.
- If you suspect you or someone you know may have PTSD, seeking professional help is crucial.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Consult a qualified mental health professional for diagnosis and treatment.[7]
Differential Diagnosis
Differential Diagnosis
Accurate diagnosis of PTSD is crucial for effective treatment, but it can be challenging due to overlapping symptoms with other mental health conditions. Here are some key differential diagnoses to consider:
Acute Stress Disorder (ASD):
- Similar to PTSD, but symptoms occur within the first month after a traumatic event.
- If symptoms persist beyond one month, a diagnosis may shift to PTSD.
Adjustment Disorder:
- Involves emotional or behavioral symptoms in response to a stressful event, but the stressor may not be as severe as in PTSD.
- Symptoms typically resolve within six months of the stressor ending.
Major Depressive Disorder (MDD):
- Shares symptoms like sadness, loss of interest, and sleep disturbances with PTSD.
- However, MDD lacks the specific trauma-related symptoms of PTSD, such as flashbacks and avoidance.
Generalized Anxiety Disorder (GAD):
- Involves excessive worry and anxiety about various aspects of life.
- While PTSD can include anxiety symptoms, they are specifically linked to the traumatic event.
Panic Disorder:
- Characterized by recurrent panic attacks and fear of future attacks.
- While panic attacks can occur in PTSD, they are typically triggered by reminders of the trauma.
Substance Use Disorders:
- Individuals with PTSD may turn to substances to cope with their symptoms.
- Careful assessment is needed to determine whether substance use is a primary problem or secondary to PTSD.
Traumatic Brain Injury (TBI):
- If the trauma involved a head injury, TBI may be present alongside PTSD.
- Symptoms like memory problems and difficulty concentrating can overlap, necessitating careful evaluation.
This comprehensive textbook Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry provides a thorough overview of psychiatric disorders, including detailed discussions on differential diagnosis for PTSD and other related conditions.
Remember:
- Accurate diagnosis of PTSD requires a careful evaluation by a qualified mental health professional.
- If you are concerned about PTSD or any other mental health condition, seek professional help.[8]
Complications
Complications
Untreated or poorly managed PTSD can lead to a range of serious complications that affect various aspects of an individual’s life. These complications can include:
Physical Health Complications:
- Chronic Pain: PTSD is associated with increased risk of chronic pain conditions, such as headaches, back pain, and fibromyalgia.
- Cardiovascular Disease: Studies have shown a link between PTSD and increased risk of heart disease, stroke, and high blood pressure.
- Gastrointestinal Problems: PTSD can contribute to digestive issues, such as irritable bowel syndrome (IBS) and ulcers.
- Weakened Immune System: Chronic stress from PTSD can weaken the immune system, making individuals more susceptible to infections and illnesses.
Mental Health Complications:
- Depression: Co-occurring depression is common in individuals with PTSD, leading to further emotional distress and difficulties functioning.
- Anxiety Disorders: PTSD often coexists with other anxiety disorders, such as panic disorder, generalized anxiety disorder, and social anxiety disorder.
- Substance Use Disorders: Individuals with PTSD may turn to alcohol or drugs to cope with their symptoms, leading to addiction and further complications.
- Suicidal Thoughts and Behaviors: PTSD increases the risk of suicidal ideation and attempts.
Social and Occupational Complications:
- Relationship Difficulties: PTSD can strain relationships due to emotional instability, irritability, and avoidance behaviors.
- Occupational Problems: Difficulty concentrating, memory problems, and emotional distress can lead to decreased work performance and job loss.
- Social Isolation: Avoiding social situations and feeling disconnected from others can lead to social isolation and loneliness.
This influential book Trauma and Recovery: The Aftermath of Violence – from Domestic Abuse to Political Terror explores the long-term consequences of trauma and highlights the potential complications of PTSD if left untreated.
Remember:
- Seeking professional help for PTSD is crucial in preventing and managing these complications.
- Early intervention and effective treatment can significantly improve quality of life and reduce the risk of long-term consequences.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Please consult with a qualified mental health professional for diagnosis and treatment of PTSD or any other mental health condition.[9]
Investigations
Investigation
Accurate assessment and diagnosis of PTSD require a comprehensive investigation conducted by a qualified mental health professional. This investigation typically involves several key components:
1. Detailed Clinical Interview:
- Trauma History: A thorough exploration of the individual’s exposure to traumatic events, including the nature, severity, and duration of the trauma.
- Symptom Assessment: Careful evaluation of the presence and severity of PTSD symptoms, often using standardized questionnaires or structured interviews, to identify patterns that align with the diagnostic criteria.
- Mental Status Examination: A comprehensive assessment of the individual’s current mental state, including mood, thought processes, cognitive function, and any signs of psychosis or dissociation.
- Medical and Psychiatric History: A review of the individual’s medical and psychiatric history to rule out other potential causes of the symptoms and identify any co-occurring conditions that may complicate treatment.
- Social and Occupational Functioning: An assessment of how the symptoms are affecting the individual’s relationships, work, and overall quality of life.
2. Physical Examination:
- While not always necessary, a physical examination may be performed to rule out any medical conditions that could contribute to the presenting symptoms or complicate treatment.
3. Psychological Testing:
- In some cases, psychological tests may be used to further assess cognitive function, emotional regulation, or personality traits that may be relevant to PTSD.
4. Collateral Information:
- Gathering information from family members, friends, or other relevant individuals can provide valuable insights into the individual’s functioning and the impact of their symptoms.
This comprehensive text Posttraumatic Stress Disorder: A Comprehensive Text provides a detailed overview of PTSD, including its assessment, diagnosis, and treatment. It offers valuable insights into the complexities of PTSD investigation and evidence-based approaches to its management.
Remember:
- Early and accurate diagnosis of PTSD is crucial for initiating effective treatment and improving outcomes.
- If you are concerned about PTSD, seeking professional help is essential.
Disclaimer: This information is for educational purposes only and should not be considered medical advice. Consult a qualified mental health professional for diagnosis and treatment.[10]
Treatment
Treatment
Assessment:
A full psychiatric history should be taken, including information from the patient, a third-party informant, primary care physician, and previous hospital notes.
Specific points to cover include:
- The nature and severity of the stressful event;
- Current symptoms, including duration and severity;
- Effect of symptoms upon life at home, work, school, etc.;
- The patient’s beliefs about the nature of their condition;
- Previous diagnoses of psychiatric conditions and treatments received for them;
- Family history of psychiatric conditions;
- Current medications (prescribed, illicit, over-the-counter, alcohol, caffeine, nicotine);
- Premorbid personality traits;
- Current social situation: accommodation, employment, finances.
General measures:
- Provide support (practical, emotional, social, self-help materials)
- Information and education about PTSD
- Help with associated guilt, grief, or anger
Encourage talking about the event to friends and family, and finding ways to understand what has happened.
This helps to integrate memories of the event with the rest of the person’s experience and to find a way for them to continue with their life.
Psychological treatments:
Watchful waiting (symptoms for less than 4 weeks).
For patients presenting with symptoms that are severe or have persisted for 3 months after the trauma, psychological therapy should be offered.
Occasionally, patients may have severe disabling symptoms soon after the event, and they should be offered psychological therapy too.
There are two main types of therapy that are effective at reducing the symptoms of Post Traumatic Stress Disorder (PTSD):
1. Trauma-focused CBT i.e.:
- CBT is the first-line choice, and should be offered to all patients with PTSD.
- Specialized CBT for PTSD includes both exposure and cognitive therapy.
- The exposure element involves helping the patient to remember and put together memories of the events, and to relive the stressor with an emphasis on discussing their thoughts and feelings during the process.
- In vivo exposure is also used, in which the patient gradually works up to confronting situations they had avoided because they reminded them of the trauma.
- Common examples include visiting the site of an attack, or driving again after an accident.
It is thought that exposure works in two ways i.e.:
- Getting the patient used to being in the situation again (habituation),
- Organizing their memories such that they can identify that intrusive re-experiences are recollections, and are not happening right now.
The therapist helps the person to challenge these beliefs and to change their behaviours surrounding them.
A completed course of CBT reduces symptoms to a clinically insignificant level in 60 percent of patients.
2. Eye movement desensitization and reprocessing (EMDR) i.e.:
- This is another specialize treatment that assists the patient to process memories of the traumatic event and feel more positive about it.
- The patient has told to track the therapist’s finger as they move it rapidly back and forth in front of them, which induces sadistic eye movements.
- During this process the patient is suppose to focus on a trauma-related image, and then afterwards to discuss the thoughts and emotions that surround it.
- This is repeat many times while focusing on different images.
Pharmacological therapies:
Drugs should not use as the first-line treatment, but should reserve for those patients who are unable to undertake therapy, fail to improve with therapy, or have comorbid depression.
Hypnotics i.e.:
- A short-term course of a hypnotic can give for insomnia, especially in the immediate aftermath of a traumatic event.
- A maximum of 3 weeks should prescribe due to the risks of tolerance and dependence.
- A good choice is a short-acting benzodiazepine (e.g. temazepam).
Antidepressants i.e.:
- Approximately 60 percent of patients will respond to an SSRI, although more than one may need to try to eliminate symptoms altogether.
- The first-line choice in the UK should an SSRI, and paroxetine has the greatest evidence base.
- Mirtazapine and amitriptyline can try if an SSRI is not successful, but they should initiate by a psychiatrist.
- The drug should continue for at least 12 months after symptoms resolve, then tapered slowly.
- If a patient does not respond to medication, check their compliance, increase the dose of the drug, or try another class.
- Occasionally, patients will need to add an atypical antipsychotic (e.g. olanzapine) to their antidepressant. [1]
Prevention
Prevention of Post-Traumatic Stress Disorder
While it’s not always possible to prevent PTSD entirely, several strategies can help reduce the risk of developing the disorder or mitigate its severity after a traumatic event. These strategies can be broadly categorized into:
1. Pre-Trauma Interventions:
- Resilience Building: Enhancing an individual’s overall resilience through stress management techniques, coping skills training, and fostering social support networks can help buffer the impact of future trauma.
- Preparedness Training: Specific training for individuals in high-risk professions, such as first responders or military personnel, can equip them with the skills and knowledge to navigate traumatic situations more effectively.
2. Post-Trauma Interventions:
- Early Intervention: Providing immediate support and psychological first aid after a traumatic event can help prevent the development of PTSD symptoms.
- Psychological Debriefing: Structured interventions that allow individuals to process their traumatic experiences in a safe and supportive environment can reduce the risk of PTSD.
- Cognitive Behavioral Therapy (CBT): CBT techniques can help individuals identify and challenge negative thoughts and beliefs related to the trauma, promoting healthier coping mechanisms.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is a specialized therapy that helps individuals process traumatic memories and reduce their emotional impact.
This workbook provides The PTSD Workbook: Simple, Effective Techniques for Overcoming Trauma and Post-Traumatic Stress Disorder practical tools and exercises based on evidence-based therapies to help individuals manage PTSD symptoms and promote recovery.
Remember:
- PTSD prevention is an ongoing process that requires a multi-faceted approach.
- Seeking professional help after a traumatic event is crucial for early intervention and reducing the risk of developing PTSD.
Disclaimer: I am an AI language model and cannot provide medical advice. Please consult with a qualified mental health professional for guidance on PTSD prevention and treatment.[11]
Homeopathic Treatment
Homoeopathic Treatment
Recommended medicines for Post Traumatic Stress Disorder (PTSD) are Natrum Muriaticum, Ignatia, and Kali Phosphoricum.
Natrum Muriaticum
acts well for PTSD when a person tends to dwell on past unpleasant memories. The person wants to isolate and is afraid of new relationships.
Ignatia, an excellent medicine for PTSD, is of great help when frustration and hopelessness accompany PTSD. Ignatia also works well when a person is quarrelsome and has many changes in mood.
Kali Phosphoricum
It is a well-indicated medicine for PTSD when night terrors accompany it. In such cases, patients have an aversion to meeting people and talking to them.
1. For PTSD with Flashbacks of Past Unpleasant Events:
Staphysagria and Nitric Acidum are considered as top-grade medicines in the treatment for PTSD when flashbacks of previous unpleasant events occur.
Staphysagria
acts well when a person keeps dwelling on past unpleasant incidents of rape or sexual abuse. The patient tends to throw or break things.
Nitricum Acidum
It is a very effective medicine for PTSD in cases where a person holds grudges also dwells on past horrifying incidents. In detail, Nitricum Acidum treats symptoms like violent anger and hatred for the people who have offended.
2. For PTSD Accompanied by Disturbed Sleep:
The most effective remedies for PTSD accompanied by disturbed sleep are Opium and Coffea.
Opium
acts well in cases of PTSD when a person is sleepy but is unable to sleep. The person develops a fear after the fright, which remains for a long time.
Coffea
works well in cases where there is sleeplessness with a continuous flow of ideas in the mind. Mental activity keeps a person awake and makes him restless.
3. For PTSD with Nightmares:
Excellent remedies for PTSD accompanied by nightmares are Arsenic Album and Staphysagria.
Arsenic Album
is a beneficial medicine for PTSD in cases where there are nightmares and restlessness. In such situations, the patient has dreams of dead persons, fire, and darkness.
Staphysagria
a well-selected medicine for PTSD, works well, especially in children. Usually, the child screams, wants everybody to go out and calls for the mother.
4. For PTSD with Delusions or Hallucinations:
Prominent remedies for PTSD along with delusions or hallucinations are Agaricus Muscarius and Hyoscyamus.
Agaricus Muscarius
is a well-indicated treatment for PTSD when the person is preoccupied with thoughts of death, graves, and dying.
Hyoscyamus
another effective remedy, acts well when a person talks to imaginary characters and also imagines he is in the wrong place.
5. For PTSD with Indifference:
Top remedies specifically for PTSD accompanied by indifference are Sepia and Aurum Metallicum.
Sepia
is very useful in persons who show an aversion to family, friends, company, also sympathy.
Aurum Metallicum
acts well while dealing with patients who have lost love. In such cases, patients tend to died by suicide, and imagine they are unfit for the world.
6. For PTSD when a Person Wants Solitude:
Natrum Muriaticum and Ignatia are excellent remedies for PTSD when a person wants to be alone.
Homeopathy can be of great help in depression.
Natrum Muriaticum
is of great help in cases of severe depression and feelings of isolation. In such situations, the person shuts down emotionally also closes off from others after the traumatic event.
Ignatia
is a well-chosen remedy especially for patients who want to be alone and cannot tolerate contradiction. Additionally, Other symptoms include indifference, excessive emotion, moodiness, and an aversion to any amusement.
7. For PTSD with Anger:
Top grade remedies for PTSD accompanied by anger are Chamomilla also Nux Vomica.
Chamomilla
works well in cases where the patient gets involved in disputes and quarrels without a valid reason. In detail, The patient also tends to dwell on past disagreeable occurrences and keeps on moaning.
Nux Vomica
Is a very effective medicine for PTSD when the patient is impatient when spoken to, spiteful, violent also angry without provocation.
8. For PTSD with Difficulty in Concentration:
Basically, Anacardium and Kali Phosphoricum are excellent remedies for PTSD for patients experiencing difficulty in concentration and memory. [3]
Diet & Regimen
Diet & Regimen
While therapy and medication are the primary treatments for PTSD, emerging research suggests that diet and lifestyle modifications can also play a supportive role in managing symptoms and promoting overall well-being.
Dietary Recommendations for PTSD:
- Anti-Inflammatory Diet: Emphasize whole foods, fruits, vegetables, nuts, seeds, and healthy fats like olive oil and fatty fish. These foods contain antioxidants and omega-3 fatty acids, which have anti-inflammatory properties that may help regulate the stress response and improve mood.
- Limit Processed Foods and Sugar: Processed foods and added sugar can contribute to inflammation and blood sugar fluctuations, which can worsen PTSD symptoms.
- Gut Health: Emerging research suggests a connection between gut health and mental health. Including probiotic-rich foods like yogurt, kefir, and sauerkraut or considering a probiotic supplement may be beneficial.
- Hydration: Adequate hydration is essential for overall health and cognitive function. Aim for at least 8 glasses of water per day.
Regimen Recommendations for PTSD:
- Regular Exercise: Exercise has been shown to reduce stress, improve mood, and promote better sleep. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Stress Management Techniques: Practices like mindfulness meditation, deep breathing exercises, and yoga can help manage stress and anxiety associated with PTSD.
- Quality Sleep: Prioritize good sleep hygiene by maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment.
- Social Support: Connecting with supportive friends, family, or support groups can provide emotional support and a sense of belonging.
While not specifically focused on PTSD, this book The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a Time offers valuable insights into the connection between brain function, lifestyle choices, and mental health. It provides practical tips on how to leverage diet, exercise, and other lifestyle factors to promote well-being and resilience.
Disclaimer:
- The recommendations above are general guidelines and should not replace personalized advice from a healthcare professional or registered dietitian.
- It’s essential to consult with a healthcare provider to develop a treatment plan tailored to your specific needs and any dietary restrictions.
Remember, a holistic approach that combines therapy, medication (if prescribed), and healthy lifestyle choices is crucial for managing PTSD and improving quality of life.[12]
Do’s and Don'ts
Do’s & Don’ts of Post-Traumatic Stress Disorder
Post-Traumatic Stress Disorder Do’s & Don’ts
Do’s:
- Seek Professional Help: If you’re experiencing symptoms of PTSD, don’t hesitate to seek help from a qualified mental health professional. They can provide a proper diagnosis and create a personalized treatment plan tailored to your needs.
- Practice Self-Care: Prioritize healthy lifestyle habits like regular exercise, balanced nutrition, and adequate sleep. These can help manage stress and improve overall well-being.
- Connect with Others: Engage in social activities and maintain relationships with supportive friends and family. Social connection can be a powerful buffer against PTSD symptoms.
- Engage in Relaxation Techniques: Practice relaxation techniques such as deep breathing exercises, meditation, or yoga to reduce anxiety and manage stress.
- Be Patient with Yourself: Recovery from PTSD takes time. Be kind to yourself and acknowledge that healing is a process with ups and downs.
- Educate Yourself about PTSD: Learning about PTSD can empower you to understand your symptoms and actively participate in your treatment.
Don’ts:
- Self-Isolate: Withdrawing from others can worsen feelings of loneliness and depression. Make an effort to connect with supportive people in your life.
- Self-Medicate: Avoid using drugs or alcohol to cope with PTSD symptoms. These substances can interfere with treatment and exacerbate symptoms in the long run.
- Ignore Your Symptoms: Ignoring or minimizing your symptoms will not make them go away. Addressing them early on can lead to more effective treatment and faster recovery.
- Push Yourself Too Hard: Recovery from PTSD is not a race. Pace yourself and avoid overexerting yourself physically or emotionally.
- Be Afraid to Ask for Help: Reaching out for support is a sign of strength, not weakness. Don’t hesitate to ask for help from friends, family, or mental health professionals when you need it.
Additional Tips:
- Consider Support Groups: Connecting with others who share similar experiences can be incredibly validating and helpful.
- Practice Mindfulness: Mindfulness techniques can help you stay grounded in the present moment and reduce the frequency and intensity of flashbacks.
- Engage in Creative Outlets: Expressing yourself through art, music, or writing can be a healthy way to process emotions and cope with stress.
Remember: PTSD is a treatable condition. With the right support and treatment, you can manage your symptoms and reclaim your life.
Disclaimer: This information is not a substitute for professional medical advice. Always seek the guidance of a qualified mental health professional for diagnosis and treatment.
Terminology
Terminology
Here are some key terminologies used in the context of Post Traumatic Stress Disorder (PTSD), along with their meanings:
Trauma:
This refers to the deeply distressing or disturbing experience that triggers PTSD. It can be a single event (like a car accident, assault, or natural disaster) or ongoing, prolonged experiences (like childhood abuse or combat).
Stressors:
While "trauma" refers to the event itself, "stressors" are specific aspects or triggers that remind the person of the trauma. These can be sights, sounds, smells, or even thoughts and feelings that bring back memories of the traumatic event.
Flashbacks:
These are vivid, intrusive, and involuntary re-experiencing of the traumatic event. It’s as if the person is reliving the trauma, often accompanied by intense emotions and physical sensations.
Nightmares:
Disturbing dreams related to the traumatic event. They can be very vivid and upsetting, often leading to sleep disturbances and insomnia.
Avoidance:
This is a key symptom of PTSD where individuals try to avoid anything that reminds them of the trauma. This can include places, people, activities, or even thoughts and feelings.
Hyperarousal:
This refers to a state of increased anxiety and alertness. People with PTSD may be easily startled, have trouble sleeping, and feel constantly on edge.
Emotional Numbing:
Feeling emotionally detached or disconnected from others and the world around them. It can involve difficulty experiencing positive emotions like joy or love.
Hypervigilance:
Being constantly on guard for danger, even in safe situations. This can manifest as scanning the environment for threats, difficulty relaxing, and an exaggerated startle response.
Intrusive Thoughts:
Unwanted and distressing thoughts, memories, or images of the trauma that pop into the person’s mind uncontrollably.
Dissociation:
Feeling disconnected from oneself, one’s body, or one’s surroundings. It can range from mild detachment to a complete sense of unreality.
Comorbidity:
This refers to the presence of other mental health conditions alongside PTSD. Common comorbidities include depression, anxiety disorders, and substance abuse.
Understanding these terms is crucial for recognizing and addressing PTSD. If you or someone you know is struggling with symptoms related to a traumatic experience, seeking professional help is essential.
While the core terminologies related to PTSD remain the same, homeopathic articles might use some additional or nuanced terms. Here are some key ones:
Constitutional Remedy:
This refers to a homeopathic remedy that matches the individual’s overall physical, mental, and emotional state, not just their PTSD symptoms. It aims to address the root cause of their susceptibility to developing PTSD.
Miasm:
In homeopathy, a miasm is a predisposition to certain patterns of illness, often passed down through generations. Some miasms are believed to make individuals more susceptible to PTSD after trauma.
Provings:
These are systematic studies in homeopathy where healthy volunteers take a substance and record their physical, mental, and emotional responses. This helps determine the symptom picture of a remedy.
Repertorization:
This is the process a homeopath uses to analyze the patient’s symptoms and match them to the most appropriate remedy using a homeopathic repertory (a comprehensive index of symptoms and corresponding remedies).
Aggravation:
In homeopathy, a temporary worsening of symptoms after taking a remedy is sometimes seen as a sign that the remedy is working and stimulating the body’s healing response.
Succussion:
This refers to the vigorous shaking of a homeopathic remedy during its preparation. It’s believed to potentize the remedy and enhance its effectiveness.
Potency:
This indicates the degree of dilution and succussion a remedy has undergone. Higher potencies are considered more diluted and are believed to act on a deeper level.
Vital Force:
This is a core concept in homeopathy referring to the body’s inherent healing energy. Homeopathy aims to stimulate the vital force to overcome illness.
Law of Similars:
The fundamental principle of homeopathy stating that "like cures like." A substance that causes symptoms in a healthy person can cure similar symptoms in a sick person.
Nosodes:
Homeopathic remedies prepared from disease products, such as tissues or secretions. In the context of PTSD, nosodes might be considered if the trauma originated from a specific disease.
It’s important to note that while homeopathy can be a complementary approach for managing PTSD symptoms, it’s crucial to seek professional help from a qualified mental health practitioner for diagnosis and treatment.
References
References
- Psychiatry, Fourth Edition – Oxford Medical Publications -SRG-by John Geddes, Jonathan Price, Rebecca McKnight / Ch 23.
- A Short Textbook of Psychiatry 7th edition by Niraj Ahuja / Ch 8.
- https://www.drhomeo.com/homeopathic-treatment/homeopathic-treatment-ptsd/
- Trauma and Recovery,Revised Edition
Writer: Judith Herman, M.D.
(1997),Publication: Basic Books - The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma
Edition: First Edition,Writer: Bessel van der Kolk M.D.(2014), Publication: Viking. - Why Zebras Don’t Get Ulcers: The Acclaimed Guide to Stress, Stress-Related Diseases, and Coping,Edition: Third Edition,Writer: Robert M. Sapolsky
(2004),Publication: Henry Holt and Company. - Diagnostic and Statistical Manual of Mental Disorders (DSM-5)
Edition: Fifth Edition
Writer: American Psychiatric Association
(2013),Publication: American Psychiatric Publishing. - Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry
Edition: 11th Edition
Writers: Benjamin J. Sadock, Virginia A. Sadock, Pedro Ruiz,(2014)
Publication: Wolters Kluwer - Trauma and Recovery: The Aftermath of Violence – from Domestic Abuse to Political Terror,Edition: Revised Edition
Writer: Judith Herman, M.D.
(1997),Publication: Basic Books - Posttraumatic Stress Disorder: A Comprehensive Text
Edition: Second Edition
Editors: Matthew J. Friedman, Terence M. Keane, Patricia A. Resick
(2007),Publication: Guilford Press - The PTSD Workbook: Simple, Effective Techniques for Overcoming Trauma and Post-Traumatic Stress Disorder
Edition: Second Edition
Writer: Mary Beth Williams, PhD, and Soili Poijula, PhD,(2016)
Publication: New Harbinger Publications. - The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a Time
Edition: First Edition
Writer: Alex Korb, PhD,(2015)
Publication: New Harbinger Publications
Also Search As
Also Search As
People can search for homeopathic articles on Post-Traumatic Stress Disorder (PTSD) using various online resources and strategies:
Online Search Engines:
Specific search terms:
Use precise phrases such as:
- "homeopathy for PTSD"
- "homeopathic treatment of PTSD"
- "homeopathic remedies for PTSD"
- "PTSD homeopathic case studies"
Include additional keywords:
Add terms like:
- "anxiety"
- "trauma"
- "flashbacks"
- "nightmares"
- specific homeopathic remedies (e.g., "Aconite for PTSD")
Homeopathic Websites and Databases:
National Center for Homeopathy (NCH):
The NCH website has a search function to find articles and resources.
Homeopathic Educational Services (HES):
HES offers a vast collection of homeopathic articles and books.
Homeopathy Plus:
This online resource features articles, research, and case studies related to homeopathy.
Social Media and Forums:
Homeopathic groups and pages:
Follow or join groups and pages on platforms like Facebook, Instagram, or Reddit that focus on homeopathy. They often share articles and discussions related to PTSD.
Homeopathic forums:
Participate in online forums where homeopaths and individuals interested in homeopathy discuss various health conditions, including PTSD.
Additional Tips:
Use quotation marks:
Enclose phrases in quotation marks to search for the exact wording, e.g., "homeopathic treatment for PTSD."
Use advanced search options:
Most search engines allow you to filter results by date, language, or file type (e.g., PDF).
Consult a homeopathic practitioner:
Ask your homeopath for recommendations on reliable sources of information or specific articles.
Visit a homeopathic library:
If available in your area, a homeopathic library can be a treasure trove of information.
Important Considerations:
Evaluate the source:
Ensure the information comes from reputable homeopathic organizations or practitioners.
Consult a professional:
Always consult with a qualified homeopath before self-treating any condition, especially PTSD.
Remember, finding reliable and informative articles on homeopathy and PTSD requires a combination of targeted search strategies and critical evaluation of sources.
There are several ways to search for information on Post-Traumatic Stress Disorder (PTSD):
Online Search Engines
Use specific keywords:
- "PTSD"
- "post-traumatic stress disorder"
- "trauma symptoms"
- "PTSD treatment"
- "PTSD causes"
Combine keywords for more specific results:
- "PTSD in veterans"
- "PTSD in children"
- "PTSD and anxiety"
- "PTSD therapy"
Reputable Websites and Organizations:
National Institute of Mental Health (NIMH):
https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd
Mayo Clinic:
https://www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967
U.S. Department of Veterans Affairs:
https://www.ptsd.va.gov/
National Center for PTSD:
https://www.ptsd.va.gov/
Academic Databases:
PubMed:
Search for peer-reviewed scientific articles on PTSD.
Google Scholar:
Find a wider range of academic resources, including articles, books, and theses.
Libraries:
Local libraries:
Your local library may have books, journals, and other resources on PTSD.
University libraries:
University libraries often offer access to extensive collections and specialized databases.
Social Media and Support Groups:
Online support groups:
Many online communities and forums provide a safe space for individuals with PTSD to connect and share experiences.
Social media pages and hashtags:
Follow relevant organizations and hashtags to stay updated on the latest research and resources.
Additional Tips:
Use quotation marks:
Enclose phrases in quotation marks to search for the exact wording, such as "PTSD treatment guidelines."
Use advanced search operators:
Utilize search operators like AND, OR, and NOT to refine your search results.
Consult with a mental health professional:
If you have concerns about PTSD, reach out to a qualified mental health professional for guidance and support.
Remember:
- It’s important to consult reputable sources for accurate and up-to-date information on PTSD.
- If you or someone you know is experiencing symptoms of PTSD, seeking professional help is crucial.
Frequently Asked Questions (FAQ)
Can homeopathy help with PTSD?
Homeopathy aims to support individuals with PTSD by addressing their unique symptoms and promoting overall well-being. It can be used alongside conventional therapies to enhance emotional and mental balance.
Is it safe to use homeopathy for PTSD?
Homeopathic remedies are generally considered safe and well-tolerated when prescribed by a qualified practitioner.
However, it’s essential to consult with a healthcare professional for proper diagnosis and management of PTSD.
What is Post Traumatic Stress Disorder?
Post Traumatic Stress Disorder (PTSD) is characterised by recurrent and intrusive recollections of the stressful event, either in flashbacks (images, thoughts, or perceptions) and/or in dreams.
What are the treatment options for PTSD?
Treatment
Psychotherapy: Therapy helps individuals process the trauma and develop coping skills. Common types include Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR).
Medication: Antidepressants and anti-anxiety medications can help manage PTSD symptoms.
What causes Post Traumatic Stress Disorder?
Genetics
Physiological reactions to stress
Neuroanatomical abnormalities
How does a homeopath choose the right remedy for PTSD?
A qualified homeopath will conduct a detailed case analysis, considering the traumatic event, the individual’s emotional and physical responses, and their overall health to select the most appropriate remedy.
What are the 5 symptoms of Post Traumatic Stress Disorder?
Symptoms
Increased arousal
Avoidance & ‘Dissociative’ symptoms
Intrusions
Depressive symptoms
Maladaptive coping responses
How long does it take to see improvement with homeopathy for PTSD?
The response to homeopathic treatment varies depending on the individual, the severity of symptoms, and the duration of PTSD. It’s important to be patient and consistent with treatment
Homeopathic Medicines used by Homeopathic Doctors in treatment of Post Traumatic Stress Disorder?
Homoeopathic Medicine For Post Traumatic Stress Disorder
Natrum Muriaticum
Ignatia
Kali Phosphoricum
Staphysagria
Nitricum Acidum
Opium
Coffea
