Shoulder pain
Definition
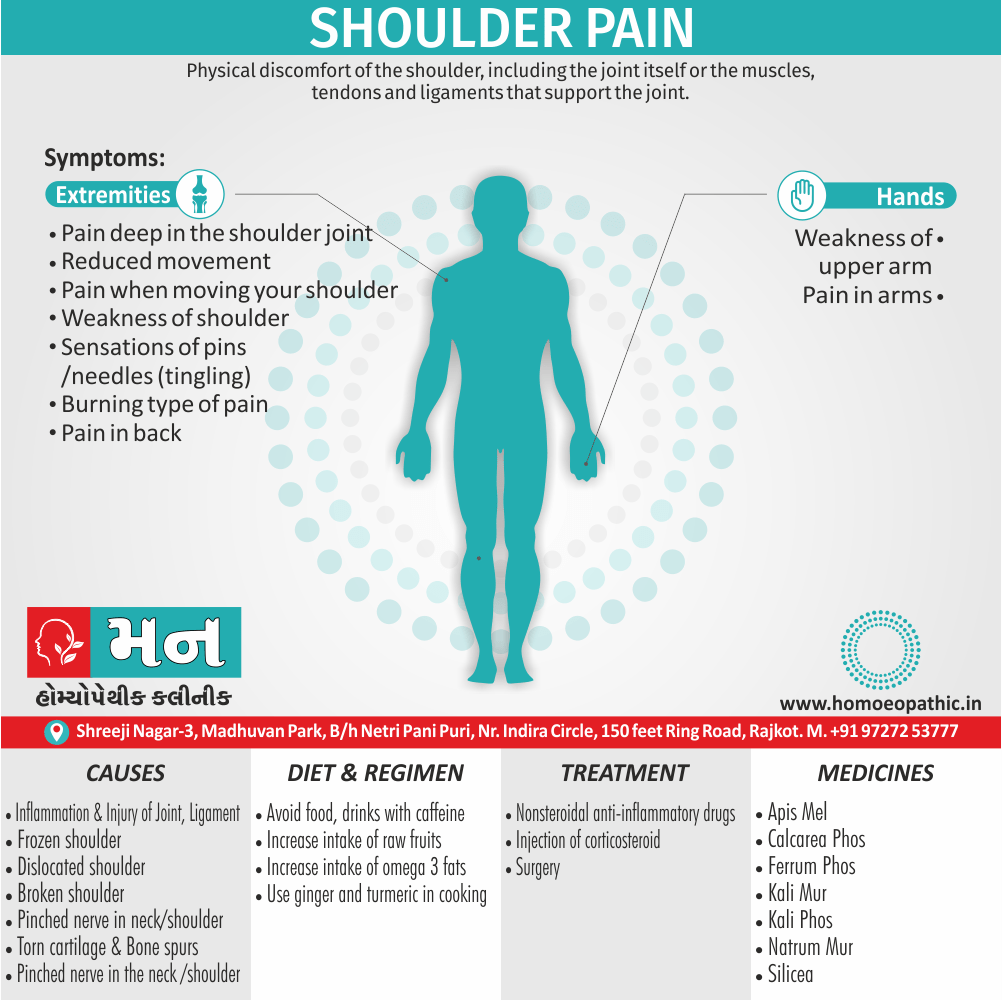
Shoulder pain is defined as Physical discomfort of the shoulder, including the joint itself or the muscles, tendons and ligaments that support the joint. [1]
Shoulder pain can be described using various synonyms, depending on the specific location, type, and intensity of the pain. Some common terms include:
General terms:
- Ache: A dull, persistent pain.
- Discomfort: A feeling of unease or pain.
- Soreness: A tender or painful feeling, often caused by overuse or injury.
- Stiffness: Difficulty moving the shoulder or a feeling of tightness.
More specific terms:
- Burning pain: A hot, stinging sensation in the shoulder.
- Radiating pain: Pain that spreads from the shoulder to other areas, such as the neck or arm.
- Sharp pain: A sudden, intense pain, often caused by a specific movement or injury.
- Throbbing pain: A pulsating or rhythmic pain.
Medical terms:
- Shoulder impingement: Pain caused by the compression of tendons or bursa in the shoulder joint.
- Rotator cuff tendinitis/tear: Inflammation or damage to the tendons that stabilize the shoulder joint.
- Frozen shoulder: A condition characterized by stiffness and pain in the shoulder joint.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Shoulder pain
During the evaluation of shoulder disorders, the examiner should carefully note any history of trauma, fibromyalgia, infection, inflammatory disease, occupational hazards, or previous cervical disease.[2]
Shoulder pain may originate in the Glenohumeral or acromioclavicular joints, sub acromial (subdeltoid) bursa, periarticular soft tissues (e.g., fibromyalgia, rotator cuff tear/tendinitis), or cervical spine. [2]
Epidemiology
Epidemiology :
The epidemiology of shoulder pain in India has been investigated in various studies, revealing the following insights:
One study found a prevalence of 22.9% among adults aged 30-70 years in Northern India (Bhawna, Multani, & Kundu, 2016). Another study reported a lifetime prevalence of up to 70% and highlighted an increasing incidence (Prevalence of shoulder disorders in tertiary care centre, no year provided).
Common Diagnoses:
- Periarthritis shoulder (adhesive capsulitis) and subacromial pain syndrome were identified as the two most common diagnoses in a tertiary care center (Prevalence of shoulder disorders in tertiary care centre, no year provided).
Risk Factors:
- Obesity, left-hand dominance, and diabetes were significantly associated with shoulder pain in one study (Bhawna et al., 2016). Other risk factors include diabetes mellitus, excessive overhead lifting, and trauma (Prevalence of shoulder disorders in tertiary care centre, no year provided).
Impact Shoulder pain
Impact Shoulder pain can significantly affect quality of life and contribute to disability. One study found a high prevalence (52.94%) of shoulder dysfunction in Indian patients with type II diabetes (Prevalence of shoulder dysfunction among Indian people with type II diabetes, 2015).[4][5]
Causes
Causes :
- Shoulder pain is referred frequently from the cervical spine but may also be referred from intrathoracic lesions (e.g., a Pancoast tumor) or from gallbladder, hepatic, or diaphragmatic disease. [2]
- Sub acromial bursitis is a frequent cause of shoulder pain. Whereas OA and RA commonly affect the acromioclavicular joint, OA seldom involves the Glenohumeral joint, unless there is a traumatic or occupational cause. [2]
- Rotator cuff tendinitis or tear is a very common cause of shoulder pain. Nearly 30 percent of the older people will have shoulder pain, with rotator cuff tendinitis or tear as the primary cause.
- Another common cause of shoulder pain is impingement syndrome where the rotator cuff gets caught between the acromion and humeral head
- Sometimes shoulder pain is the result of injury to another location in your body, usually the neck or biceps. This is known as referred pain. Referred pain generally doesn’t get worse when you move your shoulder. [2]
Other causes of shoulder pain include:
- Arthritis
- Torn cartilage
- Torn rotator cuff
- Swollen bursa sacs or tendons
- Bone spurs (bony projections that develop along the edges of bones)
- Pinched nerve in the neck or shoulder
- Broken shoulder or arm bone
- Frozen shoulder
- Dislocated shoulder
- Injury due to overuse or repetitive use
- Spinal cord injury
- Heart attack[1]
Types
Types :
- Rotator Cuff Tendinitis/Tear: The rotator cuff, a group of muscles and tendons stabilizing the shoulder joint, can become inflamed or tear due to overuse, injury, or age-related degeneration. This often results in pain and weakness, especially during overhead activities.
- Impingement Syndrome: This occurs when the tendons of the rotator cuff become compressed beneath the acromion (a bony prominence on the shoulder blade). This can lead to pain, particularly with overhead movements, and may progress to rotator cuff tears if left untreated.
- Frozen Shoulder (Adhesive Capsulitis): Characterized by stiffness and pain in the shoulder joint, frozen shoulder develops due to inflammation and thickening of the capsule surrounding the joint. This limits range of motion and can significantly impact daily activities.
- Bursitis: The bursae, fluid-filled sacs cushioning the shoulder joint, can become inflamed due to overuse or injury. This results in pain and tenderness, often exacerbated by movement.
- Osteoarthritis: Degenerative changes in the cartilage of the shoulder joint lead to osteoarthritis, causing pain, stiffness, and reduced range of motion. This is more common in older individuals or those with a history of shoulder injury.
- Referred Pain: Pain originating from other areas, such as the neck or cervical spine, can sometimes radiate to the shoulder. Identifying the underlying source of pain is crucial in such cases.[6]
Risk Factors
Risk Factors:
1. Age
As we get older, the risk of shoulder pain increases due to several factors. The cartilage in the shoulder joint can wear down with age, leading to conditions like osteoarthritis. Additionally, the tendons and muscles in the shoulder can become weaker and less flexible, making them more prone to injury.
2. Occupation
Certain occupations that involve repetitive overhead movements, heavy lifting, or prolonged sitting can increase the risk of shoulder pain. Jobs such as construction workers, painters, hairdressers, and office workers are particularly susceptible.
3. Sports and Activities
Participating in sports or activities that involve repetitive shoulder movements, such as swimming, tennis, baseball, and weightlifting, can put stress on the shoulder joint and increase the risk of injury.
4. Previous Injury
A history of previous shoulder injuries, such as dislocations, fractures, or rotator cuff tears, can increase the risk of developing chronic shoulder pain.
4. Previous Injury
A history of previous shoulder injuries, such as dislocations, fractures, or rotator cuff tears, can increase the risk of developing chronic shoulder pain.
5. Posture
Poor posture, especially rounded shoulders and a forward head position, can put strain on the muscles and tendons in the shoulder, leading to pain and discomfort.
6. Medical Conditions
Certain medical conditions, such as diabetes, rheumatoid arthritis, and heart disease, can increase the risk of developing shoulder pain.
Remember:
- Maintaining good posture
- Engaging in regular exercise
- Avoiding repetitive overhead movements
- Taking breaks from prolonged sitting
- Strengthening the muscles around the shoulder joint[6]
Pathogenesis
Pathogenesis :
Rotator Cuff Tendinopathy:
- The rotator cuff tendons are susceptible to degeneration and tears due to overuse, impingement, or age-related changes. This can lead to pain, weakness, and limited range of motion in the shoulder.
Subacromial Impingement Syndrome:
- This occurs when the rotator cuff tendons become compressed under the acromion (a bony prominence on the shoulder blade) during overhead activities. This can cause inflammation, pain, and limited shoulder function.
Adhesive Capsulitis (Frozen Shoulder):
- This condition involves inflammation and thickening of the shoulder joint capsule, leading to stiffness, pain, and restricted movement. The exact cause is unknown, but it is often associated with diabetes, thyroid disorders, or prolonged immobilization
Glenohumeral Joint Instability:
- This occurs when the head of the humerus (upper arm bone) slips out of the glenoid socket (shoulder socket) partially or completely. It can cause pain, a feeling of instability, and limited shoulder function.
Osteoarthritis:
- This degenerative joint disease involves the breakdown of cartilage in the shoulder joint, leading to pain, stiffness, and limited range of motion.[10][11][12]
Pathophysiology
Pathophysiology:
- Muscles: The rotator cuff, deltoid, and other shoulder girdle muscles play a crucial role in stabilizing the joint and facilitating movement. Muscle imbalances, weakness, or overuse can contribute to pain.
- Tendons: Tendons attach muscles to bones, and tendonitis (inflammation) or tears can be significant pain generators. The biceps tendon and rotator cuff tendons are particularly susceptible.
- Ligaments: Ligaments provide stability to the joint, and sprains or tears can lead to pain and instability.
- Bursae: Bursae are fluid-filled sacs that reduce friction between structures. Bursitis (inflammation) can cause pain and limit range of motion.
- Bones: Fractures, arthritis, or other bone abnormalities can also contribute to shoulder pain.
- Nerves: Nerves transmit signals to and from the shoulder, and nerve impingement or injury can cause pain, numbness, or weakness.[13]
Clinical Features
Clinical Features:
Shoulder Pain Clinical Features :
Shoulder pain presentations can vary widely depending on the underlying cause. Key clinical features to consider include:
- Location of Pain: Is the pain localized to a specific area of the shoulder, or does it radiate to the neck, arm, or back?
- Quality of Pain: Is the pain sharp, dull, aching, or burning?
- Onset and Duration: When did the pain start, and how long has it persisted?
- Aggravating and Relieving Factors: What activities or movements worsen or improve the pain?
- Associated Symptoms: Are there any other symptoms present, such as stiffness, weakness, numbness, or tingling? [11]
Sign & Symptoms
Sign & Symptoms
- Typically, there is pain and tenderness of the lower neck and suprascapular area, referred to the shoulder and upper limb area; shoulder movement may be restricted.
- Movement of the cervical spine and shoulder may reproduce more generalized upper back, neck, and shoulder pain.
- Upper limb paranesthesia may occur. [1]
Clinical Examination
Clinical Examination:
History
- Onset: Acute or insidious
- Duration:
- Pain characteristics: Location, quality, severity, radiation, aggravating and relieving factors
- Functional limitations: Activities of daily living, work, sports
- Previous injuries or treatments:
- Systemic symptoms: Fever, weight loss, rash
Observation
- Posture:
- Muscle wasting:
- Swelling:
- Deformity:
- Scars:
Palpation
- Bony landmarks: Sternoclavicular joint, acromioclavicular joint, coracoid process, greater tuberosity, bicipital groove
- Tenderness:
- Temperature:
- Muscle spasm:
Range of motion
- Active: Patient moves the shoulder on their own
- Passive: Examiner moves the shoulder for the patient
- Resisted: Patient moves the shoulder against resistance from the examiner
- Measure: Flexion, extension, abduction, adduction, internal rotation, external rotation
Special tests
- Impingement: Neer’s test, Hawkins-Kennedy test
- Rotator cuff: Empty can test, Drop arm test
- Instability: Apprehension test, Relocation test
- Biceps tendon: Speed’s test, Yergason’s test
- Acromioclavicular joint: Cross-body adduction test
- Neurological: Sensation, motor function, reflexes
Additional investigations
- Imaging: X-ray, MRI, ultrasound
- Other: Blood tests, nerve conduction studies[7]
Diagnosis
Diagnosis:
- During the evaluation of shoulder disorders, the examiner should carefully note any history of trauma, fibromyalgia, infection, inflammatory disease, occupational hazards, or previous cervical disease.
- In addition, the patient should questioned as to the activities or movement that elicit shoulder pain.
- Shoulder pain may originate in the Glenohumeral or acromioclavicular joints, sub acromial bursa, periarticular soft tissues or cervical spine.
- The shoulder should put through its full range of motion both actively and passively: forward flexion, extension, abduction, adduction, and internal and external rotation. Manual inspection of the periarticular structures will often provide important diagnostic information.
- Glenohumeral involvement best detect by placing the thumb over the Glenohumeral joint just medial and inferior to the coracoid process and applying pressure anteriorly while internally and externally rotating the humeral head. [2]
Differential Diagnosis
Differential Diagnosis:
Fractures:
- Clavicle
- Proximal humerus
- Scapula
Dislocations/Subluxations:
- Glenohumeral joint
- Acromioclavicular joint
- Sternoclavicular joint
Rotator Cuff Pathology:
- Tendinitis
- Tendinosis
- Partial tear
- Full-thickness tear
- Impingement syndrome
Labral Tears:
- Superior labrum anterior to posterior (SLAP)
Bankart
- Posterior labral tear
Biceps Tendon Pathology:
- Tendinitis
- Tendinosis
- Rupture
Adhesive Capsulitis (Frozen Shoulder)
Osteoarthritis:
- Glenohumeral joint
- Acromioclavicular joint
Rheumatoid Arthritis
Nerve-Related Conditions:
- Cervical radiculopathy
- Brachial plexus injury
- Suprascapular nerve entrapment
- Thoracic outlet syndrome[14]
Complications
Complications :
Frozen Shoulder (Adhesive Capsulitis):
- This condition involves the thickening and tightening of the shoulder capsule, leading to significant pain and restricted range of motion.
Rotator Cuff Tears:
- The rotator cuff is a group of muscles and tendons that stabilize the shoulder joint. Tears can occur due to injury or overuse, causing pain, weakness, and difficulty lifting the arm.
Tendinitis:
- Inflammation of the tendons in the shoulder can result from repetitive motions or overuse. This can cause pain, tenderness, and limited movement.
Bursitis:
- The bursae are small, fluid-filled sacs that cushion the shoulder joint. Inflammation of these sacs can cause pain, swelling, and difficulty moving the shoulder.
Osteoarthritis:
- This degenerative joint disease can affect the shoulder, leading to pain, stiffness, and limited range of motion.
Nerve Impingement:
- Compression of the nerves in the shoulder can cause pain, numbness, and weakness in the arm and hand.
Chronic Pain:
- Persistent shoulder pain can significantly impact daily activities, sleep, and overall well-being.
Limited Range of Motion:
- Shoulder pain and related complications can restrict the ability to move the arm freely, impacting activities such as dressing, reaching overhead, and participating in sports or hobbies.[11]
Investigations
Investigation:
- The examiner should apply direct manual pressure over the sub acromial bursa that lies lateral to and immediately beneath the acromion.
- Rotator cuff tendinitis suggest by pain on active abduction (but not passive abduction), pain over the lateral deltoid muscle, night pain, and evidence of the impingement signs (pain with overhead arm activities).
- The Near test for impingement perform by the examiner raising the patient’s arm into forced flexion while stabilizing and preventing rotation of the scapula. A positive sign is present if pain develops before 180° of forward flexion.
- The drop arm test is abnormal with supraspinatus pathology and demonstrate by passive abduction of the arm to 90° by the examiner. If the patient is unable to hold the arm up actively or unable to lower the arm slowly without dropping, the test is positive.
- Tendinitis or tear of the rotator cuff is best confirmed by magnetic resonance imaging (MRI) or ultrasound. [2]
Treatment
Treatment:
- Treatment will depend on the cause and severity of the shoulder pain. Additionally, Some treatment options include physical or occupational therapy, a sling or shoulder immobilizer, or surgery. [1]
- Your doctor may also prescribe medication such as nonsteroidal anti-inflammatory medications(NSAIDs) or corticosteroids.
- Moreover, Corticosteroids are powerful anti-inflammatory drugs that can be taken by mouth or your doctor can inject into your shoulder. [1]
- Some minor shoulder pain can be treated at home. In detail, Icing the shoulder for 15 to 20 minutes three or four times a day for several days can help reduce pain.
- Besides this, Use an ice bag or wrap ice in a towel because putting ice directly on your skin can cause frostbite and burn the skin.
- Resting the shoulder for several days before returning to normal activity and avoiding any movements that might cause pain can be helpful. In detail, Limit overhead work or activities.
- Other home treatments include using over-the-counter nonsteroidal anti-inflammatory medications to help reduce pain and inflammation also compressing the area with an elastic bandage to reduce swelling.[1]
- Simple shoulder exercises can help stretch and strengthen muscles and rotator cuff tendons. A either physical therapist or occupational therapist can show you how to do them properly.
- If you’ve had previous shoulder issues, use ice for 15 minutes after exercising to prevent future injuries.
- After having bursitis or tendinitis, performing simple range-of-motion exercises every day can keep you from getting frozen shoulder.[1]
- Nonsteroidal anti-inflammatory drugs (in other words; NSAIDs)
- Injection of an anti-inflammatory medicine called corticosteroid
- Physical therapy
- All in all, Surgery if all other treatments do not work. [1]
Prevention
Prevention:
Key Points for Shoulder Pain Prevention
While these books offer in-depth guidance, here are some essential takeaways for keeping your shoulders healthy:
- Maintain proper posture: Avoid slouching or hunching, as this can put unnecessary strain on your shoulders.
- Warm up before exercise: Before engaging in any physical activity, ensure your muscles are adequately warmed up to prevent injury.
- Use proper lifting techniques: When lifting heavy objects, use your legs and core muscles rather than your shoulders.
- Strengthen your shoulder muscles: Regular exercises that target the rotator cuff, deltoids, and trapezius can help improve stability and reduce the risk of pain.
- Stretch regularly: Stretching helps improve flexibility and range of motion, reducing the likelihood of muscle strain.
- Listen to your body: If you experience pain during or after exercise, stop and rest. Pushing through pain can worsen an injury.
- Seek professional guidance if needed: If you have persistent shoulder pain or concerns, consult a qualified healthcare professional for personalized advice and treatment.[15]
Homeopathic Treatment
Homeopathic Treatment of Shoulder pain
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Shoulder pain:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Belladonna–
- If you have Bursitis with a feeling of warmth and trembling, along with severe pain, you can take Belladonna.
- Sometimes the area becomes red and with swelling.
Arnica Montana–
- This treatment is beneficial when Bursitis is linked to severe trauma or discomfort.
- The affected region appears to be red and painful.
- If you have these symptoms, you may try to avoid any touch on the painful area.
Kalmia latifolia–
- If you have pain that begins in the upper joint (particularly the hip or shoulder) and moves down indicates that you need this remedy.
- Right shoulder bursitis is widespread and spreads to the elbow, wrist, or side.
- Pain and inflammation can come on all of a sudden, sometimes shifting.
- Discomfort is worse from motion, worse at night, and of a neuralgic kind.
Bryonia-
- When the pain generated by Bursitis or stiff tissue has a stitching or tear-like feel, this medication is a decent choice.
- You may feel that the area is inflamed.
Ferrum phosphoricum-
- This remedy can help relieve swelling, specifically in the right shoulder, which can cause pain that progresses to your wrist or even your neck.
- Here you may feel relief with gentle movement and cold massage.
Rhus tox-
- This homoeopathic medication works wonders in the treatment of joint pain.
- This medication eases both acute and chronic muscle pain.
- We use this remedy if there is any stiffness in your joints and a lot of discomforts.
- This homoeopathic remedy addresses a wide range of joint pains, from rheumatoid arthritis to overuse injuries damages.[4]
Calcarea Phos
- Shoulder-joint–Rheumatic pain in the arm near the shoulder-joint cannot lift the arm.
- Shooting and tearing from the shoulder-joint along the whole arm.
Diet & Regimen
Diet & Regimen
For Shoulder pain:
Diet:
Why it matters: Inflammation is often a key factor in shoulder pain, whether it’s from a recent injury or a chronic condition like arthritis. What you eat can either fuel or fight inflammation.
Focus on these:
Colorful fruits and veggies: These are loaded with antioxidants and phytonutrients that help protect your body from damage and reduce inflammation.
Examples: Berries (especially blueberries, raspberries, and strawberries), cherries, dark leafy greens (spinach, kale), and cruciferous vegetables (broccoli, cauliflower, Brussels sprouts).
Omega-3 fatty acids: These healthy fats have powerful anti-inflammatory effects.
Sources: Fatty fish (salmon, tuna, mackerel), flaxseeds, chia seeds, walnuts.
Spices: Certain spices have been shown to have anti-inflammatory properties.
Key ones: Turmeric (curcumin) and ginger. Add them to your cooking whenever possible.
Limit these:
Processed foods: Often high in unhealthy fats, added sugars, and sodium, which can promote inflammation and hinder healing.
Examples: Fast food, packaged snacks, processed meats.
Sugary drinks: Soda, sugary juices, and energy drinks contribute to inflammation and offer little nutritional value.
Excessive alcohol: Can interfere with healing and increase inflammation.
Regimen
Protection: Your shoulder needs a break to heal. Avoid any activities that cause pain. This might mean modifying your workouts, taking a break from certain sports, or even adjusting how you do everyday tasks.
Ice it down: Apply ice packs to the affected area for 15-20 minutes at a time, several times a day.
Compression: Gently wrap the area with an elastic bandage to provide support and help reduce swelling. Don’t wrap it too tightly, as this could restrict blood flow.
Elevate: Keep your shoulder raised above the level of your heart as much as possible. This helps reduce swelling by promoting fluid drainage. You can use pillows or a sling to help with elevation.
To promote healing and recovery:
Gentle movement: Once the initial sharp pain subsides, start moving your shoulder gently. This helps prevent stiffness, maintain range of motion, and improve blood flow to the area.
Some examples:
Pendulum exercises: Lean forward and let your arm hang down. Gently swing your arm forward and backward, side to side, and in circles.
Arm circles: Stand with your arms at your sides. Slowly make small circles with your arms, gradually increasing the size of the circles as your pain allows.
Wall slides: Stand facing a wall with your feet shoulder-width apart. Place your hands on the wall at shoulder height, fingers pointing upward. Slowly walk your fingers up the wall as high as you can comfortably reach, then slowly walk them back down.
Over-the-counter pain relief: Medications like ibuprofen (Advil, Motrin) or naproxen (Aleve) can help reduce pain and inflammation.
Important: Always follow the recommended dosage on the label and talk to your doctor or pharmacist if you have any concerns or medical conditions.
Heat therapy: After the initial acute phase (usually 48-72 hours), applying heat can help relax muscles, increase blood flow, and soothe the area.
Options: Use a warm compress, a heating pad on a low setting, or take a warm bath.
Important Reminders:
See a doctor: If your shoulder pain is severe, persistent, doesn’t improve with home care, or is accompanied by other symptoms (numbness, tingling, weakness), it’s important to seek medical attention. A healthcare professional can properly diagnose the cause of your pain and recommend the right treatment plan, which might include physical therapy, medications, or in some cases, surgery.
Listen to your body: Don’t push yourself too hard, especially in the early stages of healing. Gradually increase your activity level as your pain allows.
Individual needs: These are general recommendations. Your specific needs may vary depending on the cause of your shoulder pain and your overall health.
Do’s and Don'ts
Do’s & Don’ts
Shoulder Pain Do’s & Don’ts
Do’s:
- Maintain Good Posture: Pay attention to your posture throughout the day, especially when sitting or working at a desk. Slouching and hunching can strain your shoulders.
- Practice Proper Lifting Techniques: When lifting objects, use your legs and keep your back straight. Avoid lifting heavy objects above your head.
- Warm Up Before Exercise: Before engaging in any physical activity, perform warm-up exercises to prepare your shoulder muscles and joints.
- Stretch Regularly: Gentle stretching exercises can help improve shoulder flexibility and range of motion.
- Strengthen Your Shoulder Muscles: Targeted exercises can help strengthen the muscles surrounding your shoulder joint, providing better support and stability.
- Rest and Ice: If you experience shoulder pain, rest the affected area and apply ice packs for 15-20 minutes at a time to reduce inflammation.
- Seek Professional Help: If your pain persists or worsens, consult a healthcare professional for proper diagnosis and treatment.
Don’ts:
- Overexertion: Avoid activities that put excessive strain on your shoulder, such as heavy lifting, repetitive overhead movements, or contact sports.
- Ignoring pain: Don’t ignore persistent shoulder pain, as it could indicate a more serious underlying condition.
- Sleeping on the affected side: Avoid sleeping on the affected shoulder, as this can worsen pain and inflammation.
- Self-medicating: Don’t self-medicate with over-the-counter pain relievers without consulting your doctor, as they can have side effects and may interact with other medications.
- Delaying treatment: Don’t delay seeking professional help if your pain persists or worsens, as early intervention can lead to better outcomes.
Terminology
Terminology:
- Rotator Cuff: A group of four muscles and tendons that surround the shoulder joint, providing stability and allowing for a wide range of motion.
- Tendinitis: Inflammation of a tendon, often caused by overuse or repetitive strain.
- Bursitis: Inflammation of a bursa, a small fluid-filled sac that cushions and reduces friction between bones, tendons, and muscles near joints.
- Impingement Syndrome: A condition where the tendons of the rotator cuff become compressed or irritated as they pass beneath the acromion (the bony prominence at the top of the shoulder blade).
- Frozen Shoulder (Adhesive Capsulitis): A condition characterized by stiffness and pain in the shoulder joint, resulting in a limited range of motion.
- Labral Tear: A tear in the labrum, a ring of cartilage that surrounds the shoulder socket and helps stabilize the joint.
- Dislocation: When the head of the upper arm bone (humerus) pops out of the shoulder socket.
- Separation: An injury to the acromioclavicular (AC) joint, where the collarbone (clavicle) separates from the shoulder blade (scapula).
- Arthritis: Inflammation of a joint, leading to pain, stiffness, and swelling. Common types in the shoulder include osteoarthritis and rheumatoid arthritis.
- Fracture: A break in a bone, often caused by trauma or injury.
Other Terminology:
- Remedies: These are homeopathic medicines, usually derived from natural substances, that are used to treat various ailments, including shoulder pain. Examples include Arnica, Rhus tox, and Bryonia.
- Potency: This refers to the dilution and succussion (a specific shaking process) a remedy has undergone. Higher potencies are considered more diluted and are thought to have a deeper-acting effect.
- Constitutional remedy: This is a remedy chosen based on the individual’s overall physical and mental characteristics, not just their specific symptoms. It’s believed to address the root cause of the problem and promote long-term healing.
- Aggravation: A temporary worsening of symptoms after taking a remedy, often considered a positive sign that the remedy is working.
- Amelioration: An improvement or relief of symptoms.
- Modalities: Factors that make symptoms better or worse, such as time of day, weather, movement, or rest. These are important in choosing the right remedy.
- Materia medica: A reference book that lists the symptoms and characteristics associated with different homeopathic remedies.
- Repertory: A book that lists symptoms and the remedies that may be helpful for them. It’s used to find potential remedies based on the patient’s symptoms.
- Proving: A process where healthy individuals take a remedy and record their symptoms, helping to understand the remedy’s effects.
References
References
- https://www.healthline.com/health/chronic-pain/shoulder-pain
- Harrisons_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Sets
- A Complete Repertory of the Tissue Remedies of Schussler by S. F. Shanno https://aisclinic.in/homeopathy-treatment-and-medicine-for-shoulder-muscle-pain/
- Prevalence of shoulder disorders in tertiary care centre.
- Prevalence of shoulder dysfunction among Indian people with type II diabetes, 2015.
- "Essentials of Physical Medicine and Rehabilitation: Musculoskeletal Disorders, Pain, and Rehabilitation," 4th Edition, by Walter R. Frontera, et al. (2015).
- Reference: Magee, D. J. (2014). Orthopedic physical assessment (6th ed.). Elsevier Saunders.
- Reference: Kisner, C., & Colby, L. A. (2017). Therapeutic exercise: Foundations and techniques (8th ed.). F.A. Davis Company.
- Reference: Prentice, W. E. (2019). Rehabilitation techniques in sports medicine (6th ed.). McGraw Hill.
- Physical Rehabilitation, 7th Edition: 2019
- Kelley’s Textbook of Rheumatology: 10th Edition
2017 - DeLee & Drez’s : 5th Edition,2020.
- Neumann, D. A. (2017). Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation (3rd ed.). Mosby.
- Book: Dutton’s Orthopaedic Examination, Evaluation,and Intervention,5th Edition
"Treat Your Own Shoulder" by Jim Johnson, PT (4th Edition, 2018.
Also Search As
Also Searched As:
Online search engines
- Use specific keywords: Combine terms like "homeopathy," "shoulder pain," "remedies," and specific conditions like "frozen shoulder" or "rotator cuff injury."
- Try different search engines: Google, DuckDuckGo, Bing, and other search engines may yield different results.
- Refine your search: Use advanced search options to filter results by date, language, or file type.
Specialized homeopathic websites and databases
- Homeopathic organizations: Many organizations have websites with resources, including articles on various conditions.
- Online homeopathic journals: Search for peer-reviewed journals dedicated to homeopathy.
- Homeopathic libraries: Some libraries offer online access to homeopathic books and journals.
Social media and forums
- Homeopathy groups: Join online communities and forums to connect with others interested in homeopathy and share resources.
- Follow homeopathic practitioners: Many practitioners share information and articles on their social media pages.
There are several ways to search for information about snoring:
Online Search Engines
- Use general search terms: Start with simple searches like "snoring," "causes of snoring," or "snoring remedies."
- Be specific: If you have particular concerns, add specific keywords, like "snoring and sleep apnea," "snoring in children," or "natural remedies for snoring."
- Use medical websites: Look for reputable health websites like Mayo Clinic, WebMD, or Cleveland Clinic. They often have comprehensive articles on various health conditions, including snoring.
Online Health Forums and Communities
- Connect with others: Online forums and communities allow you to ask questions, share experiences, and learn from others who are dealing with snoring.
- Seek recommendations: You may find recommendations for treatments, products, or healthcare professionals who specialize in sleep disorders.
Medical Databases and Journals
- Access research articles: If you want in-depth information or the latest research on snoring, search medical databases like PubMed or Google Scholar.
- Consult medical journals: Look for articles in reputable medical journals that focus on sleep disorders or otolaryngology (ear, nose, and throat).
Consult a Healthcare Professional
- Get personalized advice: If you’re concerned about your snoring or suspect it might be related to a more serious condition like sleep apnea, consult a doctor or a sleep specialist. They can provide a diagnosis, recommend treatment options, and answer any questions you may have.
Remember, when searching for information online, it’s important to be critical of the sources you use. Look for information from reputable organizations and healthcare professionals, and always consult a doctor if you have concerns about your health.
Frequently Asked Questions (FAQ)
What is Shoulder pain?
It is defined as Physical discomfort of the shoulder, including the joint itself or the muscles, tendons and ligaments that support the joint.
What causes Shoulder pain?
- Intrathoracic lesions
- Sub acromial bursitis
- Rotator cuff either tendinitis or tear
- Impingement syndrome
- Arthritis
- Swollen either bursa sacs or tendons
- Bone spurs
- Pinched nerve in the neck or sh
Can I prevent shoulder pain?
Yes, you can take steps to reduce your risk. Maintain good posture, warm up before exercising, avoid overuse, and strengthen your shoulder muscles with regular exercises.
What are the symptoms of Shoulder pain?
- Pain and tenderness of the lower neck and suprascapular area, referred to the shoulder also upper limb area
- Shoulder movement may be restricted
- Movement of the cervical spine and shoulder may reproduce more generalized upper back, neck, also shoulder pain.
- Upper limb paranesthesia
Can homeopathy effectively treat shoulder pain?
Yes, homeopathy offers a holistic approach to treating shoulder pain by addressing the underlying cause and stimulating the body’s natural healing abilities. Many people find relief from various types of shoulder pain through homeopathic remedies.
What are the treatment options for shoulder pain?
Treatment depends on the underlying cause. Options may include rest, ice/heat therapy, over-the-counter pain relievers, physical therapy, corticosteroid injections, or in some cases, surgery.
How does a homeopath choose the right remedy for shoulder pain?
A qualified homeopath will conduct a detailed consultation to understand your unique symptoms, medical history, and overall health. This information helps them select the most appropriate remedy for your specific condition.
How long does it take to see results from homeopathic treatment for shoulder pain?
The response time to homeopathic treatment varies depending on the individual, the severity of the pain, and the underlying cause. Some people may experience relief quickly, while others may require more time.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Shoulder pain?
Homoeopathic Medicine For Shoulder Pain
- Belladonna
- Arnica Montana
- Kalmia latifolia
- Bryonia
- Ferrum phosphoricum
- Rhus tox
