Eating Disorder
Definition
There is a commonly held view that eating disorders are a lifestyle choice. Eating disorders are actually serious and often fatal illnesses that cause severe disturbances to a person’s eating behaviors. Obsessions with food, body weight, and shape may also signal an eating disorder.
- Clinical terms: anorexia nervosa, bulimia nervosa, pica, rumination disorder, ARFID (avoidant/restrictive food intake disorder)
- More general terms: disordered eating, unhealthy eating habits, abnormal eating patterns, psychological disorder
- Informal terms: food issues, unhealthy relationship with food
Frequently Asked Questions (FAQ)
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Eating Disorder
Obsessions with food, body weight, and shape may also signal an eating disorder.
The two specific diagnosis noted in the DSM-IV include anorexia nervosa, bulimia nervosa, and compulsive overeating disorder i.e.:
- Anorexia Nervosa
- Bulimia Nervosa
- Compulsive Overeating or Binge Eating Disorder
- Obesity (in other words, Overeating Associated with Other Psychological Disturbances)
- Psychogenic Vomiting
Epidemiology
Epidemiology of Eating Disorder
There is limited epidemiological data on eating disorders (EDs) in India, with most studies focusing on specific populations like adolescents or college students. Research suggests that the prevalence of EDs in India is lower than in Western countries, but it is still a significant concern.
Key Findings:
- A systematic review by Shah (2023) found that the prevalence of anorexia nervosa among Indian females ranged from 0.04% to 4.2%, while the prevalence of bulimia nervosa ranged from 0.2% to 2.6%.[7]
- A study by Vaidyanathan et al. (2019) estimated the prevalence of any ED to be 2.1% among Indian adolescents.[8]
- Several studies have reported a rising trend in the prevalence of EDs in India, particularly among young women in urban areas.
Important Considerations:
- Most studies have focused on anorexia and bulimia nervosa, with limited data on other EDs like binge eating disorder.
- There is a need for more representative, population-based studies to accurately estimate the prevalence of EDs in India.
- Cultural factors may influence the presentation and diagnosis of EDs in India, highlighting the need for culturally sensitive assessment tools.
Please note that these are just a few examples, and the actual prevalence of EDs in India may vary depending on the population studied and the methodology used. More research is needed to fully understand the epidemiology of EDs in India.
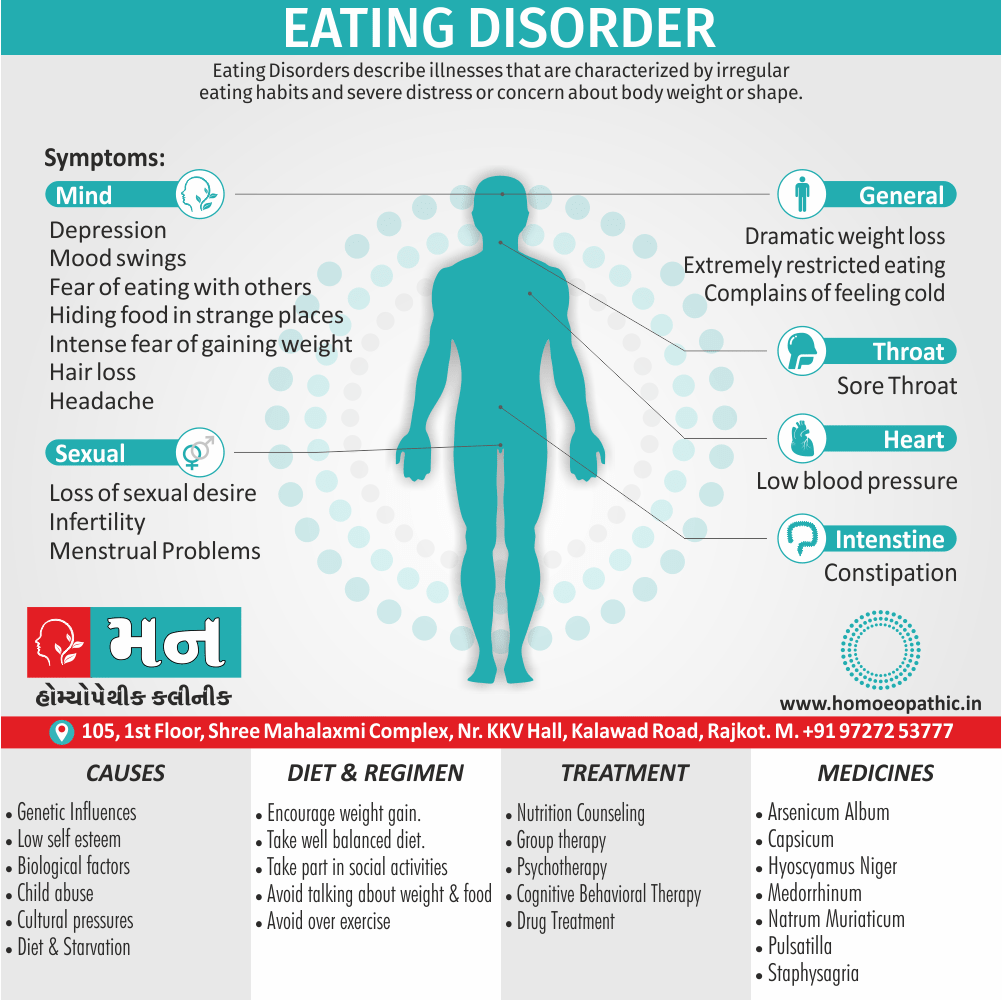
Causes
Causes of Eating Disorder
The exact cause of eating disorders is unknown. As with other mental illnesses, there may be many causes, such as:
- Genetics and biology: Certain people may have genes that increase their risk of developing eating disorders. Biological factors, such as changes in brain chemicals, may play a role in eating disorders.
- Psychological and emotional health: People with eating disorders may have psychological and emotional problems that contribute to the disorder. They may have low self-esteem, perfectionism, impulsive behavior and troubled relationships.
- Biological factors
- Child abuse
- Cultural pressures
- Diet & Starvation (3)
Types
Types of Eating Disorder
The two specific diagnosis noted in the DSM-IV include the following:
1. Anorexia nervosa:
Generally, This Eating Disorder is characterized by refusal to maintain a minimally normal body weight.
Prominent clinical features:
It occurs much more often in females as compared to the males. In detail, The common age of onset is adolescence (13-19 years of age). [1]
There is an intense fear of becoming higher in weight. Additionally, This fear does not decrease even if body becomes very thin and underweight. [1]
The Eating Disorder, Anorexia, is a unique reaction to a variety of external and internal conflicts, such as stress, anxiety, unhappiness also feeling like life is out of control. [2]
There is often a body-image disturbance. The person is unable to perceive own body size accurately. [1]
New research indicates that for a percentage of sufferers, a genetic predisposition may play a role in a sensitivity to develop Besides this, Anorexia, with environmental factors being the trigger. [2]
People with anorexia nervosa typically weigh themselves repeatedly, severely restrict the amount of food they eat, and eat very small quantities of only certain foods. Lastly, They may be afraid of losing control over the amount of food they eat, accompanied by the desire to control their emotions and reactions to their emotions. [2]
Mortality rate
Anorexia nervosa has the highest mortality rate of any mental disorder. While many young people with this disorder die from complications associated with starvation, others die of suicide. In women, suicide is much more common in those with anorexia than with most other mental disorders.
With a low self-esteem and need for acceptance they will turn to obsessive dieting and starvation as a way to control not only their weight, but their feelings also actions regarding; the emotions attached. [2]
Some also feel that they do not deserve pleasure out of life, and will deprive themselves of situations offering pleasure (including eating). [2]
Amenorrhoea, primary or secondary, is often present in females. Women with anorexia nervosa can present with poor sexual adjustment, with conflicts about being a woman and fear of pregnancy. [1]
Behavioral signs
Some of the behavioural signs can be: obsessive exercise, calorie and fat gram counting, starvation and restriction of food, self-induced vomiting, the use of diet pills, laxatives or diuretics to attempt controlling weight, and a persistent concern with body image. [2]
If untreated, the weight loss can become marked. Death may occur due to hypokalemia (caused by self-induced vomiting), dehydration, malnutrition or congestive cardiac failure (caused by anaemia). [1]
Symptoms include:
- Extremely restricted eating
- Extreme thinness (in other words, emaciation)
- A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight
- Intense fear of gaining weight.
- Distorted body image, a self-esteem that is heavily influenced by perceptions of body weight and shape, or a denial of the seriousness of low body weight.
2. Bulimia nervosa:
It is characterized by recurrent and frequent episodes of eating unusually large amounts of food and feeling a lack of control over these episodes. This compulsive overeating is followed by behavior that compensates for the overeating such as forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors. [2]
There is an intense fear of becoming higher in weight. There may be an earlier history of anorexia nervosa.
It is usually body-image disturbance and the person is unable to perceive own body size accurately. [1]
There is a persistent preoccupation with eating, and an irresistible craving for food. There are episodes of overeating in which large amounts of food are consumed within short periods of time (in other words, eating indulges). [1]
This can be indirect relation to how they feel about themselves, or how they feel over a particular event or series of events in their lives. [2]
Research
New research indicates that for a percentage of sufferers, a genetic predisposition may play a role in a sensitivity to develop Bulimia, with environmental factors being the trigger. [2]
People suffering Bulimia are usually aware they have an eating disorder. [2]
Fascinated by food they sometimes buy magazines and cookbooks to read recipes, and enjoy discussing dieting issues. [2]
Some of the behavioural signs can be: Recurring episodes of rapid food consumption followed by tremendous guilt and purging (i.e. laxatives or self-induced vomiting), a feeling of lacking control over their eating behaviours, regularly engaging in stringent diet plans and exercise, the misuse of laxatives, diuretics, and/or diet pills and a persistent concern with body image can all be warning signs someone is suffering with Bulimia. [2]
Symptoms i.e.:
- Chronically inflamed and sore throat
- Swollen salivary glands in the neck and jaw area
- Worn tooth enamel and increasingly sensitive and decaying teeth as a result of exposure to stomach acid
- Acid reflux disorder and other gastrointestinal problems
- Intestinal distress and irritation from laxative abuse
- Severe dehydration from purging of fluids
- Electrolyte imbalance (too low or too high levels of sodium, calcium, potassium and other minerals) which can lead to stroke or heart attack.
3. Compulsive Overeating or Binge Eating disorder :
Compulsive Overeating disorder is the most common eating disorder in the U.S. People with this disorder lose control over their eating. Unlike bulimia nervosa, periods of indulge eating are not followed by purging, excessive exercise, or fasting.
As a result, people with this disorder often are higher in weight. [1]
Additionally, there also may be eating of large amounts of food throughout the day with no planned meal times, eating alone because of being embarrassed, and/or feeling guilty and depressed after overeating. [1]
The disorder is not listed separately in ICD-10 and symptoms of compulsive overeating are also seen in bulimia nervosa. [1]
Fear of not being able to control eating, also while eating, not being able to stop. [2]
Isolation. Fear of eating around and with others. [2]
Chronic dieting on a variety of popular diet plans. [2]
Holding the belief that life will be better if they can lose weight. [2]
Symptoms include:
- Eating unusually large amounts of food in a specific amount of time
- Eating until you are uncomfortably full.
- Feeling distressed, ashamed, or guilty about your eating.
- Frequently dieting, possibly without weight loss.
- Hiding food in strange places ( e.g. closets, cabinets, suitcases, under the bed) to eat at a later time. Either Vague or secretive eating patterns. [2]
- Self-defeating statements after food consumption. [2]
- Eating even when you’re full or not hungry.
- Eating fast during indulges eating episodes.
- Blames failure in social and professional community on weight. [2]
- Holding the belief that food is their only friend. [2]
Other symptoms
- Frequently out of breath after relatively light activities. [2]
- Excessive sweating also shortness of breath. [2]
- High blood pressure also cholesterol. [2]
- Eating alone or in secret to avoid embarrassment.
- Leg and joint pain. [2]
- Weight gain. [2]
- Decreased mobility due to weight gain. [2]
- Loss of either sexual desire or promiscuous relations. [2]
- Mood swings, depression, fatigue. [2]
- Insomnia, poor sleeping habits. [2]
4. Obesity (Overeating Associated with Other Psychological Disturbances):
Obesity caused by a reaction to distressing events is included here. It caused by drugs or endocrine factors, or due to constitutional factors is not considered a psychiatric disorder. [1]
5. Psychogenic Vomiting:
This is clinical syndrome in which biopsychosocial factors interact to produce symptoms which are often mistaken for upper gastrointestinal tract disease, anorexia nervosa, dissociative (conversion) disorder, somatization disorder, or malingering.
The characteristic clinical features include:
- Repeated vomiting, which typically occurs soon after a meal has begun or just after it has been completed.
- Vomiting often occurs in complete absence of nausea or retching (Patients say that food just seems to come back up).
- Vomiting is often self-induced and can be suppressed, if necessary.
- Despite repeated vomiting, weight loss is not usually significant.
- The course of illness is usually chronic with frequent remissions and relapses.
Risk Factors
Risk factors of Eating Disorder
- Eating disorders frequently appear during the teen years or young adulthood but may also develop during childhood or later in life.
- These disorders affect all genders, although rates among women are 2½ times greater than among men.
- Like women who have eating disorders, men also have a distorted sense of body image.
- For example, men may have muscle dysmorphia, a type of disorder marked by an extreme concern with becoming more muscular.
Pathogenesis
Pathogenesis of Eating Disorder
The pathogenesis of eating disorders (EDs) is complex and multifactorial, involving a combination of genetic, biological, psychological, and sociocultural factors.
Genetic Predisposition:
- Family and twin studies have shown a higher concordance rate for EDs in monozygotic twins compared to dizygotic twins, suggesting a genetic contribution.
- Specific genes related to neurotransmitter systems (e.g., serotonin, dopamine) and appetite regulation have been implicated in ED susceptibility.
Biological Factors:
- Dysregulation of neurotransmitter systems, particularly serotonin and dopamine, can contribute to altered appetite, mood, and impulse control.
- Hormonal imbalances, such as altered levels of leptin and ghrelin, can affect hunger and satiety signals.
- Brain imaging studies have revealed structural and functional abnormalities in regions involved in reward processing, emotion regulation, and body image perception.
Psychological Factors:
- Low self-esteem, perfectionism, anxiety, depression, and obsessive-compulsive traits are common personality features associated with EDs.
- Negative body image and body dissatisfaction are key risk factors for ED development.
- Trauma, abuse, or adverse life events can increase vulnerability to EDs.
Sociocultural Factors:
- The thin ideal promoted in media and society can create pressure to conform to unrealistic body standards.
- Family dynamics, such as critical or overprotective parenting, can contribute to ED development.
- Peer pressure and social comparison can reinforce unhealthy eating and body image concerns.[9]
Pathophysiology
Pathophysiology of Eating Disorder
The pathophysiology of eating disorders (EDs) is a complex interplay of biological, psychological, and sociocultural factors. It involves dysregulation of various physiological systems, alterations in neurotransmitter function, and cognitive distortions.
Biological Factors:
- Genetic Predisposition: Studies suggest a heritable component in EDs, with increased risk in individuals with family history. Certain genes related to serotonin and dopamine neurotransmission may be involved.
- Neurotransmitter Imbalance: Dysregulation of serotonin, dopamine, and norepinephrine has been linked to appetite dysregulation, mood disturbances, and obsessive-compulsive behaviors in EDs.
- Hormonal Dysregulation: Altered levels of leptin, ghrelin, and cortisol can contribute to appetite dysregulation and energy imbalance.
- Brain Structure and Function: Neuroimaging studies have revealed alterations in brain regions involved in reward processing, emotion regulation, and body image perception in individuals with EDs.
Psychological Factors:
- Cognitive Distortions: Individuals with EDs often exhibit distorted thoughts and beliefs about body image, food, and self-worth.
- Perfectionism: A tendency towards perfectionism and unrealistic expectations can drive restrictive eating and overvaluation of thinness.
- Low Self-Esteem: Negative self-image and feelings of inadequacy can contribute to the development and maintenance of EDs.
- Emotional Dysregulation: Difficulty managing emotions, such as anxiety and depression, can lead to maladaptive coping mechanisms like restrictive eating.
Sociocultural Factors:
- Thin Ideal Internalization: The societal pressure to achieve a thin body ideal can trigger body dissatisfaction and disordered eating behaviors.
- Media Influence: Exposure to unrealistic body images in media can contribute to body image distortion and increase risk of EDs.
- Family Dynamics: Dysfunctional family relationships, such as enmeshment or criticism, can create a vulnerability to EDs.[10]
Clinical Features
Clinical Features of Eating Disorder
Eating disorders (EDs) vary depending on the specific diagnosis, but some common signs and symptoms can be observed across different types of EDs.
Anorexia Nervosa:
- Significantly low body weight: Often accompanied by a relentless pursuit of thinness and fear of gaining weight.
- Distorted body image: Individuals perceive themselves as higher-weight person even when they are dangerously underweight.
- Amenorrhea: Absence of menstrual periods in females due to hormonal imbalances.
- Restricting food intake: Severely limiting calorie intake and avoiding certain food groups.
- Excessive exercise: Engaging in compulsive exercise to burn calories.
- Physical complications: Malnutrition, electrolyte imbalances, bradycardia, hypotension, lanugo (fine hair growth), and osteoporosis.
Bulimia Nervosa:
- Indulge eating episodes: Recurrent episodes of consuming large amounts of food in a short period, followed by a sense of loss of control.
- Compensatory behaviors: Purging (self-induced vomiting, laxative or diuretic misuse), excessive exercise, or fasting to prevent Higher Weight.
- Fluctuations in body weight: Weight may remain within or slightly above normal range.
- Physical complications: Electrolyte imbalances, dehydration, gastrointestinal problems, dental erosion, and esophageal tears.
Indulge Eating Disorder:
- Recurrent Indulge eating episodes: Similar to bulimia nervosa but without compensatory behaviors.
- Feelings of guilt, shame, and distress: Associated with Indulge eating episodes.
- Weight gain: Often leads to Higher Weight or obesity.
- Physical complications: Obesity-related health problems like type 2 diabetes, hypertension, and cardiovascular disease.
Other Specified Feeding or Eating Disorder (OSFED):
- Atypical anorexia nervosa: Meeting all criteria for anorexia nervosa except significant weight loss.
- Bulimia nervosa of low frequency and/or limited duration: Meeting all criteria for bulimia nervosa but with less frequent Indulge-purge episodes.
- Night eating syndrome: Recurrent episodes of excessive nighttime eating.
- Purging disorder: Purging without Indulge eating.[11]
Sign & Symptoms
Sign & Symptoms of Eating Disorder
- Dramatic weight loss in a relatively short period of time.
- Wearing big or baggy clothes or dressing in layers to hide body shape also weight loss.
- Furthermore, Obsession with weight and complaining of weight problems ( even if "average" weight or thin).
- Additionally, Obsession with continuous exercise.
- Besides this, Frequent trips to the bathroom immediately following meals (occasionally, accompanied with water running in the bathroom for a long period of time to hide the sound of vomiting).
- In brief, Visible food restriction and self-starvation.
- Visible indulging also purging.
- All in all, Use or hiding use of diet pills, laxatives, ipecac syrup ( can cause immediate death !) or enemas.
Isolation
- Fear of eating around and with others.
Unusual food rituals such as shifting the food around on the plate to look eaten; cutting food into tiny pieces; additionally, making sure the fork avoids contact with the lips (using teeth to scrap food off the fork or spoon); chewing food also spitting it out, but not swallowing; dropping food into napkin on lap to later throw away.
Obsession with calories also fat content of foods.
Hiding food in strange places (e.g. closets, cabinets, suitcases, under the bed) to avoid eating (in other words, Anorexia) or to eat at a later time (in other words, Bulimia).
Moreover, Flushing uneaten food down the toilet (can cause sewage problems).
Vague or secretive eating patterns.
Lastly, Keeping a "food diary" or lists that consists of food also behaviours (i.e., purging, restricting, calories consumed, exercise, etc.)
Other symptoms
- Preoccupied thoughts of food, weight also cooking.
- Visiting websites, which promote unhealthy ways to lose weight.
- Additionally, Reading books about weight loss and eating disorders.
- Self-defeating statements after food consumption.
- Hair loss. Either Pale or "gray" appearance to the skin.
- Dizziness also headaches.
- Frequent sore throats also swollen glands.
- In detail, Low self-esteem. Feeling worthless. Often putting themselves down · also complaining of being "too foolish" or "too fat" and saying they do not matter. Need for acceptance and approval from others.
- Complaints of often feeling cold.
- Low blood pressure.
- Moreover, Loss of menstrual cycle.
- Constipation or incontinence.
- Either Bruised or calluses knuckles; bloodshot or bleeding in the eyes; light bruising under the eyes also on the cheeks.
- Perfectionist personality.
- Loss of sexual desire or promiscuous relations.
- Mood swings, depression, fatigue.
- Insomnia. All in all, Poor sleeping habits.
Clinical Examination
Clinical examination of eating disorder
The Eating Disorder Examination assesses the frequency of disordered eating behaviors over the past 28 days. The questions are organized into four groupings: restraint, eating concern, shape concern, and weight concern.
Four groupings of the EDE
The portion of the Eating Disorder Examination concerned with restraint asks questions about restraint overeating, avoiding specific foods, dietary rules, avoidance of eating, and emptiness felt in the stomach.
The eating concern portion of the Eating Disorder Examination asks about preoccupation with food, fear of losing control overeating, eating in secret, social eating, and guilt after eating.
The shape concern portion of the Eating Disorder Examination asks about body concerns including specifically a flat stomach, preoccupation with body shape or weight, the importance of shape, fear of weight gain, dissatisfaction with body shape, discomfort in seeing the body, avoidance of exposure of the body, and feelings of fatness.
The weight concern portion of the Eating Disorder Examination investigates the importance of weight to the patient, any reactions to prescribed weighing, preoccupation with body shape and weight, dissatisfaction with current weight, and a desire to lose weight.
The Eating Disorder Examination tool is extensive and may be part of a larger medical examination for determining if a patient has an eating disorder. The full medical examination for an eating disorder may also include a medical history, a physical exam, and various clinical or diagnostic tests. (4)
Diagnosis
Diagnosis of Eating Disorder
- Researchers are finding that eating disorders are caused by a complex interaction of genetic, biological, behavioral, psychological, and social factors.
- Eating disorders run in families. Researchers are working to identify DNA variations that are linked to the increased risk of developing eating disorders.
- Brain imaging studies are also providing a better understanding of eating disorders.
- For example, researchers have found differences in patterns of brain activity in women with eating disorders in comparison with healthy women.
Differential Diagnosis
Differential diagnosis of eating disorder
- Anxiety
- Depression
- Obsessive-compulsive disorder (OCD)
- Post-traumatic stress disorder (PTSD)
- Addiction like Laxatives, Diuretics, Diet pills
- Diabulimia
- Pregnancy (5)
Complications
Complications
Eating disorders (EDs) can lead to a wide range of serious and potentially life-threatening complications, affecting multiple organ systems and impacting overall health and well-being.
Physical Complications:
- Cardiovascular: Bradycardia, hypotension, arrhythmias, heart failure, mitral valve prolapse, and sudden cardiac death due to electrolyte imbalances.
- Gastrointestinal: Delayed gastric emptying, constipation, acid reflux, pancreatitis, and bowel perforation (rare).
- Endocrine: Amenorrhea, infertility, hypothyroidism, and osteopenia/osteoporosis due to hormonal dysregulation and malnutrition.
- Metabolic: Electrolyte imbalances (hypokalemia, hyponatremia, hypophosphatemia), dehydration, and refeeding syndrome (a potentially fatal condition associated with rapid reintroduction of nutrition).
- Neurological: Seizures, peripheral neuropathy, and cognitive impairment.
- Hematological: Anemia and impaired immune function.
- Dermatological: Dry skin, brittle hair and nails, lanugo (fine hair growth), and hair loss.
Psychological Complications:
- Depression and anxiety: EDs are often comorbid with mood and anxiety disorders, which can worsen the prognosis.
- Suicidal ideation and attempts: Individuals with EDs are at increased risk for self-harm and suicide.
- Substance abuse: EDs can co-occur with substance use disorders, further complicating treatment.
Social Complications:
- Social isolation: EDs can lead to withdrawal from social activities and relationships.
- Impaired academic or occupational functioning: The physical and psychological effects of EDs can interfere with school or work performance.
- Financial difficulties: The cost of treatment and lost productivity due to EDs can cause financial strain.[12]
Investigations
Investigation of Eating Disorder
While there is no one specific lab test to confirm an eating disorder diagnosis.
Your healthcare provider will likely want a blood test to check your complete blood count (CBC), along with your:
- Electrolytes
- Liver function
- Kidney function
- Thyroid function
- X-Ray
- ECG (5)
Treatment
Treatment of Anorexia Nervosa
It can be considered in two phases, which often merge into each other.
- Short-term treatment: to encourage weight gain and correct nutritional deficiencies, if any.
- Long-term treatment: aimed at maintaining the near normal weight achieved in short-term treatment and preventing relapses. [1]
1. Behaviour therapy (BT):
Behavioural treatments are based on providing positive reinforcements (and at times, negative reinforcements) contingent on weight gain by the patient.The weight gain should not exceed 1.5 to 2 kg in a fortnight. As patients are usually unable to eat a large meal, especially in the initial part of treatment, it is advisable to suggest more number of meals (about six) per day.
Occasionally, forceful Ryle’s tube feeding may be needed initially, in resistant patients. [1]
2. Individual psychotherapy:
It is often helpful in addition to supportive physical treatment. This could involve psychotherapy with a focus on cognitive behaviour therapy, psychodynamic principles or supportive measures. [1]
3. Hospitalisation:
Hospitalisation with adequate nursing care for food intake and weight gain, can be helpful in short-term treatment as well as prevention and/ or treatment of complications. It is important to keep a close eye on water and electrolyte balance, need for supplementation with vitamins and minerals, also prevent osteoporosis. [1]
4. Drugs:
i. Antipsychotics:
Chlorpromazine is rarely used these days. Furthermore, Olanzapine has efficacy in improving weight gain but it is important to be aware of possibility of prolongation of QTc particularly in patients with low BMI.
ii. Antidepressants:
(e.g. fluoxetine, clomipramine) for treatment of anorexia nervosa and/ or associated depression.
iii. Cyproheptadine:
In brief, This is particularly helpful in inducing weight gain, decreasing depressive symptoms also increasing appetite, if anorexia is actually present. The usual dose is 8-32 mg/ day, in divided doses.
5. Group therapy and family therapy:
It can be helpful in psychological-education for the patient and carers/ family about nature of anorexia nervosa and its treatment. Psychological-education may also include discussion of current social norms of slimming and fitness. [1]
Treatment of Bulimia Nervosa and Binge Eating disorder:
1. Behaviour therapy:
This is based on providing positive reinforcements (also at times negative reinforcements) contingent on the control of indulge eating by the patient. [1]
2. Individual psychotherapy.
3. Antidepressant drugs:
They are an important adjunct to other modes of therapy.
A Selective serotonin uptake inhibitor (in other words, SSRI) such as Fluoxetine (in doses of 20-60 mg) is particularly useful as it can cause loss of appetite at least in the initial phase of treatment, along with its antidepressant effect.
The drugs used in the past have included tricyclic antidepressants such as imipramine, though they are currently not widely used. [1]
4. Group therapy and family therapy:
These methods are used for psychological-education of patient and carers/family about nature of bulimia nervosa and its treatment. [1]
Treatment of Obesity (Overeating Associated with Other Psychological Disturbances):
It depend on the underlying cause; for example, psychotherapy (for present or past psychological distress), antidepressants (for depression), advice from dietician, drug treatment, or even bariatric surgery. [1]
Treatment of psychogenic vomiting:
1. The first and most important step is correct diagnosis and exclusion of other physical and/or psychiatric causes.
2. Identification of psychosocial stressor.
3. Environmental manipulation and encouragement of coping strategies to deal with stress.
4. Psychotherapy of either cognitive behavioural or psychodynamic nature. [1]
Prevention
Prevention of Eating Disorder
- Set a good example by eating well- If you live with or know someone who might be at risk for developing an eating disorder, you can help them by being a good role model. Eat regular, nutritious meals and choose healthy snacks when you get hungry between mealtimes
- Encourage your loved one to eat when they are hungry- Talk to them about how to listen to their body and recognize the signals that they are hungry or full. Discuss how being mindful when eating can help them meet their body’s needs and avoid over- or undereating.
- Avoid making negative or shaming comments about food and eating- Help your loved ones maintain a healthy relationship with food and eating by focusing on the positive. Don’t make critical or judgmental comments about what others are eating, and also avoid talking negatively about your own eating habits.
- Keep healthy foods around the house- If you’re concerned about the eating habits of someone you live with, make sure they have access to plenty of fresh, nutritious foods. Keep your fridge and cabinets stocked with lots of fruits, vegetables, and healthy snack options, such as yoghurt, nuts, or whole wheat crackers.
- Educate yourself and your family about how diet can affect your health- Take some time to learn about the benefits of eating healthy and the potential consequences of not eating well. Check out some books on nutrition from your library or get some information from your family doctor or a registered dietitian. Talk with your family about issues like.
- Practice positive talk about people’s bodies.
- Discuss healthy ways to cope with stress and negative feelings.(6)
Homeopathic Treatment
Homeopathic Treatment of Eating Disorder
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
Which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. Now a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improve with homeopathic medicines.
Homeopathic Medicines for Eating Disorder:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy, potency and repetition of dose by Homeopathic doctor.
So, here we describe homeopathic medicine only for reference and education purpose. Do not take medicines without consulting registered homeopathic doctor (BHMS or M.D. Homeopath).
Anorexia Remedies: [2]
Arsenicum alb:
Extreme fastidiousness especially about germs and dirt. Anorexia coupled with fear of being poisoned. Fear of getting certain diseases so they start starving.
Carcinosin:
Obsessive compulsive disorder. Perfectionism, fear of becoming fat, fear of rejection. Etiology-abuse, grief or fears, often related to weight. Chronic insomnia, workaholics.
Hyoscyamus:
Anorexia plus mania, insanity, fear of being poisoned. Could have pathological jealousy, over concern about weight and getting fat.
Ignatia:
Perfectionism, fear of becoming fat, fear of rejection. Hysteria loss of control of emotions, fainting. Etiology-grief or big disappointment, often related to weight.
Natrum mur:
Most often indicated remedy in anorexia, a lot of guilt. Fear of being rejected, hurt easily, very self-conscious. Dry lips, emaciate, and dry skin, constipated, lose appetite. Behind this is perfectionism and fear of becoming fat. Nat mur have more confidence.
Phosphoric acid:
Etiology-grief with loss of appetite with emaciation, pining away from loss of love, second stage they get indifferent to all emotions and food. Deadness inside (Sepia, Aurum met). Grief anorexia than some chronic disease.
Platina met:
Obsessed with their appearance, fear of becoming fat. Very obsessive and impulsive personality, egocentric and arrogant, all tied up with their sexuality, religious mania.
Pulsatilla:
Feeling of worthlessness, unloved, loneliness, fixed ideas about. Food especially certain foods are bad, than amount of foods that are bad grows, fear of gaining weight, pulsatilla gain weight easily, they can eat a pastry and swear they gained weight. Ignatia, Puls. and Nat. mur. Are constantly weighing themselves. Scanty menses.
Sepia:
Anorexia plus hormonal problems, nausea, sensitivity to smell. Disgust for food, worse since childbirth, hormones causes lack of appetite.
Staphysagria:
Acute of Carcinosin, more visible, visibly upset. Carcinosin can control it more, Staph. may it more. Additionally, Deep sense of worthlessness and depression, even suicidal. Humiliation, mortified, put down, criticized, zero confidence. Fear of becoming fat and neglected by others.
Tarentula:
Mania could be religious mania. In detail, Underneath you have a fear of being poisoned. Obsessiveness about weight, very restless and hyper energy people, they do everything fast-talk, move.
Thuja occid:
In brief, Fear of being impure, dirty blood, anxiety about health, obsessed with idea of have to clean them out. Fear of eating more also becoming fat.
Veratrum alb:
Religious mania, loquacious, end of world is coming. Punish themselves, fast to appease god. Lastly, Behind this you see guilt. [2]
Bulimia Remedies: [2]
Argentum nit:
Indulging especially with chocolate, fixed ideas, impulsive behaviour, anticipation, overriding impulses for certain foods, chocolate, salty foods, they will eat a whole box of chocolates until they get sick.
Carcinosin:
Obsessive compulsive disorder. Moreover, Perfectionism, fear of becoming fat, fear of rejection. Etiology-abuse, grief or fears, often related to weight.
Ignatia:
Perfectionism, fear of becoming fat, fear of rejection. Additionally, Hysteria-loss of control of emotions, fainting. Etiology-grief or big disappointment, often related to weight.
Medorrhinum:
Ups and down in the person’s energy, very outgoing for 2 or 3 days than wiped out for several days and with that their diets fluctuate from good to indulging. Bulimia also with alcohol and drugs.
Natrum mur:
Often indicated remedy in anorexia, a lot of guilt. Fear of being rejected, hurt easily. Very self-conscious of their weight.
Pulsatilla:
Fear of being abandoned and unloved. Fixed ideas about food, their weight, they gain and lose weight easily, eat and satiate to console themselves, consume excessively out of loneliness, or depression, then they get guilt and fear about it and then suppress it.
Staphysagria:
Indulging out of guilt, depression. Poor self-confidence and worthlessness. It is out of self-denial, they do not deserve that -lemon meringue pie so they suppress their desire for it, and then indulge on it. [2]
Diet & Regimen
Diet & Regimen of Eating Disorder
- Encourage weight gain
- Take well balanced diet
- Take part in social activities
- Avoid talking about weight & food
- Avoid over exercise
Do’s and Don'ts
Do’s and Don’ts
Do’s:
Educate yourself: Learn about the different types of eating disorders, their signs and symptoms, and available treatment options.
Express your concern: Talk to your loved one about your worries in a caring and non-judgmental way. Focus on specific behaviors that concern you rather than their appearance.
Listen empathetically: Let your loved one share their feelings and experiences without interrupting or offering unsolicited advice.
Offer support: Let your loved one know that you are there for them and encourage them to seek professional help.
Seek support for yourself: Join a support group or talk to a therapist to help you cope with the challenges of supporting someone with an eating disorder.
Encourage professional help: Help your loved one find a qualified therapist, dietitian, or physician specializing in eating disorders.
Be patient and understanding: Recovery from an eating disorder takes time and effort. Be patient with your loved one and celebrate their progress, no matter how small.
Don’ts:
Avoid blaming or shaming your loved one for their eating disorder. It is not their fault, and they need your support, not your judgment.
Avoid commenting on their weight, shape, or size. Focus on their health and well-being instead.
Don’t try to force them to eat or restrict their food intake. This can worsen the eating disorder and damage your relationship.
Even if your loved one resists help initially, don’t give up on them. Continue to offer your support and encourage them to seek treatment.
Eating disorders are serious mental illnesses that require professional help. Don’t ignore the signs and symptoms, hoping they will go away on their own.
Unless you are a qualified mental health professional, don’t try to treat your loved one’s eating disorder yourself. Encourage them to seek professional help.
Remember, eating disorders are treatable, and recovery is possible. With the right support and treatment, individuals with eating disorders can lead healthy and fulfilling lives.
Terminology
Terminology of Eating Disorder
- Eating Disorder (ED): A serious mental illness characterized by persistent disturbances in eating behaviors, thoughts, and emotions surrounding food and body image.
- Anorexia Nervosa (AN): An ED characterized by significant restriction of energy intake, intense fear of gaining weight, and a distorted body image. Individuals with AN often have a significantly low body weight.
- Bulimia Nervosa (BN): An ED marked by recurrent episodes of Indulge eating (consuming large amounts of food in a short period with a loss of control), followed by compensatory behaviors like purging (self-induced vomiting, laxative misuse), excessive exercise, or fasting.
- Indulge Eating Disorder (IED): An ED characterized by recurrent episodes of Indulge eating without compensatory behaviors. Individuals with IED often experience feelings of guilt, shame, and distress after Indulge eating episodes.
- Avoidant/Restrictive Food Intake Disorder (ARFID): An ED characterized by a lack of interest in food, avoidance of certain foods based on sensory characteristics, or fear of adverse consequences of eating.
- Other Specified Feeding or Eating Disorder (OSFED): A diagnostic category for EDs that do not meet the full criteria for AN, BN, BED, or ARFID.
- Body Image: A person’s perception of their body size, shape, and appearance. Body dissatisfaction is a common feature of EDs.
- Compensatory Behaviors: Actions taken to prevent weight gain or "undo" the effects of consume excessive eating, such as purging, excessive exercise, or fasting.
- Purging: The act of self-induced vomiting, laxative or diuretic misuse to eliminate food from the body.
- Restricting: Severely limiting food intake and avoiding certain food groups to control weight.
- Weight Stigma: Negative attitudes, beliefs, and discrimination towards individuals based on their weight or body size.
- Recovery: The process of overcoming an eating disorder and achieving a healthy relationship with food and body image. Recovery often involves a combination of therapy, nutritional counseling, and medical care.
Homoeopathic Terminology
In the context of homeopathy and eating disorders (EDs), there are some specific terminologies and concepts that are important to understand
- Homeopathy: A system of alternative medicine based on the principle of "like cures like," using highly diluted substances to trigger the body’s natural healing processes.
- Simillimum: The homeopathic remedy that most closely matches the totality of symptoms experienced by the individual with the ED.
- Constitutional Remedy: A homeopathic remedy that is chosen based on the individual’s overall physical, mental, and emotional characteristics, rather than just the specific symptoms of the ED.
- Aggravation: A temporary worsening of symptoms after taking a homeopathic remedy, which is sometimes seen as a sign that the remedy is working.
- Proving: A process in which healthy individuals take a homeopathic substance and record their symptoms, which are then used to determine the remedy’s therapeutic properties.
- Repertory: A reference book used by homeopaths to find remedies that match specific symptoms.
- Materia Medica: A collection of information on the therapeutic properties of homeopathic substances.
- Miasm: A concept in homeopathy that refers to an underlying predisposition to disease, which can be inherited or acquired.
- Nosode: A homeopathic remedy made from a disease product, such as a tissue sample or discharge.
- Potentization: The process of diluting and succussing (shaking) a homeopathic substance to increase its potency.
- Vital Force: The energy that animates the body and is responsible for maintaining health. Homeopaths believe that EDs are caused by a disturbance in the vital force.
It is important to note that homeopathy is a complementary and alternative medicine (CAM) approach to treating EDs. It is not a substitute for conventional medical care, and individuals with EDs should always consult with a qualified healthcare professional before starting any new treatment.
References
Reference of Eating Disorder
- A Short Textbook of PSYCHIATRY 7th edition by Niraj Ahuja / ch 12.
- Homeopathy in treatment of Psychological Disorders by Shilpa Harwani / ch 15.
- Eating disorders – Symptoms and causes – Mayo Clinic
- Eating Disorder Examination (eatingdisorders.com)
- Eating Disorder Diagnosis: Tests, Screening, and Criteria (verywellhealth.com)
- 3 Simple Ways to Prevent Eating Disorders – wikiHow
- Shah M. Eating Disorders in India: A Systematic Review. Acta Neurophysiol 2023, 4(3): 180022.
- Vaidyanathan S, Kumar K, Gubbi S. Eating Disorders: An Overview of Indian Research. Indian J Psychol Med 2019;41(3):215-22.
- Kaplan & Sadock’s Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry – 12th Edition.
- The American Psychiatric Association Publishing Textbook of Psychiatry.
- Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
- Clinical Manual of Eating Disorders
Also Search As
Eating Disorder Also Search As
Online Resources:
- Search Engines: Use search terms like "eating disorder," "anorexia nervosa," "bulimia nervosa," "binge eating disorder," or "ARFID" on popular search engines like Google, Bing, or DuckDuckGo.
- Websites of Reputable Organizations: Visit the websites of organizations like the National Eating Disorders Association (NEDA), the Academy for Eating Disorders (AED), and the National Institute of Mental Health (NIMH) for reliable information and resources.
- Online Forums and Support Groups: Connect with others who are going through similar experiences on online forums or support groups dedicated to EDs.
- Social Media: Follow organizations and professionals who share information about EDs on platforms like Twitter, Instagram, or Facebook.
- Educational Videos: Watch videos on platforms like YouTube or TED Talks that discuss EDs, their symptoms, causes, and treatment options.
- Online Libraries and Databases: Access research articles and publications on EDs through online libraries or academic databases.
Offline Resources:
- Libraries: Consult books, journals, and other resources on EDs available in libraries.
- Healthcare Professionals: Talk to doctors, therapists, or other healthcare providers who specialize in EDs for personalized guidance and support.
- Support Groups: Attend local support groups for individuals with EDs or their families to connect with others who understand the challenges and provide emotional support.
- Community Centers: Some community centers offer educational programs or workshops on EDs.
- Schools and Universities: Many schools and universities have counseling centers that offer support and resources for students struggling with EDs.
Important Considerations:
- Credibility of Sources: Ensure that the information you find is from reputable sources and based on scientific evidence.
- Confidentiality and Privacy: If seeking help online, choose platforms that prioritize confidentiality and privacy.
- Trigger Warning: Be aware that some content about EDs may be triggering for individuals struggling with these disorders. Seek support from a trusted person or professional if needed.
There are numerous ways to search for information about eating disorders (EDs) using different platforms and resources:
Online:
- Search Engines: Utilize search engines like Google, Bing, or DuckDuckGo with keywords such as "eating disorder," "anorexia nervosa," "bulimia nervosa," "binge eating disorder," or "ARFID." You can also search for specific symptoms, treatment options, or support groups.
- Websites of Reputable Organizations: Explore websites of organizations specializing in EDs, such as:
- National Eating Disorders Association (NEDA): Provides information, support, and resources for individuals and families affected by EDs.
- Academy for Eating Disorders (AED): A professional organization dedicated to research, education, and treatment of EDs.
- National Institute of Mental Health (NIMH): Offers information on mental health disorders, including EDs.
- Online Forums and Support Groups: Engage with others experiencing similar challenges through online forums and support groups dedicated to EDs. This can provide a safe space for sharing experiences and seeking advice.
- Social Media: Follow organizations, professionals, and support groups on social media platforms like Twitter, Instagram, or Facebook to stay updated on the latest information and resources.
- Educational Videos and Podcasts: Watch videos on platforms like YouTube or TED Talks and listen to podcasts that discuss EDs, their symptoms, causes, and treatment options.
- Online Libraries and Databases: Access research articles and publications on EDs through online libraries or academic databases like PubMed or Google Scholar.
Offline:
- Libraries: Explore books, journals, and other resources on EDs available in libraries. Librarians can assist in finding relevant materials.
- Healthcare Professionals: Consult with doctors, therapists, or other healthcare providers who specialize in EDs for personalized guidance and support.
- Support Groups: Attend local support groups for individuals with EDs or their families to connect with others who understand the challenges and provide emotional support.
- Community Centers and Organizations: Some community centers offer educational programs or workshops on EDs. Check with local organizations that focus on mental health or wellness.
- Schools and Universities: Many schools and universities have counseling centers that offer support and resources for students struggling with EDs.
Frequently Asked Questions (FAQ)
What is Eating Disorder?
Eating disorders are actually serious and often fatal illnesses that cause severe disturbances to a person’s eating behaviors.
Give types of Eating Disorder?
- Anorexia Nervosa
- Bulimia Nervosa
- Compulsive Overeating or Binge Eating Disorder
- Obesity
- Psychogenic Vomiting
What causes Eating Disorder?
- Frequently appear during the teen years or young adulthood
- Affect all genders
- Women are 2½ times greater than among men.
- Distorted sense of body image
Are eating disorders treatable?
Yes,
absolutely. Treatment often involves a combination of therapy, nutritional counseling, and sometimes medication. Early intervention is key for the best outcomes.
What are the symptoms of Eating Disorder?
- Dramatic weight loss
- Wearing big or baggy clothes
- Obsession with weight
- Obsession with continuous exercise.
- Frequent trips to the bathroom immediately following meals
- Visible food restriction and self-starvation.
- Visible indulging and/or purging.
- Isolation
Can homeopathy help with eating disorders?
Homeopathy offers a holistic approach to eating disorders, aiming to address the underlying emotional, mental, and physical imbalances that contribute to unhealthy eating patterns. While not a replacement for conventional medical care, it can be a complementary therapy.
How does homeopathic treatment for eating disorders work?
Homeopaths take a detailed case history to understand the individual’s unique symptoms, emotional state, and overall constitution. They then prescribe individualized remedies that stimulate the body’s self-healing abilities to restore balance.
What are the warning signs of an eating disorder?
Warning Sign
Signs vary, but can include drastic weight changes, preoccupation with food or body image, changes in eating habits, social withdrawal, and physical symptoms like fatigue or dizziness.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Eating Disorder?
- Arsenicum alb
- Carcinosin
- Hyoscyamus
- Ignatia
- Natrum mur
- Phosphoric acid
- Platina met
- Pulsatilla
- Sepia
How long does homeopathic treatment for eating disorders take?
Treatment time
The duration of treatment varies depending on the severity of the eating disorder, the individual’s response to treatment, and other factors. Some individuals may see improvements within weeks or months, while others may require longer-term treatment.
What is the prognosis for eating disorders with homeopathic treatment?
The prognosis for eating disorders varies depending on the severity of the condition, individual response to treatment, and the presence of any co-occurring mental health issues. Homeopathy may contribute to a positive outcome by addressing underlying emotional and psychological factors.
