Osteoporosis
Definition
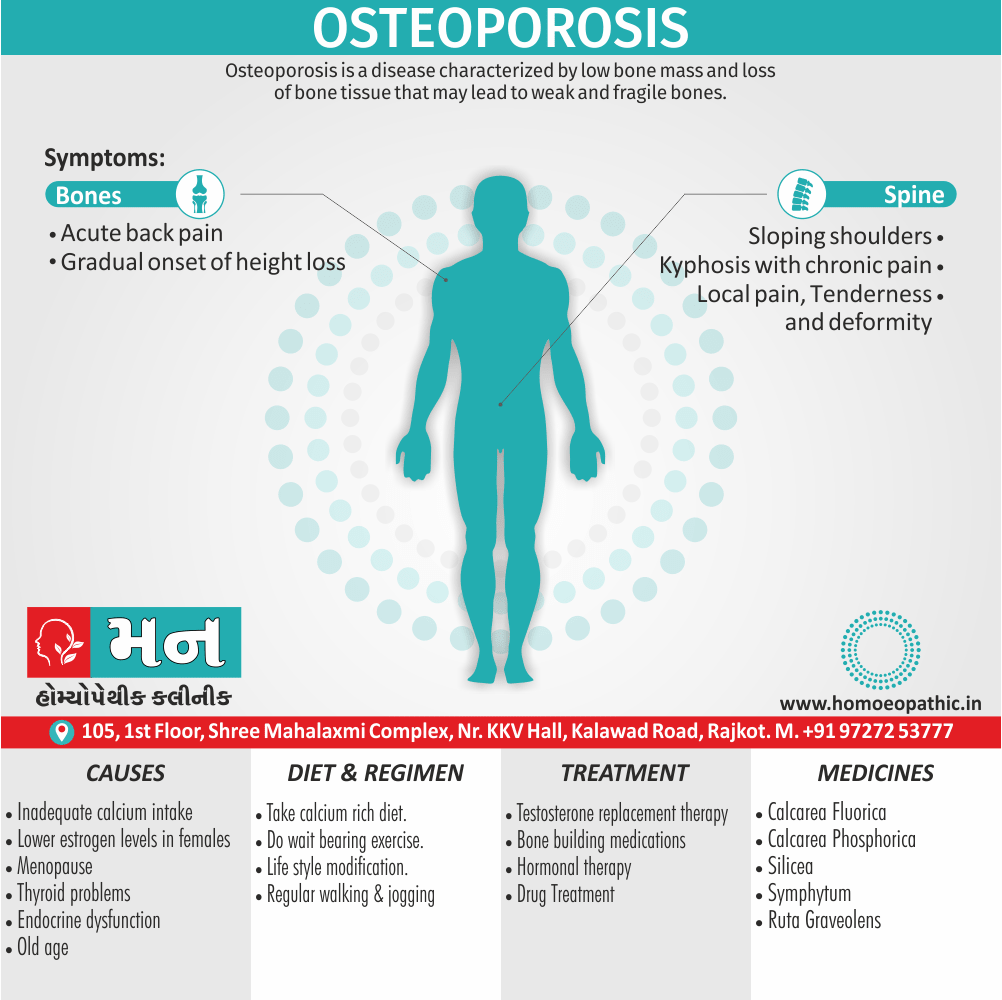
Osteoporosis is a disease characterized by low bone mass and loss of bone tissue that may lead to weak and fragile bones. [4]
There aren’t true synonyms for "osteoporosis" as it’s a specific medical condition. However, depending on the context, you can use these alternatives:
- Bone loss: This is a general term that encompasses osteoporosis but can also refer to other causes of decreased bone density.
- Decreased bone density: Similar to bone loss, this is more general but doesn’t specify the cause.
- Porous bones: This descriptive term highlights the weakened structure of bones in osteoporosis.
For a more specific but non-medical term:
- Brittle bone disease: This emphasizes the increased risk of fractures.
Important Note: These terms are for informational purposes only. If you’re looking for medical advice, consult a healthcare professional.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview
- In general, Osteoporosis is the most common bone disease and affects millions of people worldwide.
- Fractures related to osteoporosis are estimate to affect around 30% of women also 12% of men in developed countries, and are a major public health problem.
- Specifically, In the UK alone, fractures are sustain by over 250000 individuals annually, with treatment costs of about £1.75 billion.
- Osteoporotic fractures can affect any bone, but the most common sites are the forearm (Colles fracture), spine (vertebral fracture) and hip.
- Of these, hip fractures are the most serious.
- Their immediate mortality is about 12% and there is a continue increase in mortality of about 20% when compared with age matched controls.
- All in all, the defining feature of osteoporosis is reduce bone density, which causes a microarchitectural deterioration of bone tissue and leads to an increased risk of fracture.
Prevalence
- The prevalence of osteoporosis increases with age, reflecting the fact that bone density declines with age, especially in women. [1]
- Osteoporosis causes bones to become weak and brittle. So brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture.
- Bone is living tissue that is constantly being break down also replace.
- Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
- Especially older women who are past menopause are at highest risk.
- Medications, healthy diet and weight-bearing exercise can help prevent bone loss or strengthen already weak bones. [2]
Epidemiology
Indian Epidemiology:
Osteoporosis poses a significant health concern in India, affecting a substantial portion of the population. Studies have indicated varying prevalence rates across different regions and demographics.
- A study published in 2022 found the overall prevalence of osteoporosis in India to be 18.3%, with osteopenia affecting 49.9% of the population (Prevalence of osteoporosis in India: an observation of 31238 adults, 2022).[6]
- Another study from 2022 revealed a slightly higher prevalence of osteoporosis in females (26.3%) compared to males (10.9%) (Prevalence of osteoporosis in India, 2022).[7]
- Postmenopausal women are particularly vulnerable, with osteoporosis prevalence reaching 33.1% in this group (Prevalence of osteoporosis in India: an observation of 31238 adults, 2022).[6]
- Regional variations exist, with the southern region showing a higher prevalence of osteoporosis compared to the northern region (Prevalence of osteoporosis in India: an observation of 31238 adults, 2022).[6]
- The Old Age population (≥60 years) also experiences a higher prevalence of osteoporosis compared to younger adults (Prevalence of osteoporosis in India: an observation of 31238 adults, 2022).[6]
These figures highlight the widespread nature of osteoporosis in India and emphasize the need for increased awareness, preventive measures, and effective treatment strategies to address this growing public health challenge.
Note: The prevalence rates mentioned may vary slightly across different studies and populations due to methodological differences and sampling techniques. It’s essential to consult healthcare professionals for personalized assessments and recommendations.
Causes
Causes
Osteoporosis occurs when there is an imbalance between new bone formation and old bone resorption.
The body may fail to form enough new bone, or too much old bone may be reabsorbed, or both.
Two essential minerals for normal bone formation are calcium and phosphate. Throughout youth, the body uses these minerals to produce bones.
Calcium:
- It is essential for proper functioning of the heart, brain, and other organs.
- To keep those critical organs functioning, the body reabsorbs calcium that is store in the bones to maintain blood calcium levels.
- If calcium intake is not sufficient or if the body does not absorb enough calcium from the diet, bone production and bone tissue may suffer.
- Thus, the bones may become weaker, resulting in fragile and brittle bones that can break easily.
- Usually, the loss of bone occurs over an extended period of years.
Hormones:
- The leading cause of osteoporosis is a lack of certain hormones, particularly estrogen in women and androgen in men.
- Women, especially those older than 60 years of age, are frequently diagnosed with the disease.
- Menopause is accompany by lower estrogen levels and increases a woman’s risk for osteoporosis.
Other factors:
- They may contribute to bone loss in this age group include;
- Inadequate intake of calcium & vitamin D
- Lack of weight-bearing exercise
- Other age-related changes in endocrine functions (in addition to lack of estrogen)
- Overuse of corticosteroids (e.g. Cushing syndrome)
- Thyroid problems
- Lack of muscle use
- Bone cancer
- Certain genetic disorders
- Use of certain medications
- Problems such as low calcium in the diet
Types
Types of Osteoporosis
Osteoporosis can be classified into two main types:
Primary Osteoporosis: This type is associated with the natural aging process and hormonal changes, particularly the decline in estrogen levels in women after menopause and testosterone in men. It is further divided into two subtypes:
Type 1 (Postmenopausal Osteoporosis): Primarily affects women in the first 5-10 years after menopause due to rapid bone loss caused by estrogen deficiency. It predominantly leads to fractures in the spine and wrist.
Type 2 : Affects both Xenders over the age of 70. It is characterized by a slower rate of bone loss and typically results in fractures of the hip, spine, and other bones.
Secondary Osteoporosis: This type occurs as a consequence of an underlying medical condition, medication use, or lifestyle factors that negatively impact bone health. Some common causes include:
- Medications: Long-term use of corticosteroids, certain anticonvulsants, and some cancer treatments.
- Medical conditions: Endocrine disorders (e.g., hyperthyroidism, Cushing’s syndrome), malabsorption syndromes, rheumatoid arthritis, and chronic kidney disease.
- Lifestyle factors: Excessive alcohol consumption, smoking, and prolonged immobility.[8]
This comprehensive textbook provides in-depth information about the various types of osteoporosis, their causes, diagnostic approaches, and treatment options.
Risk Factors
Risk factors:
- Women are at a greater risk than men, especially women who are thin or have a small frame, as are those of advanced age.
- Women who are white or Asian, especially those with a family member with osteoporosis, have a greater risk of developing osteoporosis than other women.
- Woman who are postmenopausal, including those who have had early or surgically induced menopause, or abnormal or absence of menstrual periods, are at greater risk.
- Cigarette smoking, eating disorders such as anorexia nervosa or bulimia, low amounts of calcium in the diet, heavy alcohol consumption, inactive lifestyle, also use of certain medications, such as corticosteroids and anticonvulsants, are also risk factors.
- Rheumatoid arthritis itself is a risk factor for osteoporosis.
- Having a parent who has/had osteoporosis is a risk factor for the offspring. [3]
Pathogenesis
Pathogenesis
Osteoporosis is a complex, multifactorial condition characterized by a decrease in bone mass and deterioration of bone microarchitecture, leading to increased bone fragility and fracture risk. The pathogenesis of osteoporosis involves an imbalance between bone resorption and bone formation, resulting in a net loss of bone tissue over time.
Key factors contributing to the pathogenesis of osteoporosis include:
Imbalance in Bone Remodeling: Bone remodeling is a continuous process involving bone resorption by osteoclasts and bone formation by osteoblasts. In osteoporosis, there is an uncoupling of this process, with increased osteoclast activity and/or decreased osteoblast activity, leading to a net loss of bone mass.
Age-Related Changes: With aging, there is a natural decline in bone mass and changes in bone microarchitecture. This decline is accelerated in osteoporosis, particularly in postmenopausal women due to estrogen deficiency. Estrogen plays a crucial role in maintaining bone health by inhibiting osteoclast activity and promoting osteoblast activity.
Hormonal Imbalances: Other hormonal imbalances, such as hyperparathyroidism, hyperthyroidism, and glucocorticoid excess, can also contribute to osteoporosis by increasing bone resorption and/or decreasing bone formation.
Nutritional Deficiencies: Inadequate intake of calcium and vitamin D, essential for bone health, can increase the risk of osteoporosis. Calcium is a major component of bone tissue, and vitamin D is necessary for calcium absorption and utilization.
Genetic Factors: Genetic predisposition plays a significant role in determining peak bone mass and susceptibility to osteoporosis. Several genes have been identified as potential risk factors for osteoporosis.
Lifestyle Factors: Sedentary lifestyle, smoking, excessive alcohol consumption, and certain medications can also increase the risk of osteoporosis by negatively impacting bone health.[9]
Pathophysiology
Pathophysiology
- Osteoporosis occurs because of a defect in attaining peak bone mass and/or because of accelerated bone loss.
- In normal individuals, bone mass increases during skeletal growth to reach a peak between the ages of 20 and 40 years but falls thereafter.
- In women there is an accelerated phase of bone loss after the menopause due to oestrogen deficiency, which causes uncoupling of bone resorption and bone formation, such that the amount of bone removed by osteoclasts exceeds the rate of new bone formation by osteoblasts.
- Age related bone loss is a distinct process that accounts for the gradual bone loss that occurs with advancing age in all genders.
- Bone resorption is not particularly increased but bone formation is reduced and fails to keep pace with bone resorption.
Accumulation of fat
- Accumulation of fat in the bone marrow space also occurs because of an age related decline in the ability of bone marrow stem cells to differentiate into osteoblasts and an increase in their ability to differentiate into adipocytes.
- Peak bone mass and bone loss are regulated by both genetic and environmental factors.
- Genetic factors account for up to 80% of the population variance in peak bone mass and other determinants of fracture risk, such as bone turnover and bone size.
- Environmental factors, such as exercise and calcium intake during growth and adolescence, are important in maximising peak bone mass and in regulating rates of postmenopausal bone loss.
- Smoking has a detrimental effect on bone mineral density (BMD) and is associate with an increased fracture risk, partly because female smokers have an earlier menopause than nonsmokers.
- Heavy alcohol intake is a recognise cause of osteoporosis and fractures, but moderate intake does not substantially alter risk. [1]
Clinical Features
Clinical Features
Osteoporosis is often called a "silent disease" because bone loss occurs without symptoms in its early stages. However, as the disease progresses, it can manifest with various clinical features:
Fragility Fractures: The most common and serious clinical feature of osteoporosis is the occurrence of fragility fractures, defined as fractures that occur from minimal trauma, such as a fall from standing height or less. The most common sites of fragility fractures include the spine, hip, and wrist.
Back Pain: Back pain can result from vertebral fractures, which can lead to a loss of height and a stooped posture (kyphosis). These fractures can also cause nerve compression, leading to neurological symptoms like numbness or weakness.
Loss of Height and Stooped Posture: Vertebral fractures can result in a gradual loss of height and the development of a stooped posture. This can impact a person’s physical function and quality of life.
Bone Pain: Bone pain can occur in individuals with osteoporosis, particularly in areas where fractures have occurred or where there is significant bone loss.
Book Reference:
- Book:
This reference provides a comprehensive overview of osteoporosis, including its clinical features, diagnosis, and treatment options. It is a valuable resource for healthcare professionals and researchers interested in bone health.
Additional Notes:
- It’s important to note that not all individuals with osteoporosis experience clinical features. Many cases remain asymptomatic until a fracture occurs.
- Early diagnosis and treatment are critical for preventing fractures and maintaining bone health.
- If you are concerned about your risk of osteoporosis, consult with your healthcare provider for further evaluation and guidance.[10]
Sign & Symptoms
Sign & Symptoms of Osteoporosis
Patients with osteoporosis are asymptomatic until a fracture occurs.
Osteoporotic spinal fracture may present with;
- Acute back pain
- Gradual onset of height loss
- Sloping shoulders
- Kyphosis with chronic pain.
Acute vertebral fracture:
- It can occasionally radiate to the anterior chest or abdominal wall and mistake for a myocardial infarction or intra abdominal pathology, but worsening of pain by movement and local tenderness both suggest vertebral fracture.
Peripheral osteoporotic fractures:
- It present with local pain, tenderness and deformity, often after an episode of minimal trauma.
Hip fracture:
- The affected leg is shorten and externally rotate. [1]
Clinical Examination
Clinical Examination
While osteoporosis is often silent until a fracture occurs, a thorough clinical examination can identify risk factors, potential signs of bone loss, and associated complications.
Key Elements of the Physical Examination:
- Height Measurement: Serial height measurements can detect vertebral fractures and loss of height associated with osteoporosis.
- Posture and Gait Assessment: Kyphosis (forward curvature of the spine) and altered gait patterns may be indicative of vertebral fractures or muscle weakness.
- Palpation and Range of Motion: Tenderness over bony prominences, particularly the spine, may suggest fractures. Limited range of motion in joints may indicate associated osteoarthritis.
- Neurological Examination: Assessing balance, coordination, and muscle strength can help identify fall risk factors.
- Skin and General Examination: Examining for signs of associated conditions or secondary causes of osteoporosis, such as hyperthyroidism, Cushing’s syndrome, or malabsorption disorders.
Important Considerations:
- The clinical examination alone is not sufficient to diagnose osteoporosis. Bone mineral density (BMD) testing is essential for definitive diagnosis and fracture risk assessment.
- A comprehensive assessment should also include a detailed medical history, laboratory tests, and imaging studies as needed.
- Early detection and intervention are crucial for preventing fractures and preserving bone health.
Remember:
- It’s essential to consult with a healthcare professional for a proper evaluation and personalized recommendations for osteoporosis management.[11]
Diagnosis
Diagnosis
A doctor will consider the patient’s family history and their risk factors.
Often blood tests are use to measure i.e.;
- Calcium,
- Phosphorus,
- Vitamin D,
- Testosterone,
- Thyroid also kidney function. [4]
Levels of sex hormones and gonadotrophins should measure in men with osteoporosis and women under the age of 50.
If they suspect osteoporosis, they will request a scan, to measure bone mineral density (BMD).
Bone density scanning uses a type of x-ray technology known as dual-energy X-ray absorptiometry (in other words, DEXA) and bone densitometry.
Combined with the patient’s risk factors, DEXA can indicate the likelihood of fractures occurring due to osteoporosis.
It can also help monitor response to treatment.
Two types of device can carry out a DEXA scan:
- A central device: A hospital-based scan measures hip and spine bone mineral density while the patient lies on a table.
- A peripheral device: A mobile machine that tests bone in the wrist, heel, or finger.
DEXA test results:
The results of the test are give as a DEXA either T-score or a Z-score.
The T-score compares the patient’s bone mass with peak bone mass of a younger person.
- -1.0 or above is normal
- from -1.0 to -2.5 suggests mild bone loss
- -2.5 or below indicates osteoporosis
The Z-score compares the patient’s bone mass with that of other people with similar build and age.
The test is normally repeated every 2 years, as this allows for comparison between results.
Other tests:
- A lateral vertebral assessment (LVA) may recommend for an older patient who is more than one inch shorter than they use to, or who has back pain that is not relate to another condition.
- An ultrasound scan of the heel bone is another way to assess for osteoporosis.
It is less common than DEXA, and the measurements cannot compare against DEXA T-scores. [3]
Differential Diagnosis
Differential Diagnosis of Osteoporosis:
When diagnosing osteoporosis, it’s crucial to consider other conditions that can present with similar symptoms or radiographic findings. This helps ensure accurate diagnosis and appropriate treatment. Some of the key differential diagnoses include:
- Osteomalacia: This condition involves defective bone mineralization due to Vitamin D deficiency or other metabolic abnormalities. It can lead to bone pain and fragility, but unlike osteoporosis, bone density may be normal or even increased.
- Multiple Myeloma: This cancer affects plasma cells in the bone marrow and can cause bone pain, fractures, and elevated calcium levels. Bone lesions on X-rays may be present.
- Hyperparathyroidism: Overactive parathyroid glands can lead to increased bone resorption and elevated calcium levels. Bone pain, fractures, and kidney stones may occur.
- Metastatic Bone Disease: Cancer that spreads to the bones can weaken them and cause pain and fractures. Imaging studies can help identify the primary tumor and extent of bone involvement.
- Paget’s Disease of Bone: This condition disrupts the normal bone remodeling process, leading to enlarged and deformed bones that are prone to fractures.
- Osteogenesis Imperfecta: This genetic disorder affects collagen production and leads to fragile bones that fracture easily.[12]
Complications
Complications of Osteoporosis:
Osteoporosis, a condition characterized by decreased bone mass and increased fracture risk, can lead to several complications that significantly impact an individual’s quality of life. These complications include:
- Fractures: The most common and debilitating complication of osteoporosis, fractures can occur with minimal trauma or even spontaneously. Common fracture sites include the spine, hip, wrist, and ribs. Vertebral fractures can lead to back pain, loss of height, and spinal deformity, while hip fractures often result in prolonged hospitalization, disability, and increased mortality risk.
- Chronic Pain: Fractures and spinal deformities can cause persistent pain, limiting mobility and affecting daily activities.
- Loss of Independence: Fractures and associated pain can lead to dependence on others for basic tasks, impacting self-esteem and overall well-being.
- Reduced Quality of Life: The physical and emotional limitations associated with osteoporosis and its complications can significantly impair quality of life.
- Increased Mortality: Hip fractures, in particular, are associated with a higher risk of death within the first year after the fracture.
- Psychological Effects: Osteoporosis and its complications can contribute to anxiety, depression, and social isolation.[12]
Investigations
Investigations of Osteoporosis
Diagnosing and assessing osteoporosis involves a combination of clinical evaluation, laboratory tests, and imaging studies. These investigations help confirm the presence of osteoporosis, assess its severity, identify any underlying causes, and monitor treatment effectiveness.
Key Investigations
Bone Mineral Density (BMD) Test: This is the primary tool for diagnosing osteoporosis. It measures the amount of mineral content in your bones, usually using Dual-Energy X-ray Absorptiometry (DEXA) scan. The results are expressed as a T-score, which compares your BMD to that of a healthy young adult. A T-score of -2.5 or lower indicates osteoporosis.
Laboratory Tests: These can help identify secondary causes of osteoporosis or assess the risk of fractures. Some common tests include:
- Calcium, phosphorus, and vitamin D levels
- Thyroid function tests
- Complete blood count (CBC)
- Kidney function tests
- Liver function tests
- Parathyroid hormone levels
- Markers of bone turnover (e.g., serum C-telopeptide, procollagen type 1 N-terminal propeptide)
Imaging Studies: Besides DEXA, other imaging modalities can be used in certain situations:
- X-rays: To identify fractures or vertebral deformities.
- Vertebral Fracture Assessment (VFA): A specialized type of DEXA scan to assess vertebral fractures.
- MRI or CT: To evaluate bone structure in detail or identify other bone abnormalities.[12]
Treatment
Treatment of Osteoporosis
The Treatment recommendations are often base on an estimate of your risk of breaking a bone in the next 10 years using information such as the bone density test.
If your risk isn’t high, treatment might not include medication and might focus instead on modifying risk factors for bone loss and falls.
Biophosphonates:
For people of all genders at increased risk of fracture, the most widely prescribed osteoporosis medications are bisphosphonates.
Examples include:
- Alendronate (Binosto, Fosamax)
- Risedronate (Actonel, Atelvia)
- Ibandronate (Boniva)
- Zoledronic acid (Reclast, Zometa)
Side effects include nausea, abdominal pain and heartburn-like symptoms.
These are less likely to occur if the medicine is taken properly.
Intravenous forms of bisphosphonates don’t cause stomach upset but can cause fever, headache and muscle aches for up to three days. It might be easier to schedule a quarterly or yearly injection than to remember to take a weekly or monthly pill, but it can be more costly to do so.
Monoclonal antibody medications:
- Compared with bisphosphonates, denosumab (Prolia, Xgeva) produces similar or better bone density results and reduces the chance of all types of fractures.
- Furthermore, Denosumab is delivered via a shot under the skin every six months.
- Recent research indicates there could be a high risk of spinal column fractures after stopping the drug.
- A very rare complication of bisphosphonates and denosumab is a break or crack in the middle of the thigh bone.
- Besides this, A second rare complication is delayed healing of the jawbone (osteonecrosis of the jaw).
- Lastly, this can occur after an invasive dental procedure such as removing a tooth.
Hormone-related therapy:
- Estrogen, especially when started soon after menopause, can help maintain bone density.
- However, estrogen therapy can increase the risk of blood clots, endometrial cancer, breast cancer also possibly heart disease.
- Therefore, estrogen is typically used for bone health in younger women or in women whose menopausal symptoms also require treatment.
- Raloxifene (Evista) mimics estrogen’s beneficial effects on bone density in postmenopausal women, without some of the risks associated with estrogen.
- Taking this drug can reduce the risk of some types of breast cancer.
- Hot flashes are a common side effect.
- Raloxifene also may increase your risk of blood clots.
- In men, osteoporosis might be linked with a gradual age-related decline in testosterone levels.
- Testosterone replacement therapy can help improve symptoms of low testosterone, but osteoporosis medications have been better studied in men to treat osteoporosis and thus are recommended alone or in addition to testosterone.
Bone-building medications:
If you can’t tolerate the more common treatments for osteoporosis or if they don’t work well enough your doctor might suggest trying:
Teriparatide (Forteo):
- This powerful drug is similar to parathyroid hormone and stimulates new bone growth.
- It’s given by daily injection under the skin.
- After two years of treatment with teriparatide, another osteoporosis drug is taken to maintain the new bone growth.
Abaloparatide (Tymlos) is another drug similar to parathyroid hormone:
- You can take it for only two years, which will be followed by another osteoporosis medication.
Romosozumab (Evenity):
- Basically, this is the newest bone-building medication to treat osteoporosis.
- It is given as an injection every month at your doctor’s office.
- It is limited to one year of treatment, followed by other osteoporosis medications. [2]
Diet:
- Young adults should be encouraged to achieve normal peak bone mass by getting enough calcium (1,000 mg daily) in their diet (drinking milk or calcium-fortified orange juice and eating foods high in calcium such as salmon), performing weight-bearing exercise such as walking or aerobics (swimming is aerobic but not weight-bearing), and maintaining normal body weight.
Exercise:
- Lifestyle modification should also be incorporated into your treatment.
- Regular exercise can reduce the likelihood of bone fractures associated with osteoporosis.
- Studies show that exercises requiring muscle to pull on bones causes the bones to retain, and perhaps even gain, density.
- Researchers found that women who walk a mile a day have four to seven more years of bone in reserve than women who don’t.
- Some of the recommended exercises include weight-bearing exercise, riding stationary bicycles, using rowing machines, walking, and jogging.
- Before beginning any exercise program, make sure to review your plan with your doctor. [4]
Prevention
Prevention of Osteoporosis
Osteoporosis prevention involves a multifaceted approach aimed at building and maintaining strong bones throughout life. Key strategies include:
Adequate Calcium and Vitamin D Intake:
- Calcium is essential for bone building and maintenance. Dietary sources include dairy products, leafy green vegetables, and fortified foods.
- Vitamin D promotes calcium absorption. Sunlight exposure, fatty fish, and fortified foods are good sources. Supplements may be necessary if dietary intake is insufficient.
Regular Weight-Bearing and Muscle-Strengthening Exercise:
- Activities like walking, jogging, dancing, and weightlifting help stimulate bone growth and improve muscle strength and balance, reducing the risk of falls.
Healthy Lifestyle Choices:
- Avoid smoking and excessive alcohol consumption, as these can negatively impact bone health.
- Maintain a healthy weight, as being underweight increases fracture risk.
Fall Prevention:
- Make your home safer by removing tripping hazards and installing grab bars.
- Consider balance and strength training exercises to reduce fall risk.
Medication:
- For individuals at high risk, medications like bisphosphonates, denosumab, or hormone replacement therapy may be recommended to slow bone loss or promote bone growth.[13]
This comprehensive textbook provides in-depth information on osteoporosis prevention, diagnosis, and treatment, including the latest research and clinical guidelines.
Remember, prevention is key in managing osteoporosis. Starting early and adopting healthy habits can help maintain strong bones and reduce fracture risk throughout life. It’s also important to consult your healthcare provider for personalized advice and risk assessment.
Homeopathic Treatment
Homoeopathic Treatment for Osteoporosis
Calcarea Phosphorica:
- Excellent remedy in homeopathic treatment especially for Osteoporosis where there is excess curvature of spine.
- Patient has weakness also brittleness of bones and is unable to appropriately support the body leading to bending of bones.
Calcarea Fluorica:
- Of use in homeopathic treatment for Osteoporosis by promoting calcium absorption in the body.
- Cracking specifically in the joints.
- Easy dislocations of joints.
- Enlargements of bone either with or without caries, particularly of traumatic origin.
- Has got action on long bones.
Silicea:
- Especially suited in homeopathic treatment for Osteoporosis to people who have a fragile appearance and weak spine.
- Injuries and fractures take a long time to heal.
Symphytum:
- Of great use in the healing process when fractures occur.
- It strengthens the bones and takes care of the pain in old fractures that have healed. [5]
Ruta Graveolens:
- It is yet another very effective homeopathic cure used for the treatment of fractures in osteoporosis.
- Whenever a bone gets broken, the ligaments and tendons of bones that surround it additionally get harmed.
- This regular solution helps in mending torn ligaments and tendons.
Diet & Regimen
Diet & Regimen of Osteoporosis
A balanced diet and healthy lifestyle play a crucial role in managing and preventing osteoporosis. Key recommendations include:
Diet:
- Adequate Calcium Intake: Consume calcium-rich foods like dairy products (milk, yogurt, cheese), leafy green vegetables, fortified foods, and calcium supplements if needed. The recommended daily intake varies depending on age and gender.
- Sufficient Vitamin D: Ensure adequate sun exposure (15-20 minutes daily) and consume Vitamin D-rich foods like fatty fish, egg yolks, and fortified foods. Vitamin D supplements may be necessary, especially in individuals with limited sun exposure or those at risk of deficiency.
- Protein: Include adequate protein in the diet to support muscle mass and bone health. Good sources include lean meats, poultry, fish, beans, lentils, and eggs.
- Fruits and Vegetables: Consume a variety of fruits and vegetables for essential nutrients and antioxidants that contribute to overall health and bone health.
- Limit Sodium and Caffeine: Excessive sodium intake can increase calcium excretion, while caffeine can interfere with calcium absorption. Moderation is key.
- Avoid Excessive Alcohol: Excessive alcohol consumption can negatively impact bone health and increase the risk of fractures.
Regimen:
- Weight-bearing and Muscle-strengthening Exercises: Engage in regular physical activity, including weight-bearing exercises (walking, jogging, dancing) and muscle-strengthening exercises (resistance training, yoga) to improve bone density and muscle strength.
- Fall Prevention: Take measures to prevent falls, such as removing tripping hazards, using assistive devices if needed, and improving balance and coordination through exercise.
- Smoking Cessation: Smoking weakens bones and increases the risk of fractures. Quitting smoking is crucial for bone health.
- Medications: In some cases, medications may be prescribed to treat osteoporosis and reduce fracture risk. Consult a healthcare professional for appropriate medication options.[12]
Do’s and Don'ts
DO’s:
Related to Diet:
- Consume Calcium-rich foods: Include dairy products, leafy greens, fortified foods, and consider supplements if needed.
- Get enough Vitamin D: Spend time in the sun, eat fatty fish, egg yolks, fortified foods, and consider supplements.
- Eat adequate Protein: Choose lean meats, fish, beans, lentils, and eggs for muscle and bone support.
- Include Fruits and Vegetables: Enjoy a variety for essential nutrients and antioxidants.
- Limit Sodium and Caffeine: Moderation is key to avoid hindering calcium absorption and increasing excretion.
Exercise & Lifestyle:
- Engage in Weight-bearing exercises: Walking, jogging, dancing help maintain bone density.
- Do Muscle-strengthening exercises: Include resistance training and yoga for bone and muscle health.
- Take Fall prevention measures: Remove tripping hazards, use assistive devices if needed, and improve balance through exercise.
- Quit Smoking: Smoking weakens bones and increases fracture risk.
- Limit Alcohol intake: Excessive alcohol can negatively affect bone health.
Medical:
- Consult your doctor: Get regular bone density checks and discuss medications if needed.
- Take prescribed medications: Follow your doctor’s instructions for osteoporosis medications.
DON’Ts:
Related To Diet:
- Don’t consume excessive sodium: It can increase calcium excretion.
- Avoid drink too much caffeine: It can interfere with calcium absorption.
- Don’t consume excessive alcohol: It negatively impacts bone health.
Exercise & Lifestyle:
- Avoid High-impact exercises: Activities like jumping and running can lead to fractures.
- Avoid Jerky, rapid movements: Choose exercises with slow, controlled motions.
- Not Bending and twisting: These motions can increase the risk of spinal fractures.
- Don’t smoke: It weakens bones and increases fracture risk.
Other:
- Don’t ignore symptoms: Consult your doctor if you experience bone pain or loss of height.
Remember:
- It’s essential to consult with your healthcare professional for personalized guidance on diet, exercise, and medication management based on your individual needs and risk factors.
- Making these lifestyle changes and following medical advice can help improve bone health, reduce fracture risk, and enhance your overall quality of life with osteoporosis.
Terminology
Terminology of Osteoporosis
- Osteoporosis: A condition characterized by decreased bone mass and density, leading to increased bone fragility and fracture risk.
- Bone Mineral Density (BMD): A measurement of the amount of mineral content in bone tissue, often used to assess bone health and diagnose osteoporosis.
- T-score: A standardized score comparing an individual’s BMD to that of a healthy young adult of the same sex. A T-score of -2.5 or lower indicates osteoporosis.
- Z-score: A standardized score comparing an individual’s BMD to that of others in the same age group and sex. It helps identify secondary causes of bone loss.
- Osteopenia: A condition where bone mineral density is lower than normal but not low enough to be classified as osteoporosis. It represents an increased risk of developing osteoporosis.
Fracture: A break in the continuity of a bone.
Vertebral Fracture: A fracture in one or more of the bones in the spine (vertebrae).
- Hip Fracture: A fracture in the upper part of the femur (thigh bone).
- Fragility Fracture: A fracture that occurs with minimal trauma, often indicative of underlying bone fragility.
- Dual-Energy X-ray Absorptiometry (DXA or DEXA): An imaging technique used to measure bone mineral density and diagnose osteoporosis.
- Osteoblast: A cell responsible for bone formation.
- Osteoclast: A cell responsible for bone resorption (breakdown).
- Bone Remodeling: The continuous process of bone breakdown by osteoclasts and bone formation by osteoblasts.
- Calcium: An essential mineral for bone health and other bodily functions.
Vitamin D: A nutrient crucial for calcium absorption and bone health.
- Estrogen: A hormone that plays a role in maintaining bone density, especially in women.
- Menopause: The cessation of menstrual periods in women, associated with decreased estrogen levels and increased risk of osteoporosis.
- Antiresorptive Medications: Drugs that slow down bone resorption by osteoclasts, helping to maintain bone density.
- Anabolic Medications: Drugs that stimulate bone formation by osteoblasts, increasing bone mass.
- Fall Prevention: Strategies to reduce the risk of falls and fractures, including exercise, home modifications, and assistive devices.
References
References
- Davidson’s Principles and Practice of Medicine (22nd edition)
- https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
- https://www.medicalnewstoday.com/articles/155646.php
- https://www.emedicinehealth.com/osteoporosis/article_em.htm#are_there_home_remedies_for_osteoporosis
- https://www.womenshealth.gov/a-z-topics/osteoporosis
- Prevalence of osteoporosis in India: an observation of 31238 adults, 2022.
- Prevalence of osteoporosis in India, 2022.
- Osteoporosis: Pathophysiology and Clinical Management, 4th Edition, Clifford J. Rosen and Stuart H. Ralston, 2019, Elsevier.
- Kelley’s Textbook of Rheumatology, 11th Edition, Edited by Gary S. Firestein, Ralph C. Budd, Sherine E. Gabriel, Iain B. McInnes, and Josef S. Smolen, 2021, Elsevier.
- Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism, 9th Edition, Clifford J. Rosen (Editor), 2013, American Society for Bone and Mineral Research.
- Harrison’s Principles of Internal Medicine, 21st Edition, Dennis L. Kasper, Anthony S. Fauci, Stephen L. Hauser, Dan L. Longo, J. Larry Jameson, Joseph Loscalzo,2022, McGraw-Hill Education.
- Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism, 9th Edition,Clifford J. Rosen, Shonni J. Silverberg, John P. Bilezikian, and Michael P. Whyte, 2019, John Wiley & Sons.
- Osteoporosis, 5th Edition, David A. Hanley, Robert G. Josse, and Ego Seeman, 2020, Elsevier.
Also Search As
Osteoporosis Also Search As
People can search for homeopathic articles on osteoporosis using a variety of online resources and platforms. Here are some ways:
Online Search Engines:
- Use specific search terms: Type in phrases like "homeopathic treatment for osteoporosis," "homeopathy for osteoporosis," "homeopathic remedies for osteoporosis," or "homeopathic articles on osteoporosis" into search engines like Google, Bing, or DuckDuckGo.
- Refine your search: Include additional terms to focus your results, such as "research," "clinical trials," "case studies," or the names of specific homeopathic remedies.
Homeopathic Websites and Databases:
- Explore dedicated websites: Visit websites of homeopathic organizations, clinics, or journals that often feature articles on various health conditions, including osteoporosis.
- Utilize homeopathic databases: Search databases such as HomBRex or Hompath, which compile homeopathic research and clinical information.
- Consult online homeopathic forums: Participate in online communities and forums dedicated to homeopathy to exchange information and seek advice.
Social Media:
- Follow relevant groups and pages: Join homeopathy-related groups or follow pages on social media platforms like Facebook, Twitter, or Instagram to stay updated on the latest news and research.
- Use hashtags: Search for hashtags like #homeopathy, #osteoporosis, or #naturalremedies on social media to discover related content.
Libraries and Bookstores:
- Browse physical books and journals: Visit your local library or bookstore and look for books or journals on homeopathy that may contain information about osteoporosis.
- Utilize online library resources: Many libraries offer access to online databases and journals that may include homeopathic research articles.
Consult a Homeopathic Practitioner:
- Seek professional guidance: If you are considering homeopathic treatment for osteoporosis, consult with a qualified homeopathic practitioner who can provide personalized recommendations and information based on your individual needs and medical history.
Tips:
- Be critical of sources: Evaluate the credibility and reliability of the information you find. Look for evidence-based research, peer-reviewed articles, and reputable sources.
- Consider consulting a conventional doctor as well: Homeopathy can be used as a complementary therapy alongside conventional medical treatment. Discuss your interest in homeopathy with your doctor to ensure safe and effective treatment for your osteoporosis.
Remember, finding reliable and evidence-based information is crucial when exploring any treatment options, including homeopathy. Use a variety of sources, be critical of the information you find, and always consult with qualified healthcare professionals.
Frequently Asked Questions (FAQ)
What is Osteoporosis?
Osteoporosis is a disease characterized by low bone mass and loss of bone tissue that may lead to weak and fragile bones.
What causes Osteoporosis?
- Calcium intake is not sufficient
- Body does not absorb enough calcium from the diet
- Lack of certain hormones (estrogen)
- They may contribute to bone loss
- Inadequate intake of calcium & vitamin D
- Lack of weight-bearing exercise
- Overuse of corticosteroids
- Thyroid problems
- Lack of muscle use
- Bone cancer
How is osteoporosis treated?
Treatment involves lifestyle changes like increasing calcium and vitamin D intake, regular exercise, and fall prevention strategies. Medications may also be prescribed to slow bone loss or stimulate new bone growth.
How is osteoporosis diagnosed?
The primary diagnostic tool is a bone mineral density test (BMD), usually done with a dual-energy X-ray absorptiometry (DXA) scan.
Can homeopathy help with osteoporosis?
Homeopathy aims to stimulate the body’s self-healing abilities and may offer supportive treatment for osteoporosis alongside conventional approaches.
What are the symptoms of Osteoporosis?
Symptoms
- Acute back pain
- Gradual onset of height loss
- Sloping shoulders
- Kyphosis with chronic pain
- Local pain, tenderness and deformity
What are the risk factors for osteoporosis?
Risk factors include age, gender (women are more susceptible), family history, low calcium intake, vitamin D deficiency, sedentary lifestyle, smoking, and excessive alcohol consumption.
Is homeopathic treatment for osteoporosis safe?
Homeopathic remedies are generally considered safe when prescribed and monitored by a qualified homeopathic practitioner.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Osteoporosis?
- Calcarea Phosphorica
- Calcarea Fluorica
- Silicea
- Symphytum
- Ruta Graveolens
