Tuberculosis
Definition
Tuberculosis (TB), which is caused by bacteria of the Mycobacterium tuberculosis complex, is one of the oldest diseases known to affect humans. [1]
There are no direct synonyms for tuberculosis, but it was historically known as:
Consumption: This term was widely used in the 19th and early 20th centuries, often associated with the wasting away of the body due to the disease.
Phthisis: This is an older medical term for tuberculosis, particularly pulmonary tuberculosis. It derives from the Greek word for "wasting away."
While these terms are not commonly used today, they may appear in historical literature or medical texts. It’s important to note that using these older terms might be considered outdated or insensitive.
Overview
Epidemiology
Causes
Types
Risk Factors
Pathogenesis
Pathophysiology
Clinical Features
Sign & Symptoms
Clinical Examination
Diagnosis
Differential Diagnosis
Complications
Investigations
Treatment
Prevention
Homeopathic Treatment
Diet & Regimen
Do’s and Don'ts
Terminology
References
Also Search As
Overview
Overview of Tuberculosis
- A major cause of death worldwide. Recent population genomic studies suggest that M. tuberculosis may have emerged ~70,000 years ago in Africa and subsequently disseminated along with anatomically modern humans, expanding globally during the Neolithic Age as human density started to increase.
- Progenitors of M. tuberculosis are likely to have 202 Section 8 Mycobacterial Diseases affected prehominids.
- This disease most often affects the lungs, although other organs are involved in up to one-third of cases.
- More than 5.7 million new cases of TB (all forms, both pulmonary and extrapulmonary) were reported to the World Health Organization (WHO) in 2013; 95% of cases were reported from developing countries. [1]
Epidemiology
Indian Epidemiology of Tuberculosis
India bears a significant burden of tuberculosis (TB). According to the WHO Global TB Report 2022, India’s TB incidence for the year 2021 was 210 per 100,000 population. This represents an 18% decline from the baseline year of 2015, surpassing the global average decline of 11%.
While progress has been made, TB remains a major public health challenge in India. The WHO also highlights that India accounted for 26% of the incident TB cases globally in 2020 and 38% of global TB deaths among HIV-negative people.
Further insights into the Indian TB epidemic can be gleaned from other sources:
- A systematic review and meta-analysis published in 2023 ("The prevalence of tuberculosis infection in India: A systematic review and meta-analysis") estimated that 31% of individuals above 15 years of age in India have latent TB infection.
- A study published in BMC Pulmonary Medicine in 2021 ("Trends in incidence and mortality of tuberculosis in India over past three decades: a joinpoint and age-period-cohort analysis") analyzed trends in TB incidence and mortality in India between 1990 and 2019. The study found a significant decreasing pattern in both incidence and mortality rates over this period.
These references, along with ongoing surveillance and research efforts, provide a comprehensive picture of the epidemiology of TB in India. They underscore the need for continued efforts to control and eliminate TB in the country.[4]
Causes
Causes
- The most common and important agent of human disease is M. tuberculosis.
Complex includes i.e.:
- M. bovis
- M. caprae
- M. africanum
- M. microti
- M. Pinni pedii
- Tuberculosis is a rod-shaped, non-spore-forming, thin aerobic bacterium measuring 0.5 μm by 3 μm.
- Another molecule in the mycobacterial cell wall, lipoarabinomannan, is involved in the pathogen–host interaction and facilitates the survival of M. tuberculosis within macrophages. [1]
Types
Types of Tuberculosis
TB is classified as pulmonary, extrapulmonary, or both.
1. Firstly, Pulmonary TB
- Pulmonary TB is conventionally categorized as primary or post primary (adult-type, secondary). pulmonary TB result from recent infection (either primary infection or reinfection) and not from reactivation.
2. Secondly, Extrapulmonary TB
- In order of frequency, the extrapulmonary sites most commonly involved in TB are the lymph nodes, pleura, genitourinary tract, bones and joints, meninges, peritoneum, and pericardium. However, virtually all organ systems may be affected.
Lymph Node TB (in other words, Tuberculous Lymphadenitis)
- The most common presentation of extrapulmonary TB in both HIV-seronegative and HIV-infected patients (35% of cases worldwide and more than 40% of cases in the United States in recent series)
- Once caused mainly by M. bovis, tuberculous lymphadenitis today is due largely to M. tuberculosis. Lymph node TB presents as painless swelling of the lymph nodes, most commonly at posterior cervical also supraclavicular sites (a condition historically referred to as scrofula).
TB of the Upper Airways
- Nearly always a complication of advanced cavitary pulmonary TB, TB of the upper airways may involve the larynx, pharynx, and epiglottis.
- Moreover, Symptoms include hoarseness, dysphonia, and dysphagia in addition to chronic productive cough. Findings depend on the site of involvement, and ulcerations may be seen on laryngoscopy.
Genitourinary TB
- Local symptoms predominate, and up to 75% of patients have chest radiographic abnormalities suggesting previous or concomitant pulmonary disease.
- Urinary frequency, dysuria, nocturia, haematuria, and flank or abdominal pain are common presentations. However, patients may be asymptomatic and their disease discovered only after severe destructive lesions of the kidneys have developed.
Skeletal TB
- In the United States, TB of the bones also joints is responsible for ~10% of extrapulmonary cases.
- In bone and joint disease, pathogenesis is related to reactivation of hematogenous foci or to spread from adjacent paravertebral lymph nodes.
- Weight-bearing joints (the spine in 40% of cases, the hips in 13%, and the knees in 10%) are most commonly affected. [1]
Risk Factors
Risk Factors of Tuberculosis
The Global Tuberculosis Report 2023 highlights various risk factors that increase an individual’s susceptibility to developing tuberculosis (TB):
Socioeconomic and Environmental Factors:
- Poverty and overcrowding: Low socioeconomic status and living in overcrowded conditions increase the risk of TB transmission.
- Undernutrition: Malnutrition weakens the immune system, making individuals more susceptible to TB infection.
- Poor ventilation: Inadequate ventilation in homes and workplaces increases the concentration of airborne TB bacteria, raising the risk of exposure.
Health-Related Conditions:
- HIV infection: People living with HIV have a significantly weakened immune system, making them highly vulnerable to TB.
- Diabetes: Diabetes impairs the immune response and increases the risk of developing active TB disease.
- Other Conditions: Smoking, alcohol abuse, and other chronic lung diseases can also increase the risk of TB.
Additional Risk Factors:
- Close contact with TB patients: Close contact with individuals with active TB, particularly those with pulmonary TB, increases the risk of infection.
- Certain occupations: Healthcare workers, miners, and people working in crowded settings are at a higher risk of TB exposure.
- Immigration from high TB burden countries: People who have immigrated from countries with high TB prevalence may have a higher risk of latent TB infection.[5]
Pathogenesis
Pathogenesis of Tuberculosis
As described in Harrison’s Principles of Internal Medicine, 21st Edition, the pathogenesis of tuberculosis (TB) involves a complex interplay between the host’s immune system and Mycobacterium tuberculosis (Mtb), the causative agent.
Key Stages:
Inhalation and Initial Infection:
- Mtb is primarily transmitted via inhalation of aerosolized droplets containing the bacteria, usually expelled by an individual with active pulmonary TB during coughing, sneezing, or speaking.
- Once inhaled, the droplets reach the alveoli of the lungs, where Mtb is phagocytosed by alveolar macrophages.
- In most cases, the macrophages are able to contain the infection, leading to latent TB infection (LTBI). However, in some individuals, the bacteria can evade the immune response and multiply, leading to active TB disease.
Primary TB:
- If the initial infection is not contained, Mtb multiplies within the macrophages, eventually causing them to rupture and release the bacteria.
- This leads to the formation of a primary focus of infection, usually in the mid or lower zones of the lungs.
- The bacteria can also spread to nearby lymph nodes, forming a Ghon complex.
Latent TB Infection (LTBI):
- In most cases, the immune system is able to contain the primary infection, leading to LTBI.
- In LTBI, the bacteria remain dormant within granulomas, which are organized collections of immune cells that wall off the infection.
- Individuals with LTBI do not have symptoms and are not contagious, but they have a lifelong risk of developing active TB disease, especially if their immune system becomes weakened.
Reactivation TB (Post-primary TB):
- Reactivation TB occurs when the dormant bacteria in LTBI become active and start multiplying, leading to active TB disease.
- This can happen years or even decades after the initial infection.
- Reactivation TB usually affects the upper lobes of the lungs, but it can also spread to other organs, such as the kidneys, bones, and meninges.
Factors Influencing Progression to Active TB:
- Weakened immune system: HIV infection, malnutrition, diabetes, and certain medications can increase the risk of reactivation TB.
- Age: Young children and the old age person are more susceptible to developing active TB disease after infection.
- Other factors: Smoking, alcohol abuse, and chronic lung diseases can also increase the risk of progression to active TB.
Understanding the pathogenesis of TB is crucial for developing effective prevention and treatment strategies. By targeting key stages in the disease process, we can reduce the burden of TB and move closer to achieving the global goal of ending TB.[1]
Pathophysiology
Pathophysiology
From exposure to infection
- In general, Tuberculosis is most commonly transmitted from a person with infectious pulmonary TB by droplet nuclei, which are aerosolized by coughing, sneezing, or speaking.
- Furthermore, The tiny droplets dry rapidly; the smallest (<5-10 μm in diameter) may remain suspended in the air for several hours and may reach the terminal air passages when inhaled.
- There may be as many as 3000 infectious nuclei per cough.
- Besides this, Age is an important determinant of the risk of disease after infection.
- Among infected persons, the incidence of TB is highest during late adolescence and early adulthood; additionally the reasons are unclear.
- Lastly, The incidence among women peaks at 25–34 years of age. [1]
Clinical Features
Clinical Features of Tuberculosis
As detailed in Kumar & Clark’s Clinical Medicine, 10th Edition, the clinical features of tuberculosis (TB) can vary depending on the site of infection and the stage of the disease.
Pulmonary TB (Most Common):
Symptoms:
- Chronic cough: Often lasting more than 3 weeks, may be productive of sputum (phlegm) which can be blood-streaked.
- Chest pain: Can be pleuritic (sharp pain on breathing) or a dull ache.
- Fatigue and malaise: Feeling tired and unwell.
- Weight loss and loss of appetite: Unexplained weight loss and reduced desire to eat.
- Fever: Often low-grade, especially in the evenings (night sweats).
- Haemoptysis: Coughing up blood (can be a sign of advanced disease).
Signs:
- Crackles on auscultation: Abnormal lung sounds heard with a stethoscope.
- Dullness to percussion: Reduced resonance over affected areas of the lung.
- Lymphadenopathy: Enlarged lymph nodes, especially in the neck.
Extrapulmonary TB:
TB can affect any organ in the body. The clinical features will depend on the specific site of infection. Some common examples include:
- TB lymphadenitis: Swollen lymph nodes, usually in the neck.
- TB meningitis: Headache, fever, neck stiffness, altered mental status.
- Genitourinary TB: Abdominal pain, urinary symptoms, infertility.
- Skeletal TB: Bone pain, joint swelling, back pain (Pott’s disease).
General Symptoms (Can be present in both pulmonary and extrapulmonary TB):
- Fever: Often low-grade.
- Night sweats: Profuse sweating during sleep.
- Weight loss: Unexplained loss of weight.
- Fatigue: Feeling tired and weak.
- Loss of appetite: Reduced desire to eat.
Important Notes:
- TB can present with a wide range of symptoms, and the presentation can be subtle, especially in the early stages.
- A high index of suspicion is needed, particularly in individuals with risk factors for TB.
- Early diagnosis and treatment are essential to prevent complications and reduce transmission.[6]
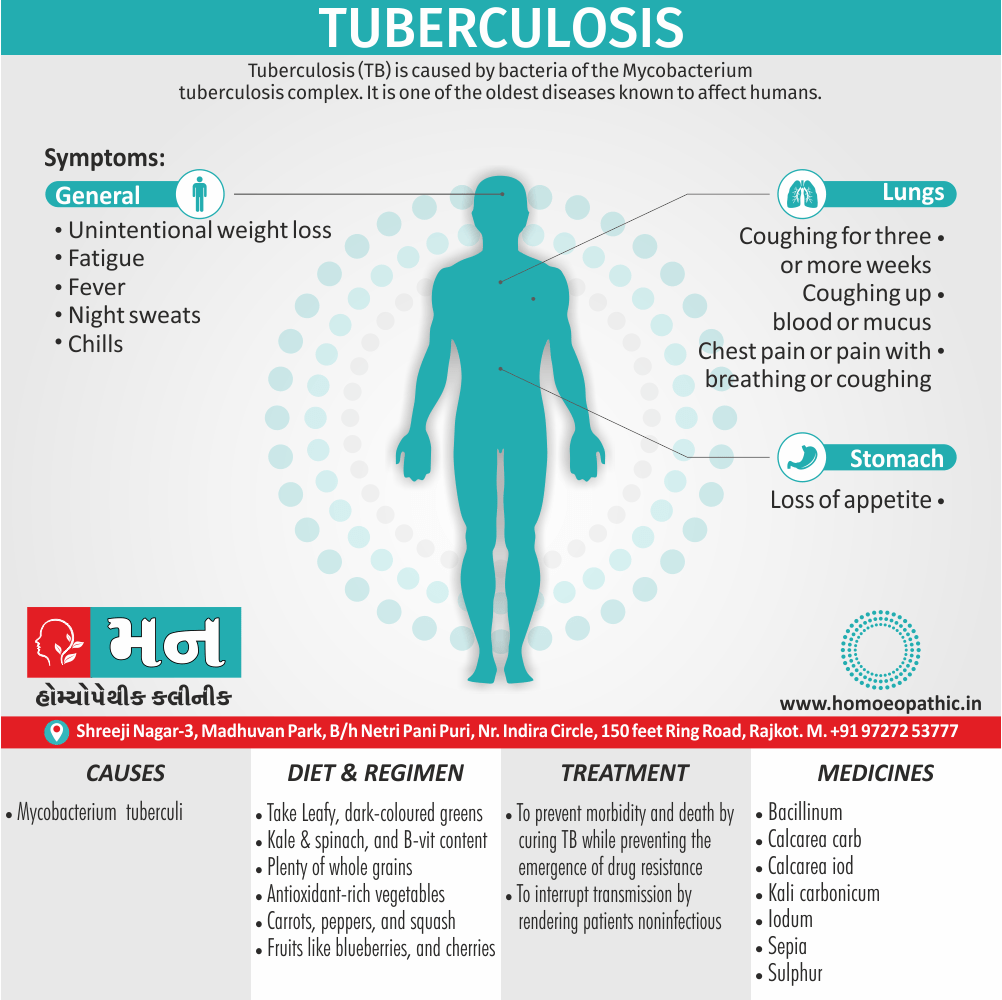
Sign & Symptoms
Sign & Symptoms of Tuberculosis
- Coughing for either three or more weeks
- Coughing up either blood or mucus
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue
- Fever
- Night sweats
- Chills
- Loss of appetite
- Tuberculosis can also affect other parts of your body, including the kidneys, spine or brain.
- When TB occurs outside your lungs, signs and symptoms vary according to the organs involved.
- For example, tuberculosis of the spine might cause back pain, and tuberculosis in your kidneys might cause blood in your urine. [1]
Clinical Examination
Clinical Examination of Tuberculosis
Systemic Symptoms:
- Fever (often low-grade and intermittent)
- Night sweats
- Fatigue
- Weight loss
- Anorexia
Respiratory Symptoms:
- Cough (initially dry, later productive of sputum)
- Hemoptysis (coughing up blood)
- Chest pain
- Shortness of breath
Physical Examination Findings:
Pulmonary:
- Dullness to percussion over affected areas
- Reduced breath sounds
- Crackles (rales)
- Wheezing (less common)
Extrapulmonary:
- Lymphadenopathy (enlarged lymph nodes)
- Hepatosplenomegaly (enlarged liver and spleen)
- Skin manifestations (e.g., erythema nodosum)
- Meningitis (in TB meningitis)
Important Considerations:
History:
- Exposure to individuals with TB
- Travel to areas with high TB prevalence
- Previous TB infection or treatment
- Immunosuppression (e.g., HIV infection)
- Other medical conditions
Investigations:
- Chest X-ray
- Sputum smear microscopy and culture
- Tuberculin skin test (TST) or interferon-gamma release assay (IGRA)
- Other imaging studies (e.g., CT scan) or biopsies may be needed depending on the site of involvement.
Disclaimer:
- The information provided here is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment.
- The clinical presentation of tuberculosis can be variable. This information reflects common findings but may not encompass all possible manifestations.[7]
Diagnosis
Diagnosis
- Classic chest radiograph showing upper-lobe infiltrates with cavities
- On the other hand, the diagnosis can easily be missed in an older people nursing home resident or a teenager with a focal infiltrate.
- AFB Microscopy
- Nucleic Acid Amplification Technology
- Mycobacterial Culture
- Drug Susceptibility Testing
- Radiographic Procedures
- Tuberculin Skin Testing
- IFN-γ Release Assays [1]
Differential Diagnosis
Differential Diagnoses of Tuberculosis
Respiratory:
- Infections:
- Pneumonia (bacterial, viral, fungal)
- Lung abscess
- Bronchiectasis
- Histoplasmosis
- Coccidioidomycosis
- Aspergillosis
- Malignancies:
- Lung cancer
- Lymphoma
- Other:
- Sarcoidosis
- Wegener’s granulomatosis
- Pulmonary embolism
- Chronic obstructive pulmonary disease (COPD)
Extrapulmonary:
- Depending on site of involvement:
- Lymphadenitis (other infectious or malignant causes)
- Meningitis (bacterial, viral, fungal)
- Peritonitis (bacterial, fungal)
- Bone and joint infections
- Crohn’s disease
- Systemic lupus erythematosus (SLE)
Note:
- The differential diagnoses can vary depending on the clinical presentation and site of involvement.
- It is important to consider other conditions that can mimic tuberculosis, especially in individuals with risk factors or atypical presentations.[7]
Complications
Complications of Tuberculosis
- TB may cause persisting pulmonary damage in patients whose infection has been considered cured on clinical grounds.
- Chronic impairment especially of lung functions, bronchiectasis, aspergillomas, and chronic pulmonary aspergillosis (CPA) have been associated with TB. [1]
Investigations
Investigations of Tuberculosis
Microbiological Investigations:
- Sputum smear microscopy:
- Ziehl-Neelsen stain to identify acid-fast bacilli (AFB)
- Fluorescence microscopy may be used for increased sensitivity
- Sputum culture:
- Gold standard for diagnosis
- Liquid and solid media used
- Can take several weeks for results
- Allows for drug susceptibility testing
- Nucleic acid amplification tests (NAATs):
- Rapid detection of Mycobacterium tuberculosis complex
- Can also detect rifampicin resistance
- May be performed on sputum or other specimens
Imaging:
- Chest X-ray:
- Initial imaging modality
- Can show infiltrates, cavities, pleural effusions, or hilar lymphadenopathy
- CT scan:
- More detailed assessment of lung parenchyma and mediastinum
- May be used for further evaluation or to guide procedures
Immunological Tests:
- Tuberculin skin test (TST):
- Measures delayed-type hypersensitivity response to tuberculin
- Positive result indicates exposure to M. tuberculosis
- Can be falsely positive or negative in certain situations
- Interferon-gamma release assays (IGRAs):
- Measure T-cell response to M. tuberculosis antigens
- More specific than TST
- Less affected by prior BCG vaccination
Other Investigations:
- Blood tests:
- Complete blood count (CBC)
- Erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP)
- HIV testing
- Other specimens:
- Depending on site of involvement:
- Pleural fluid, cerebrospinal fluid (CSF), urine, lymph node biopsy, etc.
- May be sent for microscopy, culture, and/or NAAT.[7]
- Depending on site of involvement:
Treatment
Treatment of Tuberculosis
The two aims of TB treatment are i.e.:
(1) Firstly, To prevent morbidity and death by curing TB while preventing the emergence of drug resistance
(2) Secondly, To interrupt transmission by rendering patients non infectious. Chemotherapy for TB became possible with the discovery of streptomycin in 1943.
- Administration of streptomycin to patients with chronic TB reduced mortality rates also led to cure in the majority of cases.
- DRUGS Four major drugs are considered first-line agents for the treatment of TB: for example isoniazid, rifampicin, pyrazinamide, and ethambutol
(1) The fluoroquinolone antibiotics
(2) The injectable aminoglycosides kanamycin, amikacin, also streptomycin
(3) The injectable polypeptide capreomycin; also the oral agents
(4) Ethionamide also prothionamide
(5) Cycloserine also terizidone (therizidone)
(6) PAS. [1]
Prevention
Prevention of Tuberculosis
- The best way to prevent TB is to diagnose and isolate infectious cases rapidly and to administer appropriate treatment until patients are rendered non infectious (usually 2–4 weeks after the start of proper treatment) and the disease is cured.
- Additional strategies include BCG vaccination and treatment of persons with LTBI who are at high risk of developing active disease.
- BCG Vaccination
- BCG was derived from an attenuated strain of M. bovis and was first administered to humans in 1921. [1]
Homeopathic Treatment
Homeopathic Treatment of Tuberculosis
Homeopathy treats the person as a whole. It means that homeopathic treatment focuses on the patient as a person, as well as his pathological condition. The homeopathic medicines selected after a full individualizing examination and case-analysis.
which includes
- The medical history of the patient,
- Physical and mental constitution,
- Family history,
- Presenting symptoms,
- Underlying pathology,
- Possible causative factors etc.
A miasmatic tendency (predisposition/susceptibility) also often taken into account for the treatment of chronic conditions.
What Homoeopathic doctors do?
A homeopathy doctor tries to treat more than just the presenting symptoms. The focus is usually on what caused the disease condition? Why ‘this patient’ is sick ‘this way’?.
The disease diagnosis is important but in homeopathy, the cause of disease not just probed to the level of bacteria and viruses. Other factors like mental, emotional and physical stress that could predispose a person to illness also looked for. No a days, even modern medicine also considers a large number of diseases as psychosomatic. The correct homeopathy remedy tries to correct this disease predisposition.
The focus is not on curing the disease but to cure the person who is sick, to restore the health. If a disease pathology not very advanced, homeopathy remedies do give a hope for cure but even in incurable cases, the quality of life can greatly improved with homeopathic medicines.
Homeopathic Medicines for Tuberculosis:
The homeopathic remedies (medicines) given below indicate the therapeutic affinity but this is not a complete and definite guide to the homeopathy treatment of this condition. The symptoms listed against each homeopathic remedy may not be directly related to this disease because in homeopathy general symptoms and constitutional indications also taken into account for selecting a remedy.
Medicines:
Bacillinum:
- Bacillinum has been employed successfully in the treatment of tuberculosis.
- Besides this, Its good effects are seen in the change of sputum, which becomes decreased, more aerated and less purulent.
- It will relieve congestion of the lungs, thus paving the way for other remedies in tuberculosis.
- In other words, this is an excellent first stage attack for this disease, to be followed by one of the following remedies.
- Calcarea carb:
- Extreme Dyspnoea. Suffocating spells, tightness, burning and soreness in chest.
- Chest very sensitive to touch, percussion or pressure. Longing for fresh air. Bloody expectoration. Sneezing (pain in head and nape).
- Worse – going upstairs or slightest ascent; from mental or physical exertion, cold in every form; water, washing, moist air, wet weather; during full moon; standing.
- Better – dry climate; especially lying on painful side.
- Kali carb:
- Pains are sharp and cutting, also come from within out, with a stinging characteristic.
- Whole chest very sensitive; leaning forward relieves chest symptoms.
- Expectoration must be swallowed; cheesy taste; copious offensive lump. Wheezing.
- Coldness of chest. Tendency to tuberculosis.
- Worse – cold weather; from soup and coffee; around 3 am. Lying on left side; and lying on painful side. On the other hand Better – warm weather, though moist; during the day; while moving about.
Iodum:
- Difficult expansion of chest, blood-streaked sputum; internal dry heat, external coldness.
- Inspiration difficult. Croupy cough with difficult respiration; wheezy.
- Cold extends downwards from head to throat and bronchi. Besides this, Great weakness about chest.
- Palpitation from the least exertion. Iodum cough.
Phellandrinum:
- Respiratory remedy. Good remedy specifically for offensive expectoration and cough phthisis.
- Tuberculosis, affecting generally the middle lobes. Everything tastes sweet.
- Dyspnoea and continuous cough early in morning. Cough, with profuse also fetid expectoration; compels him to sit up. Hoarseness.
Stannum:
- Very marked debility especially of chronic bronchial and pulmonary conditions, characterised by profuse muco-purulent discharges upon tuberculosis basis.
- Talking causes a very weak feeling in the throat and chest. Pains come also go gradually.
- Mucous expelled especially by forcible cough. Violent, dry cough in evening until midnight.
Sulphur:
- Oppression and burning sensation in chest. Additionally, Difficult respiration; wants windows open.
- Loose cough; aggravation specifically in talking, morning. Greenish, purulent, sweetish expectoration, Much rattling of mucous.
- Stitching pains shooting through back aggravation lying on back, breathing deeply. Oppression, as of a load on chest.
- Dyspnoea in middle of night, relieved especially by sitting up. Lastly, Pulse more rapid in morning.
- Calcarea Iod:
- This remedy is preferable, when glandular complications are present, in young subjects who grow rapidly with tickling, teasing cough, rapid pulse, high fever, and rapid hepatization.
- It corresponds more exactly to the miliary form of tuberculosis.
Sepia:
- Hirschel claims that this remedy stands next to Calcarea in dry, fatiguing, tickling coughs.
Diet & Regimen
Diet and Regiment
For Tuberculosis
Diet:
- Focus on nutrient-dense foods:
- Protein: Essential for tissue repair and immune function. Include lean meats, poultry, fish, eggs, dairy products, beans, lentils, nuts, and seeds.
- Complex carbohydrates: Provide energy. Opt for whole grains like brown rice, quinoa, oats, and whole wheat bread.
- Healthy fats: Support the absorption of fat-soluble vitamins. Include avocados, nuts, seeds, and olive oil.
- Fruits and vegetables: Rich in vitamins, minerals, and antioxidants. Aim for a variety of colorful options.
- Protein: Essential for tissue repair and immune function. Include lean meats, poultry, fish, eggs, dairy products, beans, lentils, nuts, and seeds.
- Micronutrients:
- Vitamin C: Boosts immunity. Found in citrus fruits, berries, and leafy greens.
- Vitamin D: Aids in calcium absorption and immune function. Get sunlight exposure or consider supplements.
- Zinc: Important for wound healing and immune response. Found in nuts, seeds, and lean meats.
- Iron: Helps carry oxygen in the blood. Include iron-rich foods like red meat, spinach, and beans.
- Vitamin C: Boosts immunity. Found in citrus fruits, berries, and leafy greens.
- Hydration: Drink plenty of water to stay hydrated and support overall health.
Foods to Avoid:
- Processed foods: High in unhealthy fats, sugar, and sodium.
- Sugary drinks: Can contribute to weight gain and other health problems.
- Alcohol: May interfere with medications and weaken the immune system.
- Caffeine: Can interfere with sleep and increase anxiety.
Regimen:
- Medication adherence: Strictly follow the prescribed medication regimen as directed by your doctor. This is crucial for successful treatment.
- Rest: Get adequate rest to allow your body to heal.
- Hygiene: Practice good hygiene, including covering your mouth and nose when coughing or sneezing, to prevent the spread of TB bacteria.
- Regular check-ups: Attend all scheduled appointments with your doctor to monitor your progress and address any concerns.
- Support: Seek emotional support from family, friends, or support groups. Dealing with TB can be challenging, and having a support system can make a difference.
Do’s and Don'ts
Do’s and Don’ts of Tuberculosis
Tuberculosis Do’s & Don’ts
Do’s:
- Seek medical attention: If you experience symptoms like persistent cough, fever, night sweats, or unexplained weight loss, consult a doctor promptly. Early diagnosis and treatment are critical for TB management.
- Adhere to treatment: Strictly follow the prescribed medication regimen. Complete the full course of treatment, even if you start feeling better. Skipping doses or stopping treatment early can lead to drug resistance and relapse.
- Practice good hygiene: Cover your mouth and nose with a tissue when coughing or sneezing. Dispose of used tissues properly in a sealed bag. Wash your hands frequently with soap and water.
- Isolate yourself: If you have active TB, stay at home and avoid close contact with others, especially vulnerable individuals, until your doctor confirms you are no longer contagious.
- Wear a mask: When around others, wear a well-fitting mask to prevent the spread of TB bacteria through the air.
- Maintain a healthy lifestyle: Eat a balanced diet, get adequate rest, and avoid smoking and excessive alcohol consumption to boost your immune system.
- Attend follow-up appointments: Regularly visit your doctor for checkups and monitoring during and after treatment.
Don’ts:
- Ignore symptoms: Don’t dismiss persistent cough or other TB symptoms. Seek medical advice to rule out TB or other conditions.
- Dont self-medicate: Don’t attempt to treat TB with over-the-counter medications or home remedies. Consult a doctor for proper diagnosis and treatment.
- Stop treatment prematurely: Don’t discontinue treatment without your doctor’s approval, even if you feel better. Incomplete treatment can lead to complications and drug resistance.
- Spread the infection: If you have active TB, avoid close contact with others, especially in enclosed spaces, until you are no longer contagious.
- Dint share personal items: Don’t share utensils, towels, or other personal items with others to prevent the spread of TB bacteria.
- Smoke or use tobacco products: Smoking weakens the lungs and increases the risk of complications from TB.
- Consume excessive alcohol: Alcohol can interact with TB medications and impair your immune system.
Remember, TB is a treatable disease. Following these do’s and don’ts and working closely with your healthcare provider can help you manage the condition effectively and prevent its spread.
Terminology
Terminology
1. Acid-Fast Bacilli (AFB):
- Meaning: Bacteria (like Mycobacterium tuberculosis, the cause of TB) that resist decolorization by acids during staining procedures, making them easily identifiable under a microscope.
- Relevance: AFB presence in sputum smears is a strong indicator of TB infection.
2. Bacillus Calmette-Guérin (BCG) Vaccine:
- Meaning: A vaccine primarily used to prevent severe forms of TB in children, particularly TB meningitis.
- Relevance: While not universally used, BCG vaccination is considered in high TB prevalence areas.
3. Caseous Necrosis:
- Meaning: A type of cell death where tissues transform into a cheese-like substance, characteristic of TB granulomas.
- Relevance: This is a hallmark of TB infection and often seen on imaging studies.
4. Cavitation:
- Meaning: The formation of cavities or holes in the lungs due to tissue destruction caused by TB.
- Relevance: Cavitations can indicate advanced TB and are associated with increased infectivity.
5. Directly Observed Therapy (DOT):
- Meaning: A strategy where healthcare workers observe patients taking each dose of their TB medication.
- Relevance: DOT ensures treatment adherence, reduces drug resistance, and improves treatment success rates.
6. Extrapulmonary Tuberculosis:
- Meaning: TB infection that occurs outside the lungs, affecting organs like lymph nodes, bones, or the brain.
- Relevance: Extrapulmonary TB can be challenging to diagnose and often requires specialized treatment.
7. Granuloma:
- Meaning: A collection of immune cells that forms in response to TB infection, attempting to contain the bacteria.
- Relevance: Granulomas are a key feature of TB and can be seen on imaging studies.
8. Latent TB Infection (LTBI):
- Meaning: A state where individuals are infected with M. tuberculosis but show no symptoms and are not contagious.
- Relevance: LTBI can progress to active TB, especially in people with weakened immune systems.
9. Multidrug-Resistant TB (MDR-TB):
- Meaning: TB resistant to at least two of the most potent first-line anti-TB drugs (isoniazid and rifampicin).
- Relevance: MDR-TB requires prolonged and more complex treatment regimens.
10. Pulmonary Tuberculosis:
- Meaning: TB infection that primarily affects the lungs.
- Relevance: The most common form of TB, responsible for most transmission.
11. Sputum:
- Meaning: Mucus coughed up from the lungs.
- Relevance: Sputum samples are essential for diagnosing TB through smear microscopy and culture.
12. Tuberculin Skin Test (TST):
- Meaning: A skin test to determine if someone has been exposed to M. tuberculosis.
- Relevance: A positive TST indicates exposure, but further testing is needed to confirm active TB.
References
References
- Harrison-s_Principles_of_Internal_Medicine-_19th_Edition-_2_Volume_Set
- https://www.everydayhealth.com/tuberculosis/the-right-diet-to-beat-tuberculosis.aspx
- Homoeopathic Body-System Prescribing – A Practical Workbook of Sector Remedies.
- A systematic review and meta-analysis published in 2023 ("The prevalence of tuberculosis infection in India.
- Global Tuberculosis Report 2023, World Health Organization (WHO), 2023, World Health Organization.
- Kumar & Clark’s Clinical Medicine, 10th Edition, Parveen Kumar, Michael Clark, 2021, Elsevier.
- Davidson’s Principles and Practice of Medicine, 24th Edition, Brian R. Walker, Nicki R. Colledge, Stuart H. Ralston, Ian D. Penman, 2022, Elsevier.
Also Search As
Tuberculosis also search as
1. Online Search Engines:
- Use specific keywords:
- Combine "homeopathy" or "homeopathic" with terms like "tuberculosis," "TB," "treatment," "case studies," or "research."
- Example search queries:
- "homeopathic treatment for tuberculosis"
- "homeopathy and TB research"
- "case studies of homeopathy in tuberculosis"
- Utilize advanced search operators:
- Use quotation marks to search for exact phrases (e.g., "homeopathic remedies for TB").
- Use the minus sign to exclude specific terms (e.g., homeopathy tuberculosis -conventional medicine).
- Use the site: operator to search within specific websites (e.g., site:homeopathy.org tuberculosis).
2. Homeopathic Websites and Journals:
- Explore reputable homeopathic organizations:
- Visit websites of organizations like the National Center for Homeopathy (NCH), the American Institute of Homeopathy (AIH), or the Faculty of Homeopathy.
- These organizations often have resources, articles, or links to research on homeopathy and various conditions, including TB.
- Search homeopathic journals:
- Access online databases of homeopathic journals like "Homeopathy" or "The Journal of the American Institute of Homeopathy."
- Use their search functions to find articles specifically related to tuberculosis.
3. Online Libraries and Databases:
- Utilize academic databases:
- If you have access to academic libraries or databases, search platforms like PubMed, Google Scholar, or ScienceDirect for homeopathic research on TB.
- Filter results by publication type (e.g., articles, reviews) or date to find the most relevant and recent information.
4. Social Media and Online Forums:
- Join homeopathic communities online:
- Participate in discussions or search for information on homeopathy-focused social media groups or forums.
- Be mindful of the source and credibility of information shared in these spaces.
Tips for Effective Searching:
- Be specific: Use precise keywords and search terms to narrow down results.
- Consider alternative terms: Try synonyms or related terms (e.g., "homeopathic medicine," "nosodes," "constitutional remedies").
- Filter results: Use search engine filters or database options to refine your search by date, publication type, or language.
- Evaluate sources: Critically assess the credibility and reliability of the information you find. Look for articles published in peer-reviewed journals or from reputable organizations.
Frequently Asked Questions (FAQ)
What is Tuberculosis?
Definition
Tuberculosis (TB), which is caused by bacteria of the Mycobacterium tuberculosis complex, is one of the oldest diseases known to affect humans.
What causes Tuberculosis?
- M. tuberculosis
- M. bovis
- M. caprae
- M. africanum
- M. microti
- M. Pinni pedii
How is TB spread?
TB spreads through the air when an infected person coughs, sneezes, or speaks, releasing tiny droplets containing the bacteria.
Give the types of Tuberculosis?
- Pulmonary TB
- Extrapulmonary TB
- Lymph Node TB
- TB of the Upper Airways
- Genitourinary TB
- Skeletal TB
What is the treatment for TB?
TB is treated with a combination of antibiotics taken for several months.The specific drugs and duration of treatment depend on the type of TB and individual factors.
How is TB diagnosed?
Diagnosis
TB is diagnosed through a combination of medical history, physical examination, chest X-ray, sputum tests (smear microscopy and culture), and blood tests (such as IGRAs)
What are the symptoms of Tuberculosis?
- Coughing for three or more weeks
- Coughing up blood or mucus
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue
- Fever
- Night sweats
- Chills
- Loss of appetite
Can homeopathy cure tuberculosis (TB)?
Homeopathy aims to stimulate the body’s healing response and improve overall well-being. While there is anecdotal evidence suggesting potential benefits, it’s crucial to understand that homeopathy is not a substitute for conventional TB treatment with antibiotics.
Is it safe to use homeopathy for TB?
Homeopathic remedies are generally considered safe when used under the guidance of a qualified practitioner. However, it’s important to avoid self-treatment and inform your doctor about any homeopathic remedies you’re taking.
Homeopathic Medicines used by Homeopathic Doctors in treatment of Tuberculosis?
Homoeopathic medicines for Tuberculosis
- Bacillinum
- Calcarea carb
- Kali carb
- Iodum
- Phellandrinum
- Stannum
- Sulphur
- Calcarea Iod
- Sepia
